Copy link
Continuing vs. Stopping Cardiovascular Medications, Antiplatelet Agents, and Anticoagulants Before Noncardiac Surgery
Last updated: 10/22/2025
Key Points
- Beta blockers, calcium channel blockers, and statins should be continued uninterrupted up to and including the day of surgery.
- Potassium-sparing diuretics can be continued as prescribed, whereas loop diuretics are typically held except in select patients with severe heart failure.
- There is no difference in outcomes between patients who continue or discontinue angiotensin-converting enzyme inhibitors/angiotensin receptor blockers. Holding reduces intraoperative hypotension but increases postoperative hypertension.
- Patients on low-dose aspirin with a history of prior stent placement (coronary or cerebrovascular) should continue aspirin uninterrupted unless scheduled for very high-risk surgery (e.g., intracranial surgeries).
- Patients on P2Y12 inhibitors typically hold them for 5-7 days except for patients who have had a stroke, myocardial infarction or a stent within the last 12 months. Discontinuing antiplatelet medications in these patients should involve a specialist recommendation.
- Direct oral anticoagulants taken for stroke prevention or history of venous thromboembolism (VTE) are typically held for two days prior to surgery and do not require bridging with low molecular weight heparin (LMWH).
- Patients with a VTE within three months requiring urgent surgery should have a specialist recommendation for anticoagulation management and may require a bridge with LMWH.
- Given the long half-life of warfarin, it is typically held for 5 days prior to surgery. Patients at a high risk of VTE (CHA2DS2VASc score ≥7, severe thrombophilia, or certain types of mechanical valves) should be bridged with LMWH.
Introduction
- The majority of adult patients presenting for surgery are on chronic medicines. A detailed medication reconciliation is crucial for verifying the accuracy and dosage of medications.
- Most medications taken for optimization of cardiovascular disease should be continued in order to avoid exacerbation of disease and to maintain an optimized physiologic state
- However, there are some indications for interrupting medications:
- Increased bleeding
- Interactions with anesthesia
- Complications associated with perioperative stress and fasting state
- If oral intake is restricted or if impaired gastrointestinal absorption is anticipated, per-oral medications can be substituted with intravenous, transdermal, or transmucosal formulations, if available.
- Cardiovascular medications can be restarted in the postoperative period once the patient can tolerate oral intake.
Cardiovascular Medications
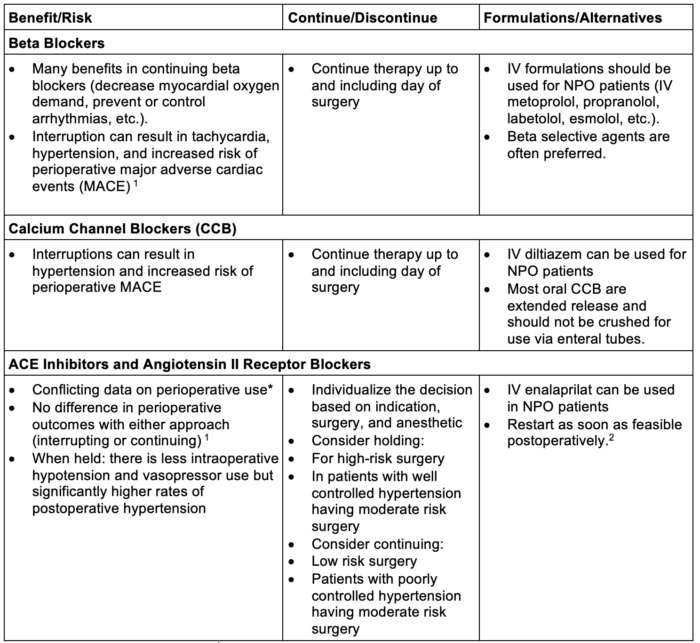
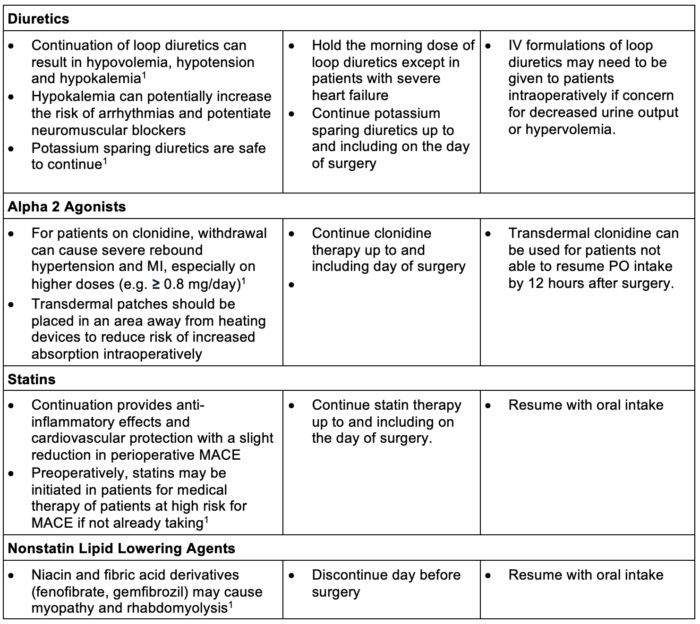
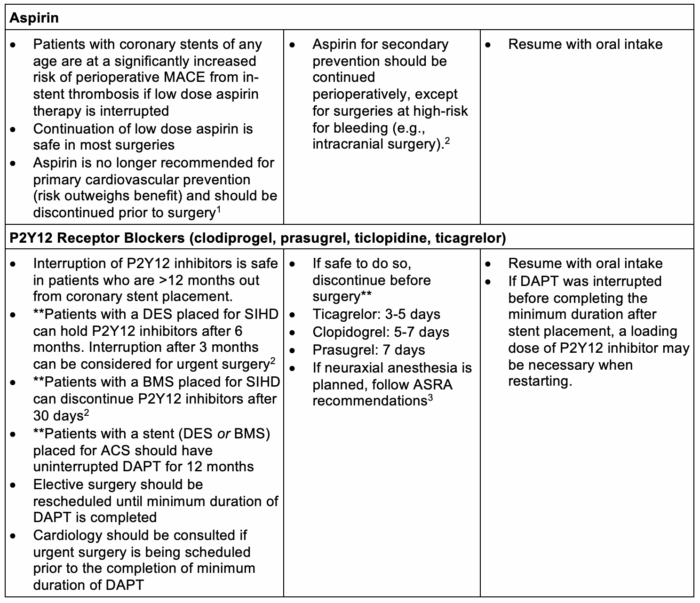
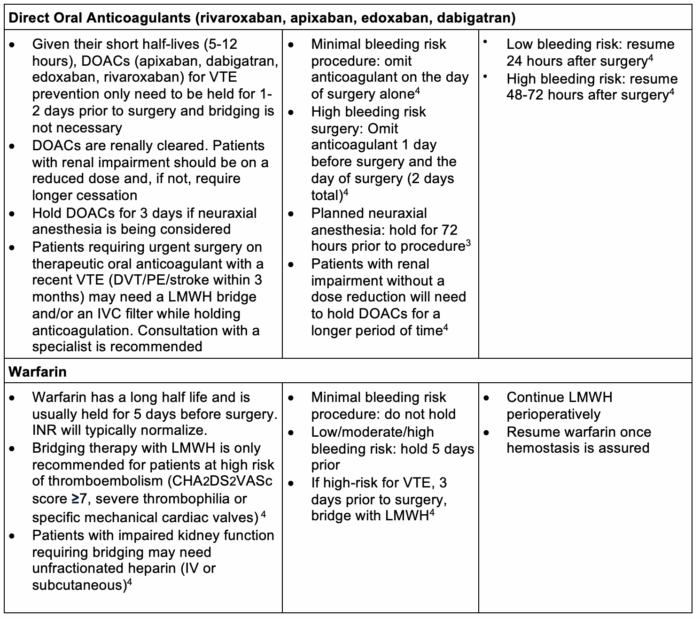
Table 1. Perioperative management of cardiovascular medications. Abbreviations: DOS = day of surgery, NPO = nil per os, IV = intravenous, MACE = major adverse cardiac events, MI = myocardial infarction, DES = drug eluting stent, SIHD = stable ischemic heart disease, BMS = bare metal stent, ACS = acute coronary syndrome, DAPT = dual antiplatelet therapy, ASRA = American Society for Regional Anesthesia, DOAC = direct oral anticoagulant, VTE = venous thromboembolism, DVT = deep venous thrombosis, PE = pulmonary embolism, LMWH = low molecular weight heparin, IVC = Inferior vena cava, INR= International normalized ratio.
* Please see the OA summaries on the renin-angiotensin-aldosterone system Link and anesthesia for patients with hypertension. Link
** Please see the OA summary on antiplatelet agents. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.