Copy link
Evoked Potentials: Alarm Criteria, Differential Diagnosis, and Recommendations
Last updated: 01/05/2023
Key Points
- Intraoperative neurophysiologic monitoring (IONM) is a valuable tool for improving the safety and outcome of cranial, spinal, and vascular surgery through real-time monitoring of the electrophysiologic activity of the brain, spinal cord, and peripheral nerves.1
- Anesthetic agents affect monitored signals and waveforms to variable degrees.2
- Significant changes in evoked potentials (EP) should be readily identified and reported to the surgical and anesthesia teams.1-3
Strategies to Optimize IONM
- Strategies to optimize the conditions for IONM include:1,2
- Use the lowest effective anesthetic dose
- Avoid boluses and maintain constant anesthesia level (especially during critical monitoring periods)
- Use continuous infusions (as opposed to boluses)
- Consider total intravenous anesthesia (TIVA) when possible (especially when EPs are otherwise inadequate)
- Maintain inhalational agents less than 0.5 minimum alveolar concentration (MAC)
- Use short-acting neuromuscular blocking agents (NMBA) in low doses, when/if needed
- Use opioids and other anesthetic adjuncts
- Maintain physiologic homeostasis
Warning/Alarm Criteria
- Somatosensory evoked potentials (SSEP)
- An amplitude reduction greater than 50%1
- A latency shift greater than 10%1
- Motor evoked potentials (MEP)
- An amplitude reduction greater than 80% or disappearance
- The threshold elevation at least or greater than 100V
- Morphology simplification
- MEP changes often precede changes in SSEPs
- Electromyography (EMG)
- High frequency neurotonic discharges with stretch or blunt mechanical trauma to cranial nerves or spinal roots2
- An increase in latency and/or reduction in amplitude of compound muscle action potentials (CMAP) may indicate nerve injury2
- The loss of triggered EMG responses with cranial nerve stimulation
- The threshold responses < 10mA with pedicle screw stimulation
- Electroencephalography (EEG)
- A progressive reduction in frequency and amplitude up to isoelectricity
- New asymmetry
- Seizure-like activity
- Brainstem auditory evoked potentials (BAEP)
- A 1 msec or a 10% increase in waveform component latency
- A 50% decrease in waveform component amplitude3
Differential Diagnosis and Troubleshooting
- Brief and transient signal loss (as opposed to persistent or prolonged loss of signal) is compatible with good recovery.1 This underscores the importance of recognizing and reporting signal changes, as well as the importance of identifying underlying potential causes to allow for the best possible outcome.
- When a change is noted, signal acquisition should be repeated to confirm the change (if time allows), and attention to other modalities should also be given. The surgical team, including the surgeon and anesthesiologist, should be alerted of the change as soon as it is confirmed, and troubleshooting to identify the cause should be undertaken.2 Possible causes of IONM signal change include surgical and nonsurgical reasons, as listed below.
- To determine the underlying cause, the temporal relationship between signal change and anesthesia changes (like delivering a bolus or adding an inhalational agent) or surgical manipulation (like aneurysm clipping, carotid clamping, or spinal instrumentation) should be considered. The physician should establish whether the change is focal versus global, and whether cortical versus subcortical waveforms are affected. In general, focal changes suggest surgical, technical, or positional causes, whereas global changes tend to be due to pharmacological or physiological factors.
- Optimizing oxygenation, ventilation, and perfusion (by raising blood pressure, if appropriate, and increasing the inspired oxygen concentration, may minimize potential neurological injury while investigating the cause.2
I. Surgical causes2
- Acute trauma (including blunt trauma and laceration)
- Mechanical effects including device, retractor, and pledgets
- Traction
- Compression
- Stretch injury
- Ischemia or anoxia due to vascular insufficiency and occlusion (embolism or thrombosis)
II. Nonsurgical causes include:
1. Technical issues2
- Electrical interference and artifact
- Poor impedance
- Displaced stimulation pads, leads, or electrodes
- Inaccurate location of stimulating or recording leads
- Edema and swollen limbs
- Machine malfunction
- Improper display or testing settings
- Check for stimulation artifact and muscle twitching
2. Positional issues:2
- Vascular insufficiency due to occlusion
- Mechanical stretch or pressure on plexus or nerves
- Due to extreme head position with neck hyperextension or flexion, peripheral nerve compression, spine flexion or extension
- Changes in upper extremity EPs:
- If prone, reposition arms and consider further extension
- If supine, check pulse at wrist, release shoulder tape if possible
- Remove blood pressure cuff
- Changes in lower extremity EPs
- Ensure legs are still on the operating table
- Ensure good perfusion and check pulses
- Loosen straps around the legs
- Changes in upper extremity EPs:
3. Pharmacological issues/anesthesia changes2
- Added halogenated agents or nitrous oxide
- Change in concentration of halogenated agents
- Intravenous (IV) bolus dose
- Change in infusion rate
- Change in muscle relaxation
- Epidural, intrathecal, or regional block
- Anesthesia is the most likely cause of signal change when the change is noted in multiple extremities and when the cortical signals are affected more than the subcortical signals.
- The subcortical signals are more resistant to change and are often more reliable.
4. Physiologic:
- Temperature change
- Hypothermia affects axonal function. Even small changes in temperature can cause a delay in latency and a reduction in the amplitude of the cortical and subcortical SSEPs and MEPs.1
- Relative hyperthermia has the opposite effect.
- Regional cooling, like with cold irrigation to surgical site or cold IV solutions, as well as active warming, can result in changes even when core body temperature is unchanged.2
- A stable temperature should be maintained when possible (within 2-2.5°C of baseline temperature).2
- Blood flow and blood pressure (BP) change
- When the BP decreases, the signal amplitudes decrease globally.
- Causes of blood flow and BP changes include autonomic changes, loss of autoregulation, blood and volume loss, poor cardiac output, or vascular steal phenomenon.
- Appropriate mean arterial pressure (MAP) should be maintained for optimal central nervous system perfusion. This should be at least 65 mmHg during intracranial neurosurgery, and often 80 mmHg during spine surgery.
- A reduction in regional blood flow, resulting in focal signal change, can result from surgical compression, spinal distraction, vascular compromise from position, tourniquets, retractor, clip, or vasospasm.
- Intracranial pressure (ICP) change
- Elevated ICPs result in loss of cortical SSEP > MEP > subcortical SSEP > BAEP
- Changes in ventilation and oxygenation
- EP are affected when pH is less than 7.2 or PaCO2 is less than 20 mmHg.
- Hypoxia is poorly tolerated and can contribute to neuronal dysfunction.
- Hematocrit change/blood loss
- When the hematocrit decreases, the amplitude of EP decreases.
- A decrease in EP can occur with extreme anemia.
- The hemoglobin should be maintained close to the baseline to maximize oxygen delivery.
Recommendations for the Anesthesia Team1-4
- The monitoring team should be kept abreast of any significant anesthetic, physiologic, and homeostatic changes. Notify the team of:
- any changes in anesthetics, including boluses, change in infusion rates, and use of halogenated agents or nitrous oxide;
- significant fluctuations in the patient’s blood pressure, ventilation, blood loss, temperature, ability to palpate pulses, glucose level extremes, electrolyte abnormalities, or changes in position.
- IONM can be used with most anesthetic techniques. However, there is a need for clear understanding of the anesthetic effects on IONM signals and an open communication amongst teams.
- For SSEP monitoring:
- Use low dose halogenated agents:
- Less than 0.5 MAC (up to 1 MAC)
- Sevoflurane and desflurane are preferred over isoflurane
- N2O should be avoided and not combined with other inhalational agents
- IV agents
- Using relatively high dose opioid infusions should be considered if appropriate (sufentanil up to 1mcg/kg/hour, or remifentanil 0.1-0.5 mcg/kg/min, or fentanyl up to 10 mcg/kg/hour).2
- Ketamine or etomidate should be considered, if not contraindicated.
- Lower dose propofol infusion (around 75-100 mcg/kg/min, though effective rate can vary significantly among patients) should be maintained.
- NMBA can help speed up SSEP by eliminating EMG artifacts and noise.
- Use low dose halogenated agents:
- For MEP monitoring:
- The physician should ensure that bite blocks are in place prior to stimulation and after positioning.
- NMBA should be avoided until the baseline MEPs are obtained.
- NMBA should be avoided (especially high dose intermediate to long-acting agents). If used, maintain the train-of-four (TOF) with at least 2/4 twitches.
- Opioid infusions should be considered, if appropriate.
- TIVA with propofol and opioids +/- ketamine, dexmedetomidine or lidocaine is preferred when possible.
- If inhalational agents are needed, less than 0.5 MAC should be used.
- For BAEP monitoring
- Both inhalational and IV agents may be used.
- For EEG monitoring
- Halogenated agents: Less than 0.5 MAC should be used
- Relatively high dose opioid
- +/- NMBA
- When burst suppression is needed for aneurysm clipping, propofol infusion can be titrated up to 150 mcg/kg/min and then replaced by opioid (like remifentanil) with 0.5 MAC inhalational agent after clipping.2
- For EMG monitoring
- Inhalational agent less than 1.5 MAC
- IV agents (opioid)
- NMBA should be avoided if possible. If NMBAs are used, consider using short-acting agents in low doses, and maintain the TOF at least 2/4 twitches
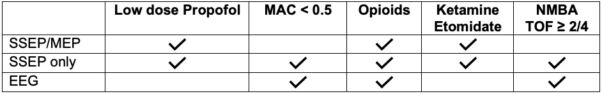
Table 1. Recommended anesthetic depending on IONM modality
References
- Husain, A. Practical Approach to Neurophysiologic Intraoperative Monitoring. Demos Medical Publishing, 2008. ProQuest Ebook Central.
- Koht A, Sloan TB, Toleikis JR (Editors) Monitoring the Nervous System for Anesthesiologists and Other Health Care Professionals, Second Edition. Springer, 2017.
- Legatt AD, Arezzo JC, Vaughan HG Jr. The anatomic and physiologic bases of brain stem auditory evoked potentials. Neurol Clin. 1988;6(4):681-704. PubMed
- Shils JL, Sloan TB. Intraoperative neuromonitoring. Int Anesthesiol Clin. 2015;53(1):53-73. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.