Copy link
Drug Metabolism in Pregnancy
Last updated: 12/21/2023
Key Points
- Drug metabolism refers to enzymatic activity that causes chemical modifications, resulting in either activation of a prodrug or loss of biological activity. Most drugs are metabolized in the liver. The activity of most, but not all, enzymes involved in hepatic drug metabolism is increased during pregnancy.
- Most drugs are renally eliminated. The elimination rates of renally cleared medications increase during pregnancy due to increases in renal blood flow and glomerular filtration rate.
- Drug activity is also affected by the volume of distribution. Increases in plasma volume and decreases in plasma protein concentration affect the free fraction of many drugs.
- Changes in drug metabolism and physiologic activity affect dosing considerations for some commonly anesthetic agents.
Introduction
- The majority of organ systems are affected by the anatomic and physiologic changes during pregnancy.1
- Changes to the hepatic and renal systems in pregnancy significantly affect the pharmacokinetic (absorption, distribution, metabolism, and elimination) and pharmacodynamic properties of many medications.2-5
- Expansion of plasma volume results in the dilution of plasma proteins (concentrations of albumin and α1-acid glycoprotein, for example, decrease 20-40% at term). This leads to decreased drug binding and increased concentrations of unbound drugs.1-3
Hepatic and Renal Changes in Pregnancy
Hepatic Changes
- Many drugs undergo hepatic metabolism, so changes in hepatic physiology can result in significant changes in drug metabolism.
- Most members of the cytochrome P450 enzyme family have increased activity during pregnancy, resulting in increased metabolism of many commonly used drugs (Table 1). The mechanism for this increase has not been fully elucidated but may be related to changes in cortisol, estradiol, or progesterone.
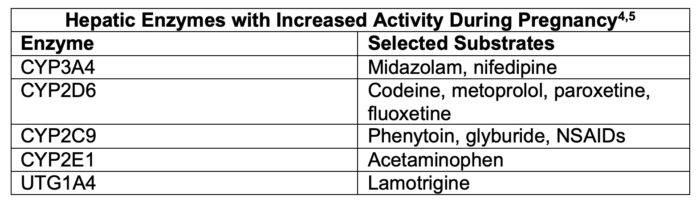
Table 1. Hepatic enzymes with increased activity during pregnancy
- The activities of a smaller number of hepatic enzymes involved in drug metabolism are decreased during pregnancy (Table 2).
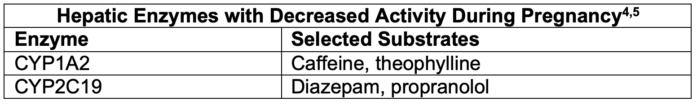
Table 2. Hepatic enzymes with decreased activity during pregnancy
- Liver size, morphology, and blood flow do not change.
Renal Changes
- Renal blood flow is 75% greater than prepregnancy by 16 weeks. By 34 weeks, renal blood flow declines to 50% above baseline and remains stable until the end of pregnancy.1
- Creatinine clearance is increased from 120 mL/min at baseline to 150 to 200 mL/min early in pregnancy, with a slight decrease near term. The mechanism behind the increase in glomerular filtration rate is likely secondary to vasodilation of afferent and efferent arterioles.1
- The increase in renal clearance can have a significant increase (20–65%) in the elimination rates of renally cleared medications leading to shorter half-lives.4,5
- The kidneys are also involved in water and sodium osmoregulation. Pregnancy results in a significant increase in sodium and water retention. Total body water increases 6-8 L, and the “dilutional effect” leads to mild hyponatremia. This volume expansion leads to reductions in peak serum concentrations (Cmax) of many hydrophilic drugs, particularly if the drug has a relatively small volume of distribution.4,5
Dosing Considerations for Commonly Used Anesthetic Agents
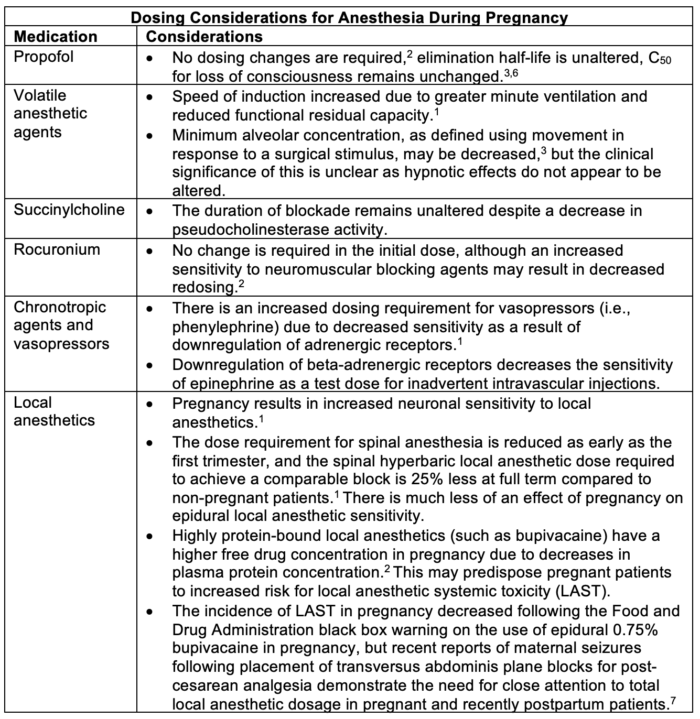
Table 3. Dosing considerations for anesthesia during pregnancy
Placental Drug Transfer and Metabolism
- The placenta is a semipermeable barrier to drug passage, much like the blood–brain barrier. Placental drug transfer is determined by a number of characteristics as outlined in Table 4.
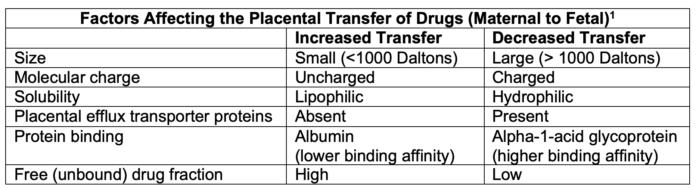
Table 4. Factors affecting the placental transfer of drugs
- The placenta is capable of drug metabolism; it expresses both phase 1 enzymes (oxidation, reduction, and hydrolysis) and phase 2 enzymes (conjugation) like the liver. Phase 1 enzymes expressed by the placenta include CYP1A1, CYP2E1, CYP3A4, CYP3A5, CYP3A7, CYP4B1, and CYP19 (aromatase).2
- Prednisone and dexamethasone undergo significant placental metabolism in pregnancy.2
- The esterases that metabolize remifentanil are highly expressed in the placenta. This results in much lower fetal remifentanil concentrations when compared to the mother.
References
- Kacmar R, Gaiser R. Physiologic changes of pregnancy. In: Chestnut DH, Nathan N. Chestnut’s Obstetric Anesthesia: Principles and Practice. Sixth edition. Philadelphia. Elsevier; 2020: 13-29.
- Ansari J, Carvalho B, Shafer SL, et al. Pharmacokinetics and pharmacodynamics of drugs commonly used in pregnancy and parturition. Anesth Analg. 2016; 122:786–804. PubMed
- Gin T. Pharmacology during pregnancy and lactation. In: Chestnut DH, Nathan N. Chestnut’s Obstetric Anesthesia: Principles and Practice. Sixth edition. Philadelphia: Elsevier; 2020: 313-35.
- Feghali M, Venkataramanan R, Caritis S. Pharmacokinetics of drugs in pregnancy. Semin Perinatol. 2015; 39:512–9. PubMed
- Tasnif Y, Morado J, Hebert MF. Pregnancy-related pharmacokinetic changes. Clin Pharmacol Ther. 2016; 100:53–62. PubMed
- Higuchi H, Adachi Y, Arimura S, Kanno M, Sato H. Early pregnancy does not reduce the C(50) of propofol for loss of consciousness. Anesth Analg. 2001; 1565-9. PubMed
- 7. Weiss E, Jolly C, Dumoulin JL, et al. Convulsions in 2 patients after bilateral ultrasound-guided transversus abdominis plane blocks for cesarean analgesia. Reg Anesth Pain Med. 2014; 39:248–51. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.