Copy link
Graft Allocation and Recipient Selection for Liver Transplantation
Last updated: 06/26/2025
Key Points
- There is a significant mismatch between the number of patients awaiting liver transplants and the availability of suitable donor grafts.
- This scarcity of suitable grafts for transplantation necessitates an organized, multidisciplinary approach to graft allocation guided by clinical urgency and ethical considerations.
- Recipient selection involves a comprehensive medical evaluation, psychosocial assessment, and compatibility matching conducted by a multidisciplinary team.
- In the United States (US), the United Network for Organ Sharing (UNOS) systems oversees the graft allocation process.
- Ethical considerations are central to graft allocation, ensuring protection for all patients, particularly those from vulnerable populations.
Introduction
- Liver transplantation (LT) can be a life-saving intervention for patients with acute liver failure, end-stage liver disease, liver malignancies, and metabolic liver disease.1,2 However, the demand for LT far exceeds the availability of suitable grafts for donation. To address this imbalance, a systematic and equitable process of graft allocation and recipient selection is crucial.
- Donor grafts are available from deceased or living individuals. In the US, deceased donation following brain or cardiac death is predominant, while living donation is more common across parts of Asia.
- Over the past decade, the total number of liver transplants performed in the US has increased year after year. In 2024, a total of 11,458 liver transplants were performed, including 604 from living donors. Despite this, 962 patients died while on the waiting list.3
Recipient Selection
- Potential candidates are referred to a transplant center, where a comprehensive evaluation is conducted by a multidisciplinary team (Tables 1 and 2).
- Medical evaluation: Performed by hepatologists to confirm diagnosis, assess disease severity, and determine urgency
- Surgical evaluation: Assesses surgical feasibility for transplantation and includes a prior history of abdominal surgeries and anatomical considerations
- General health screening: Evaluates comorbidities that may impact perioperative risk, including cardiopulmonary and renal status
- Psychiatric assessment: Screens for mental health status, substance use history, and behavioral risk factors
- Nutritional, dental, and infectious disease evaluation: Identifies modifiable risk factors and opportunities for optimizing pre-transplant health, including vaccination needs
- Financial and social work assessment: Confirms insurance status and the presence of a support network to assist in the recovery period
- Following the evaluation, the transplant committee reviews the case to determine eligibility for listing. Periodic reassessments are conducted for those listed. Candidates denied listing may be reconsidered if modifiable conditions improve.
- Absolute contraindications include uncontrolled extrahepatic malignancy, ongoing substance abuse, and severe cardiopulmonary disease. Individual transplant centers may apply additional relative contraindications based on center policy and risk tolerance.
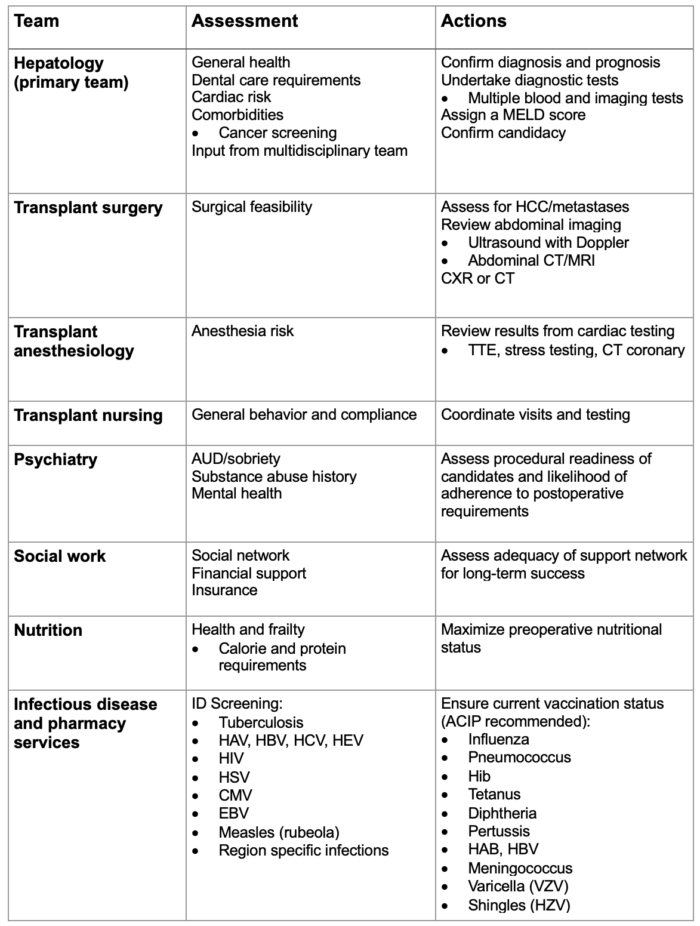
Table 1. Multidisciplinary team candidate assessment and actions undertaken before the decision to “list” on the transplant register. Abbreviations: HCC, hepatocellular carcinoma; CXR, chest x-ray; CT, computerized tomography; AUD, alcohol use disorder; ID, infectious disease; HAV, hepatitis A virus; HBV, hepatitis B virus; HCV, hepatitis C virus; HIV, human immunodeficiency virus; HSV, herpes simplex virus; CMV, cytomegalovirus; EBV, Epstein-Barr virus; ACIP, Advisory Committee on Immunization Practices; Hib, Haemophilus influenzae type b; VZV, varicella-zoster virus; HZV, herpes-zoster virus.
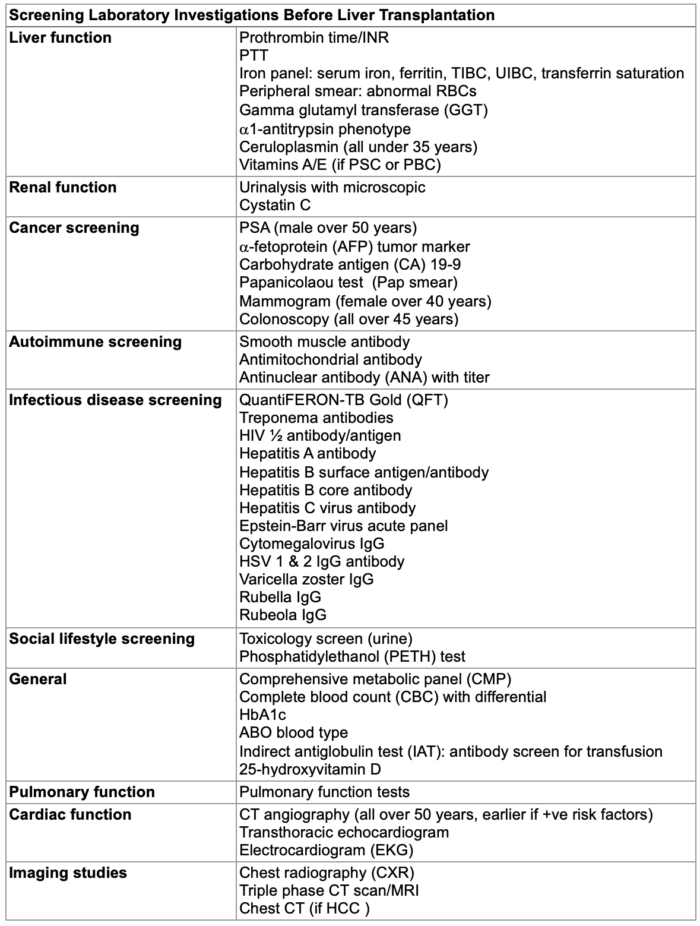
Table 2. Typical laboratory tests and investigations undertaken as part of the screening process for liver transplantation candidacy. Abbreviations: INR, international normalized ratio; PTT, partial thromboplastin time; TIBC, total iron binding capacity; UIBC, unsaturated iron binding capacity, RBC, red blood cell; PSC, primary sclerosing cholangitis; PBC, primary biliary cholangitis; PSA, prostate specific antigen; HIV, human immunodeficiency virus; IgG, immunoglobulin type G; HSV, herpes simplex virus; HbA1c, glycated hemoglobin test; CT, computed tomography; MRI, magnetic resonance imaging; HCC, hepatocellular carcinoma.
Graft Allocation Principles
- The US federal “Final Rule” policy on transplantation dictates the procedures and protocols for the allocation of grafts from deceased donors.4
- The guiding principles for graft allocation are designed to ensure fairness for all candidates while seeking to optimize the outcomes for both the graft and the recipient. They include:
- Medical urgency: Grafts are allocated to candidates based on the severity of their disease, as assessed by objective medical criteria such as the Model for End-Stage Liver Disease (MELD) scoring system for adults, the Pediatric End-Stage Liver Disease (PELD) scoring system for candidates younger than 12 years of age, or other similar versions.5 A higher MELD (or PELD) score corresponds to sicker patients and gives them timelier access to potential grafts.
- Equity: Strict medical criteria ensure an equitable distribution unaffected by age, gender, race, or socioeconomic status.
- Utility: Grafts are precious life-saving resources, and every effort is made to maximize the benefits of transplantation for potential recipients while, at the same time, avoiding futile transplants.
- Transparency: The allocation process is open to public scrutiny, and data is freely accessible.
Graft Allocation Process
- When a suitable donor graft becomes available, the local organ procurement organization (OPO) assumes responsibility for donor care and graft procurement. OPOs must be members of the Organ Procurement and Transplantation Network (OPTN), itself managed in the US by the United Network for Organ Sharing (UNOS).6 In Europe, the Eurotransplant organization plays a similar role.7
- The OPO collaborates with the donor’s family and hospital. Once authorization for donation is obtained, it works with UNOS to identify the best candidate from the list of potential recipients, while coordinating with the donor’s and recipient’s surgical teams.
- While the MELD (or PELD) score can identify sicker candidates with a more urgent need for transplantation, the final decision to allocate is influenced by other factors, such as ABO blood group and human leukocyte antigen compatibility, organ size, and logistical feasibility.1
Outcomes
- The OPTN/Scientific Registry of Transplant Recipients data for 2022 reported 9,528 liver transplants, marking a record high.
- The reported 1-year mortality following transplant was 6.8%, with 19.8% and 35.7% at the 5- and 10-year points.
- Living donor transplants demonstrated higher survival rates in both pediatric and adult populations compared to deceased donor grafts.8
- Pretransplant mortality in adult patients decreased to 12.3 deaths per 100-patient years, indicating improvements in preoperative medical care.
Current and Future Trends
- The MELD scoring system, although objective, fails to consider special conditions where a candidate’s status is more urgent than their score suggests due to the nature of their disease. Candidates with portopulmonary hypertension, hepatopulmonary syndrome, and hepatocellular carcinoma, for example, may receive additional points due to higher waiting list mortality.
- The transplant candidate population is trending older and with more comorbidities.⁹ Alcohol-associated liver disease and metabolic dysfunction-associated liver disease now dominate indications for listing in the US.
- It is recognized that the criteria for graft acceptance must be expanded to enlarge the donor graft pool. These extended donor criteria mean that older donors and donors with medical complexities that would have previously been excluded are now considered for LT. Such conditions include exposure to hepatitis B or C virus, high-risk social behaviors, and grafts donated after cardiac death.
- Machine perfusion is increasingly used to preserve grafts after procurement.
- Hypothermic machine perfusion utilizes a cold preservation solution (less than 12°C) pumped through the graft’s blood vessels to reduce metabolic activity, thereby increasing graft viability for a more extended period.
- Normothermic machine perfusion uses warmed, oxygenated, nutrient-rich perfusate (35-37°C), which keeps the graft functioning in a near-physiological metabolic state. This allows for more time for better assessment of marginal-graft viability.2
- Split-LT enables a single graft to be divided into two recipients, often benefiting pediatric or small adult recipients. Around 10% of donor livers are suitable for this technique.
- Living donor LT, already a mainstay of practice in some other parts of the world, is being promoted in an effort to provide more grafts for the donor pool.10 The benefits for the recipient include shorter waiting times, better health at the time of transplantation, and the ability to direct the graft to a chosen recipient, often a family member or friend. Living donors undergo a similar selection process to recipients to ensure safety.
References
- Ionescu VA, Diaconu CC, Bungau S, et.al. Current approaches in the allocation of liver transplantation. J Pers Med. 2022;12(10):1661. PubMed
- Lucey MR, Furuya KN, Foley DP. Liver Transplantation. N Engl J Med. 2023;389(20):1888-1900. doi:10.1056/NEJMra2200923 PubMed
- Organ Procurement and Transplantation Network. (2025). National Data: Liver. Accessed 5-30-2025 Link
- Organ Procurement and Transplantation Network, 2025, Final Rule. Accessed 5-30-2025 Link
- Wiesner R., Edwards E., Freeman R., et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003; 124(1): 91-6. PubMed
- United Network for Organ Sharing, 2025, About Us, Life Without Limits. Accessed 6-6-2025. Link
- Eurotransplant, 2025, About Eurotransplant. Accessed 6-6-2025. Link
- Jackson WE, Malamon JS, Kaplan B, et al. Survival benefit of living-donor liver transplant. JAMA Surg. 2022;157(10):926-32. PubMed
- Kwong AJ, Kim WR, Lake JR, et al. OPTN/SRTR 2022 Annual Data Report: Liver. Am J Transplant. 2024;24(2S1):S176-S265. PubMed
- Hendrickse A, Ko J, Sakai T. The care of donors and recipients in adult living donor liver transplantation. BJA Educ. 2022;22(10):387-95. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.