Copy link
Ehlers-Danlos Syndrome
Last updated: 06/24/2025
Key Points
- Ehlers-Danlos syndrome (EDS) is a heterogeneous group of connective tissue disorders caused by abnormal collagen, which can exhibit different clinical phenotypes.
- EDS patients can present unique challenges to anesthesia providers, such as a higher risk of bleeding, cardiopulmonary complications, abnormal healing, and local anesthetic resistance. Understanding these challenges can help anesthesia providers better care for their patients.
Introduction
- EDS refers to a group of inherited connective tissue disorders caused by abnormal collagen. These defects lead to increased tissue elasticity and varying clinical manifestations, which can result in significant morbidity and mortality.
- Collagen is found in nearly all organ systems, so EDS can affect various organs, making anesthetic management particularly challenging. This summary outlines how EDS affects patients, its unique pathophysiology, and the anesthetic considerations for managing individuals with this condition.
Epidemiology
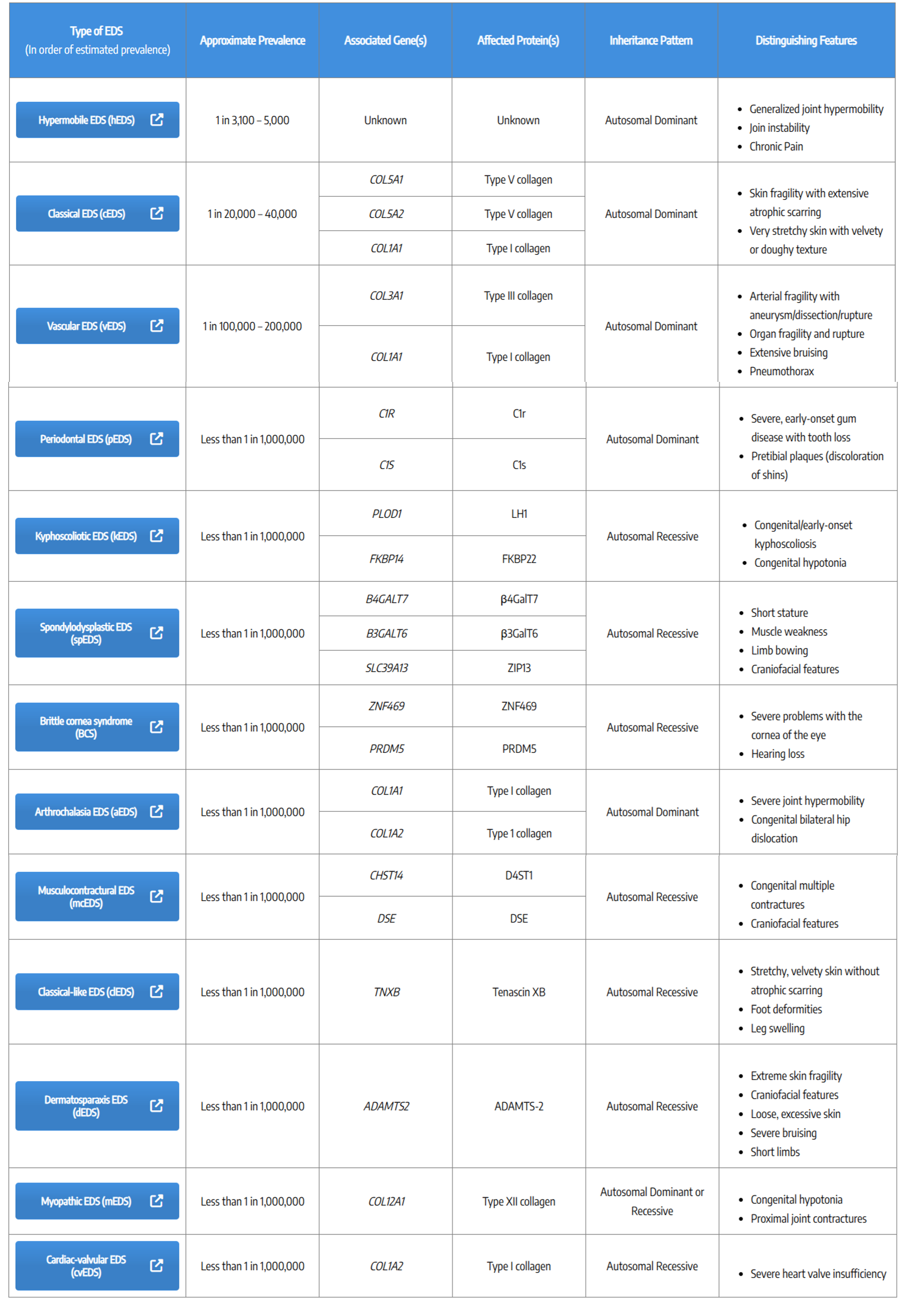
- EDS consists of multiple forms with different genotypes and phenotypes, ranging in prevalence and severity. The most common type is hypermobile EDS, affecting 1 in 3,100–5,000 individuals, followed by the classical type (1 in 20,000–40,000) and vascular EDS (vEDS) (1 in 100,000–200,000).
- Other subtypes are rare, affecting fewer than 1 in one million people.1 EDS can be inherited as autosomal dominant, autosomal recessive, or arise from de novo mutations.
- Clinically, EDS typically presents with skin hyperelasticity, joint hypermobility, atrophic scarring, and vascular fragility. Each subtype has distinct symptoms, some of which overlap with those of others, and the severity of symptoms can vary significantly among individuals with the same subtype. In 2017, an international classification system was established to better categorize EDS.2 Table 1 is a summary of 13 EDS subtypes from the Ehlers-Danlos Society.3
Understanding the specific EDS subtype can help prepare for appropriate patient care.
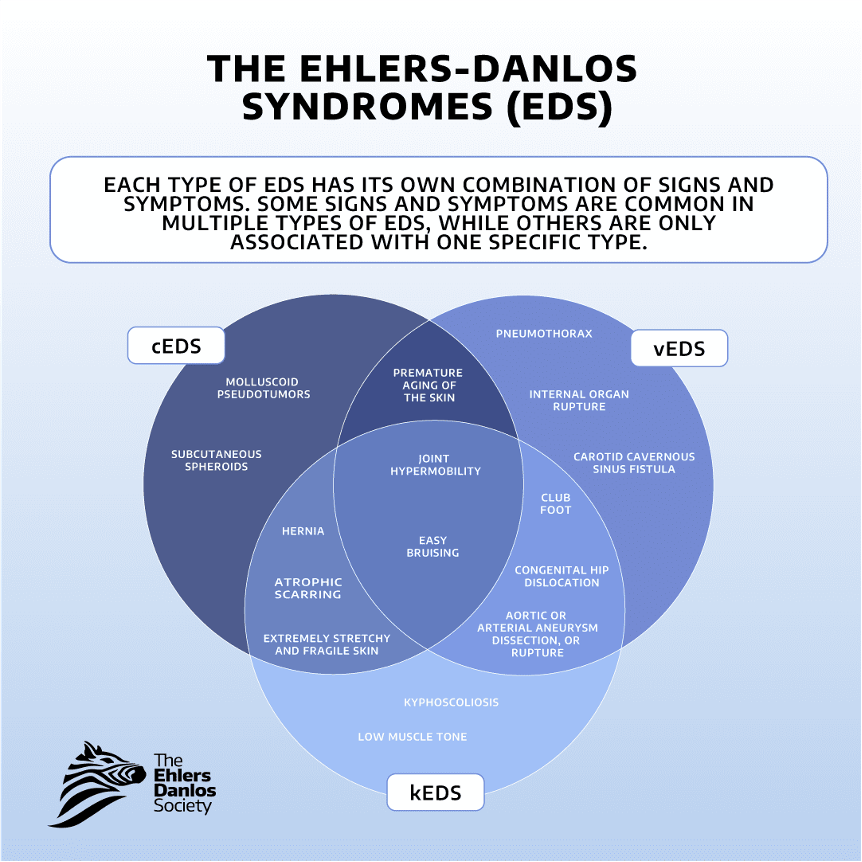
Figure 1: Clinical presentation of EDS. Figure reproduced by permission from © 2025 The Ehlers-Danlos Society.3
Pathophysiology
- EDS primarily impairs collagen production. Collagen is found in multiple organ systems throughout the body and can therefore lead to varying degrees of symptoms. The most common forms of collagen affected in EDS are Types I, III, and V, which are all fibrillar types of collagen.4
- The different genetic mutations that lead to EDS can arise from errors in the enzymes responsible for modifying and processing these collagens. Here is a summary of the various subtypes of collagen affected by EDS and the pathophysiology of how the error in collagen formation can lead to different symptomatology.
Defects in Type I Procollagen (Arthrochalasia EDS, Dermatosparaxis EDS, Cardiac vEDS)
- Type I collagen is found in the body’s extracellular matrix (ECM) and connective tissues, and it functions to provide structure and mechanical scaffolds and to support connective tissues such as skin, blood vessels, tendons, ligaments, and bones. Genetic mutations can cause amino acid substitutions in the formation of type I collagen, leading to hyperelasticity in the skin, easy bruising, joint hypermobility, joint and muscle pain, increased susceptibility to arterial rupture, and abnormal scarring.4
Defects in Type III Procollagen (vEDS)
- Type III collagen functions to organize the ECM and regulate fibril formation. This is the most abundant form of collagen found in compliant tissues, such as the skin dermis, blood vessel walls, gastrointestinal (GI) tract, uterus, lungs, liver, and spleen.4
Defects in Type V Procollagen (Classical)
- Type V collagen is responsible for creating the scaffold that allows type I collagen to form correctly. Furthermore, it functions as a major regulator of collagen fibril formation, ECM organization, wound healing, endoplasmic reticulum homeostasis, and autophagy.4 Decreased type V collagen is responsible for symptoms associated with classical EDS. Type V collagen is found in various body parts, including the skin, cell surfaces, placenta, tendons, and bones.
Defects in the Modification and Processing of Collagen
- Variants of EDS that affect collagen crosslinking and folding include kyphoscoliotic EDS. Impaired crosslink formation can lead to scoliosis and atrial fragility in patients due to mechanical instability in affected tissues.4
- Classical-like EDS is affected by defects in the ECM bridging molecules (not collagen), specifically tenascin-x (TNX). Loss of function of TNX leads to skin hyperextensibility without atrophic scarring, significant nursing, joint hypermobility, muscle weakness, and contractures.4
- Type XII collagen is a fibril-associated collagen that binds to TNX, forming flexible bridges between collagen fibrils and other ECM molecules. Type XII collagen is disturbed in myopathic EDS.4
Defects in Proteoglycans
- Proteoglycans are found in the ECM and on the cell surface. They play a crucial role in cell-to-cell communication, cell-matrix interactions, cell growth and differentiation, and interactions with other molecules found in the ECM, such as collagen.
- Defects in proteoglycan synthesis cause spondylodysplastic EDS, which presents with symptoms including skin hyperextensibility and joint hypermobility.
- Musculocontractural EDS is another form of EDS caused by defective proteoglycans, which can lead to craniofacial anomalies, contractures, ocular and visceral malformations, and tissue fragility.
Defects Present in Other Forms of EDS
- Brittle cornea syndrome is associated with errors in zinc finger proteins and has been linked to defects in corneal development and structural tissue integrity.4
- Defects in the complement pathway cause periodontal EDS.4
Anesthetic Considerations
Given the variety of organ systems involved in the various subtypes of EDS, there are distinct considerations for each organ system when planning care for patients with EDS.
Cardiovascular
- vEDS patients are most vulnerable to cardiac issues, especially mitral valve prolapse and aortic root dilation. Early echocardiograms are recommended, ideally at the time of diagnosis or by age 5.
- Screening: Murmurs should be listened for, and a bedside transthoracic echocardiogram can help identify valvular abnormalities. Common valvular abnormalities include aortic insufficiency or mitral valve prolapse.
- Arterial risks: If possible, arterial angiography or arterial line placement should be avoided, as there is an increased risk of arterial rupture.
- Hypotension: Permissive hypotension may help reduce the risk of arterial dissection or rupture in vascular subtypes.4
Hematology
- Bleeding risk: Patients are more prone to bleeding due to abnormal collagen and ECM interactions. Based on expected blood loss during surgery, blood products should be available.
- Fragile tissue: Classical and vascular subtypes present with fragile tissues, increasing the risk of bruising, tearing, or vascular damage during routine procedures such as IV insertion.5
- Nonsteroidal anti-inflammatory drugs (NSAIDs): The risks and benefits of NSAIDs should be carefully evaluated before their use.4
Respiratory
- Pneumothorax and diaphragm rupture: There is a higher risk of these complications in various EDS subtypes.
- Lung disease: Some patients may have restrictive lung disease (i.e., from scoliosis or pectus deformities) or hypoplasia with associated complications, such as frequent infections, pulmonary hypertension, and chronic respiratory failure. Lung-protective ventilation with adjusted peak pressures and tidal volumes should be used. The potential for prolonged mechanical ventilation should be discussed with high-risk patients.
- Airway management: Difficult intubation, especially in cases of micrognathia, high-arched palates, or cervical instability should be anticipated. Fiberoptic scopes may be necessary for intubation. Patients may require a smaller-sized endotracheal tube due to potential subglottic stenosis; therefore, the minimum necessary cuff pressure should be used to reduce mucosal stress.5
- Tracheal collapse and obstructive sleep apnea (OSA): Patients are at a higher risk of developing tracheobronchomalacia and OSA, especially after undergoing anesthesia. Maintaining spontaneous respiration and using postoperative airway support devices should be considered to reduce complications.8
- Vocal cord dysfunction: Laxity of the vocal cords and dysmotility of the cricoarytenoid joint can result in dysphonia. During laryngoscopy, there is an increased risk of laryngospasm and vocal cord damage.
- Temporomandibular joint (TMJ): Joint hypermobility increases the risk of TMJ dislocations or subluxation; extra caution is needed when opening the patient’s mouth.5
Gastrointestinal
- Gastrointestinal (GI) perforation: EDS patients are at a higher risk of bowel perforation, especially during routine procedures such as colonoscopies.
- Pelvic floor dysfunction: The potential need for Foley catheter placement in some cases due to defecation and urinary evacuation issues should be considered.4
- Esophageal rupture: Certain subtypes have an increased risk; adequate postoperative nausea and vomiting prophylaxis should be ensured to prevent rupture.5
- GI motility issues: Some patients may benefit from prokinetic drugs to address motility problems. Providers should take precautions to minimize the risk of aspiration.
Skeletal
- Skeletal anomalies: EDS patients may have scoliosis, kyphosis, craniocervical instability, and other spinal issues. Epidural or spinal anesthesia may be challenging or contraindicated, depending on the manifestations.5
- Joint dislocations: Patients with joint hypermobility are at an increased risk of dislocations during anesthesia. Proper padding and securing during surgery are essential to avoid injury.5
- Bone density: Some EDS patients have reduced bone density and may require medication to enhance their bone health.
- Tourniquet use: If possible, the use of tourniquets should be avoided, after discussing with surgeons. There is a high risk for compartment syndrome and serious bleeding.5
Pregnancy
- vEDS: There is a risk of increased maternal mortality (up to 5/100 pregnancies), particularly due to uterine rupture and arterial blood loss. Blood products should be available for transfusion.
- Other subtypes: There is an increased risk of premature birth and vaginal/cervical tears.4
- Neuraxial anesthesia: There is a risk of ineffective spinal/epidural due to resistance to local anesthetic and possibly dural ectasia. As mentioned above, there is a higher chance of hematoma formation and difficult placement due to skeletal anomalies.
Pain Management
- Chronic Pain: EDS patients are prone to chronic pain, central sensitization, and complex regional pain syndrome.5,6 Opioids alone may not be effective for pain control, and an opioid-reduced anesthetic plan may be beneficial.
- Adjuvant medications: Using dexmedetomidine, lidocaine, ketamine, and peripheral nerve blocks for opioid-sparing anesthesia should be considered.
- Local anesthetic resistance: Patients with hypermobile EDS, in particular, may be resistant to local anesthetics. A study found that EDS patients were three times more likely to experience dental block failure than non-EDS patients.7 Providers should be cautious with local anesthetic doses, particularly for epidurals, spinal, and nerve blocks.
References
- Miklovic T, Sieg VC. Ehlers-Danlos syndrome. In: StatPearls [Internet]. StatPearls Publishing; May 29, 2023. Link
- Malfait F, Castori M, Francomano CA, et al. The Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017. Link
- Ehlers-Danlos Society. Types of Ehlers-Danlos syndrome. Accessed March 24, 2025. Link
- Malfait F, Castori M, Francomano CA, et al. The Ehlers-Danlos syndromes. Nat Rev Dis Primers. 2020;6(1):64. PubMed
- OrphanAnesthesia. Ehlers-Danlos syndrome. Accessed March 24, 2025. Link
- Ramírez-Paesano C, Rodiera Clarens C, Sharp Segovia A, Coila Bustinza A, Rodiera Olive J, Juanola Galceran A. Perioperative opioid-minimization approach as a useful protocol in the management of patients with Ehlers-Danlos syndrome-hypermobility type, craniocervical instability and severe chronic pain who are to undergo occipito-cervical fixation. Orphanet J Rare Dis. 2023;18(1):214. Published 2023 Jul 25. doi:10.1186/s13023-023-02829-9 PubMed
- Feldman ECH, Hivick DP, Slepian PM, et al. Pain symptomatology and management in pediatric Ehlers–Danlos syndrome: A review. Children (Basel). 2020;7(9):146. PubMed
- Sedky K, Gaisl T, Bennett DS. Prevalence of obstructive sleep apnea in joint hypermobility syndrome: A systematic review and meta-analysis. J Clin Sleep Med. 2019;15(2):293-99. PubMed
- Schubart JR, Schaefer E, Janicki P, et al. Resistance to local anesthesia in people with the Ehlers-Danlos syndromes presenting for dental surgery. J Dent Anesth Pain Med. 2019;19(5):261-70. PubMed
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.