Copy link
Coronary Artery Anatomy and Coronary Perfusion Pressure
Last updated: 10/15/2025
Key Points
- There are two main coronary arteries, left and right, that supply the heart.
- The major coronary vessel that feeds the posterior descending artery (PDA) determines the “dominance” of the coronary circulation.1
- Occlusion of a specific coronary artery may lead to regional electrocardiographic (ECG) changes with associated wall motion abnormalities on echocardiogram.
- The left ventricle (LV) is perfused during diastole, while the right ventricle (RV) is perfused during both diastole and systole.
Introduction
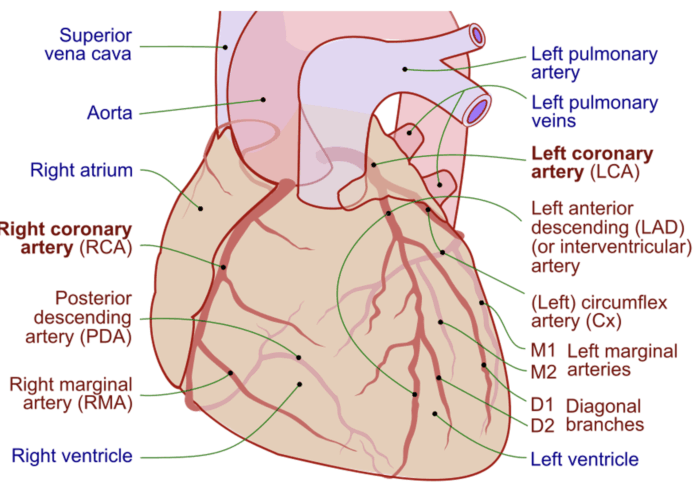
- The right and left coronary arteries (RCA and LCA, respectively) provide blood supply to the entire myocardium2 (Figure 1).
- The RCA typically supplies the right atrium, a majority of the RV, and, in most individuals, part of the interventricular septum via the PDA.
- The LCA normally supplies the left atrium, most of the interventricular septum, and LV.1,2
- A critical stenosis or acute occlusion of these vessels can lead to specific ECG changes accompanied by regional wall motion abnormalities on echocardiography.
- Understanding the anatomy of the coronary arteries and the distribution of their blood supply can aid in the swift diagnosis and management of these lesions.
Anatomy
Dominance
- Dominance of the coronary circulation is determined by which main coronary vessel, left versus right, supplies the PDA.1
- In a right-dominant circulation, the RCA supplies the PDA.
- In a left-dominant circulation, the left circumflex artery (LCCA), a branch of the LCA, supplies the PDA.
- In a co-dominant circulation, the PDA receives dual supply from both the RCA and LCA.3
- It is estimated that approximately 80% of people have a right dominant circulation, while the remaining 20% are either left dominant (approximately 8%) or co-dominant (about 7%).3
Left Coronary Artery
- The LCA originates from the left Sinus of Valsalva in the ascending aorta and passes between the left atrium and pulmonary artery.
- The LCA bifurcates into the left anterior descending artery (LAD) and the LCCA.
- The LAD courses down the anterior interventricular groove and provides numerous Diagonal (typically Diagonal 1-Diagonal 3) and septal perforator branches.4
- The LCCA travels in the atrioventricular (AV) groove, giving off the obtuse marginal (OM) branch that supplies the anterior and posterior aspects of the lateral wall.1
- In a left-dominant circulation, the LCCA wraps around the AV groove and supplies the PDA.2
- In addition to supplying the left atrium, most of the interventricular septum, and LV (anteroseptal and lateral walls), the LCCA also partially supplies the bundle of His, and the anterior and posterior papillary muscles of the mitral valve.1,2
- Critical stenosis or acute occlusion of the LAD produces ECG changes in V1-V4, accompanied by regional wall motion dysfunction in the anterior wall and apex based on its distribution.5
- LCCA occlusion produces ECG changes in I, aVL, V5, and V6 with regional wall motion abnormalities in the lateral wall that may be seen on echocardiogram.
Right Coronary Artery
- The RCA originates from the right sinus of Valsalva in the ascending aorta. It gives off the sinoatrial (SA) and AV nodal arteries as well as the PDA in 80% of individuals.
- The RCA supplies the medial aspect of the posterior wall as well as the posterior third of the interventricular septum.1
- In 60% of patients, the RCA provides arterial supply to the SA node, while the LAD supplies the SA node in the remaining 40%.2
- Additionally, the RCA supplies the AV node branch in 85-90% of people, while the LCCA supplies the AV node in the remaining 10-15%.2
- In two-thirds of patients, the posteromedial papillary muscle is supplied by a single coronary artery, most commonly the RCA. This leaves the posteromedial papillary muscle more vulnerable to ischemia compared to the anterolateral papillary muscle in the event of occlusion of the single arterial supply.
- RCA occlusion causes ischemic changes in II, III, and aVF with regional wall motion abnormalities in the RV and inferoseptal and inferior regions of the LV, if the PDA is supplied by the RCA.
Wall Motion Abnormalities
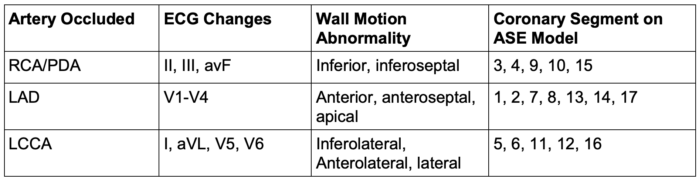
Table 1. Coronary artery distribution, ECG changes, and wall motion abnormalities.
Abbreviations: RCA: Right coronary artery; PDA: Posterior descending artery; LAD: Left anterior descending artery; LCCA: Left circumflex artery; ECG: Electrocardiogram; ASE: American Society of Echocardiography
- Regional wall motion abnormalities are specific areas in the myocardium with abnormal contractile function.
- The distribution of the wall motion abnormalities should correspond to the territory supplied by a coronary artery.
- Regional wall motion is assessed by a scoring system based on the 17 segments of the LV6 (Figure 2).
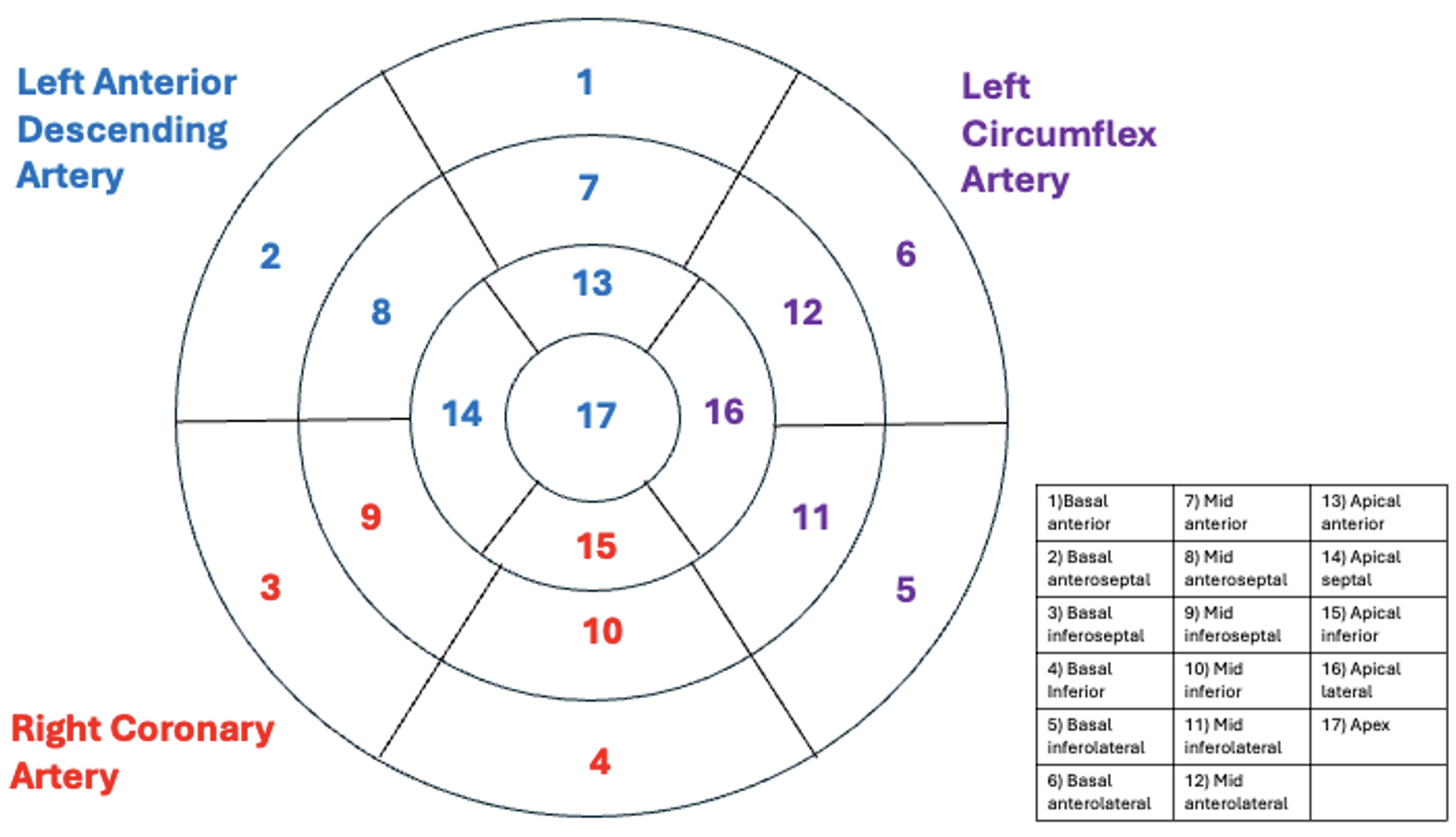
Figure 2. 17-segment model of the coronary artery circulation of the left ventricle
- Each segment is then assessed using a wall motion score (see Table 2 below).6
- The wall motion score index (WMSI) is then calculated by dividing the total number of points from the wall motion score above by 17.
- A WMSI of 1 (17➗17) is considered normokinetic.
- Therefore, the higher the WMSI, the greater the degree of dysfunction.
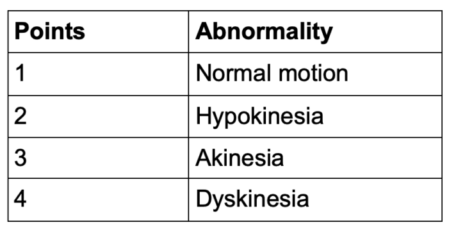
Table 2. Wall motion score
Coronary Perfusion Pressure (CPP)
- In the average adult, coronary blood flow is approximately 250 mL/min (4-5% of cardiac output).1
- CPP = aortic diastolic pressure (AoDP) – left ventricular end-diastolic pressure.
- CPP is based on the diastolic pressure difference between the aorta and the ventricle because the left ventricular myocardium is perfused during diastole rather than systole.
- Unlike other organs, the heart receives its perfusion intermittently rather than continuously because of myocardial contraction.2
- During systole, the myocardial pressure in the LV rises and approximates arterial pressure.
- The compression of the intramyocardial portion of the coronaries during systole occludes the vessels, temporarily stopping, or even transiently reversing, flow in the epicardial vessels.2 As a result, the LV is perfused almost entirely during diastole.
- However, the right atrium, RV, and left atrium are perfused during both systole and diastole because aortic pressure is usually greater than the pressure in these chambers (except in cases of pulmonary hypertension).1
- CPP is reduced with decreases in AoDP (seen with severe aortic valvular insufficiency) or increases in end-diastolic pressure (heart failure).1,2
- With decreases in CPP, the subendocardial layer is most susceptible to ischemia because it is exposed to higher pressure during systole.
References
- Pagel PS, Stowe DF. Cardiac anatomy and physiology. In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC, Ortega R, Sharar SR, Holt NF. Clinical Anesthesia (Barash), 8e. Philadelphia; Wolters Kluwer; 2017: Chapter 12
- Chapter 20. Cardiovascular Physiology & Anesthesia. In: Butterworth JF, IV, Mackey DC, Wasnick JD. Morgan & Mikhail’s Clinical Anesthesiology, 5e. McGraw-Hill; 2013: 362
- Baim DS, Grossman W. Grossman’s cardiac catheterization, angiography, and intervention. Philadelphia; Lippincott Williams & Wilkins; 2006.
- Rehman I, Kerndt CC, Rehman A. Anatomy, thorax, heart, left anterior descending (LAD) artery. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. Link
- Ogobuiro I, Wehrle CJ, Tuma F. Anatomy, thorax, heart, coronary arteries. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. PubMed
- Lang, R. et al, Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular. Journal of the American Society of Echocardiography. 2015; 28 (1): 10-13. PubMed
Other References
- Bechtel A. TEE views and coronary perfusion pressure. OA Keys to the Cart. 2018. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.