Copy link
Heart Sounds, Electrocardiogram, and Echocardiogram
Last updated: 02/05/2024
Key Points
- Perioperative evaluation of heart function can be achieved through cardiac auscultation, electrocardiogram (ECG) analysis, and echocardiography.
- Taken together with the overall hemodynamics, these modalities aid in the rapid assessment of the patient’s clinical status.
Heart Sounds1,2
- S1: closure of mitral valve (M1) shortly followed by tricuspid valve (T1) (Audio 1)
- S2: closure of aortic valve (A2) shortly followed by pulmonic valve (P2) (Audio 1)
- S3: “ventricular gallop” (Audio 2)
- S3 occurs in early diastole shortly after A2 due to passive rapid ventricular filling in diastole.
- It is common and benign in children, adolescents, and young adults and is considered physiologic S3 in these cases.
- After age 30, S3 is called a ventricular gallop and can be considered a sign of pathology, often due to left ventricular systolic dysfunction and congestive heart failure.
- S4: “atrial gallop” (Audio 3)
- S4 occurs in late diastole just before S1 due to active rapid ventricular filling during atrial systole.
- It is almost always abnormal and indicative of reduced ventricular compliance, often from diastolic dysfunction.
- The intensity of heart sounds increases with increasing pressure gradients across the valve.

Audio 1. Normal S1 and S2 heart sounds heard at the apex area. Source: University of Michigan Heart Sound & Murmur Library, CC BY-SA 3.0. Click here, locate and click on the icon: Link

Audio 2. S3 gallop heard at the apex area. Source: University of Michigan Heart Sound & Murmur Library, CC BY-SA 3.0. Click here, locate and click on the icon: Link

Audio 3. S4 gallop heard at the apex area. Source: University of Michigan Heart Sound & Murmur Library, CC BY-SA 3.0. Click here, locate and click on the icon: Link
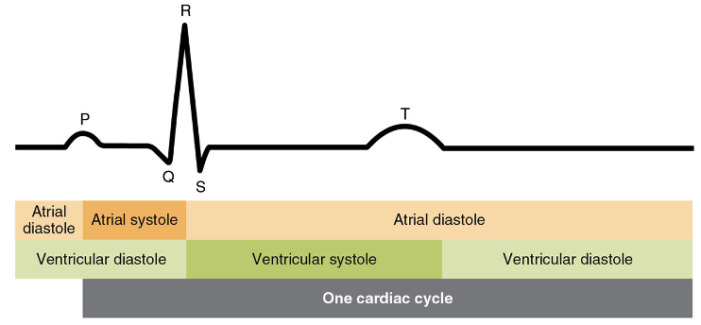
Electrocardiogram3,4
- The electrocardiogram (ECG) is a measurement of how the electrical activity of the heart changes over time. The ECG provides specific waveforms of electrical differences when the atria and ventricles depolarize and repolarize (Figure 1).
- As one of the standard American Society of Anesthesiologists monitors, intraoperative ECG monitoring can aid in the diagnosis of malignant dysrhythmias and myocardial ischemic events.
- Five lead ECGs have the advantage of monitoring for ischemic events (except for the posterior wall) over three lead systems.
- Lead II monitors the right atrium and is the most sensitive for dysrhythmias.
- Lead V5 monitors the lateral wall of the left ventricle and is the most sensitive for ischemic events.
- ST-segment depression suggests subendocardial ischemia, whereas ST-segment elevation suggests transmural myocardial ischemia.
- ST-segment depression commonly precedes ST-segment elevation.
Echocardiogram5
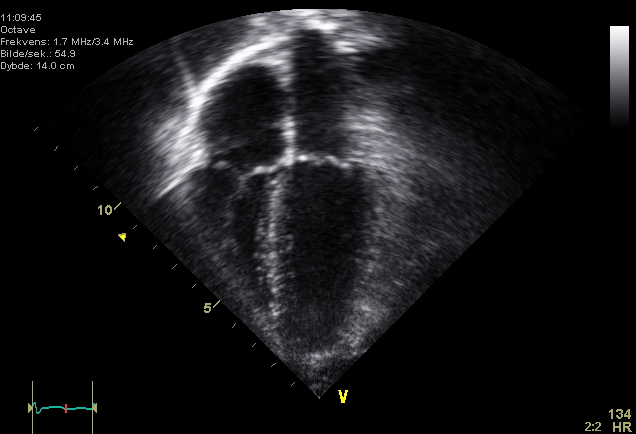
- Echocardiography is an imaging technique used in the perioperative setting for real-time evaluation of myocardial, valvular, and hemodynamic performance.
- Applications:
- Perioperative diagnosis and evaluation of heart function
- Guidance of intracardiac and intravascular catheter and device placement
- Assessment of severity of valvular pathology
- Immediate evaluation of surgical interventions such as valve repair or replacement
- Rapid diagnosis of acute hemodynamic instability and assessment of response to goal-directed therapies
- How does it work?
- Using the basic principles of ultrasound technology, echocardiography generates dynamic images of the heart from reflections of sound waves.
- The Doppler effect allows for the visualization of blood flow and measurement of velocity. Continuous wave doppler enables evaluation of high velocity flow but cannot localize the flow. Pulse wave Doppler enables evaluation of flow at a specific point.
- Echocardiography includes two main modalities:
- Transthoracic echocardiography (TTE; transducer placed on the skin)
- TTE is the most commonly used modality, but can be limited in the perioperative setting by surgical field, patient position, or patient condition (i.e., obesity, edema, surgical dressings).
- Perioperative TTE predicts postoperative cardiac events in noncardiac surgical patients at an increased clinical cardiac risk.3
- Transesophageal echocardiography (TEE; transducer placed in the esophagus)
- TEE is indicated for intraoperative monitoring during open-heart surgery, or when TTE is nondiagnostic or limited due to body habitus or other factors.
- In the operating room, TEE is useful because the probe does not interfere with the surgical field and can be utilized throughout the case for continuous real-time monitoring and evaluation of cardiac structure and function, as well as the quality of the surgical repair.
- Transthoracic echocardiography (TTE; transducer placed on the skin)
References
- Hutchins J. Blood Pressure, Heart Tones, and Diagnoses. In: Paul A. Iaizzo. Handbook of Cardiac Anatomy, Physiology, and Devices. 3rd Ed. Switzerland; Springer Cham; 2015: 307-20.
- Kusko M, Maselli K. Introduction to Cardiac Auscultation. In: Allen J. Taylor. Learning Cardiac Auscultation: From Essentials to Expert Clinical Interpretation. London; Springer London; 2015: 3-14.
- Hensley FA, Gravlee GP, Martin DE. Practical Approach to Cardiac Anesthesia. 5th Ed. Philadelphia Wolters Kluwer. Ann Arbor, Michigan. Proquest; 2014: 118-37.
- Vieau S, Iaizzo P. Basic ECG Theory, 12-Lead Recordings, and Their Interpretation. In: Paul A. Iaizzo. Handbook of Cardiac Anatomy, Physiology, and Devices. 3rd Ed. Switzerland; Springer Cham; 2015: 321-34.
- Perrino Jr. A, Popescu W, Jadbabaie F, Skubas N. Echocardiography. In: Paul G. Barash et al. Clinical Anesthesia. 8th Ed. Philadelphia; Wolters Kluwer; 2017: 731-766.
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.