Copy link
Complex Regional Pain Syndrome
Last updated: 05/22/2025
Key Points
- Complex regional pain syndrome (CRPS) is a neuropathic pain disorder, usually affecting the distal limbs, characterized by pain, swelling, limited range of motion, vasomotor instability, skin changes, and patchy bone demineralization.
- The pain is not restricted to a nerve territory or dermatome, is disproportionate to the degree of tissue injury, and persists beyond the normal expected time for tissue healing.
- Treatment is guided by a multidisciplinary approach. The first-line therapy includes physical therapy, occupational therapy, and nonsteroidal anti-inflammatory drugs (NSAIDs).
Introduction and Pathogenesis
- CRPS is a neuropathic pain disorder, usually affecting the distal limbs, characterized by pain, swelling, limited range of motion, vasomotor instability, skin changes, and patchy bone demineralization.1,2 It often begins following a fracture, soft tissue injury, or surgery.
- A consensus definition of CRPS is as follows: “CRPS describes an array of painful conditions that are characterized by a continuing (spontaneous and/or evoked) regional pain that is seemingly disproportionate in time or degree to the usual course of any known trauma or other lesion. The pain is regional (not in a specific nerve territory or dermatome) and usually has a distal predominance of abnormal sensory, motor, sudomotor, vasomotor, and/or trophic findings. The syndrome shows variable progression over time.”2
- There are two subtypes of CRPS.1
- Type I CRPS (previously known as reflex sympathetic dystrophy) occurs in patients without evidence of peripheral nerve injury and represents approximately 90% of cases.
- Type II CRPS (previously known as causalgia) occurs when peripheral nerve injury is present.
- Clinically, they are indistinguishable and follow a regional rather than dermatomal or peripheral nerve distribution.3
- CRPS is further subdivided into “warm” or “cold,” and “sympathetically maintained or sympathetically independent,” which affect prognosis and treatment options.3
- The exact pathogenesis of CRPS remains unknown.1,3 Proposed mechanisms include:
- Inflammatory changes with the release of inflammatory mediators (tumor necrosis factor-alpha, interleukin 1b, 2, and 6) and pain-producing peptides (bradykinin, substance P, calcitonin gene-related peptide) by peripheral nerves
- Immunologic changes with autoantibodies against beta-2 adrenergic receptors, alpha 1a adrenergic receptors, and muscarinic-2 receptors
- Peripheral sensitization of the nervous system is triggered by the release of proinflammatory mediators.
- Central sensitization and maladaptive changes in pain perception at the central nervous system level. Increased excitability of the secondary dorsal horn neurons often occurs.
- Autonomic changes result from catecholamine hypersensitivity.
Epidemiology and Inciting Factors
- The estimated incidence of CRPS in the United States is 5-26 per 100,000 per year.
- CRPS is much more prevalent in women, with estimates of 2-4 times the rate in men. The incidence is highest in postmenopausal females.1
- The most common inciting factors for CRPS are fractures, crush injuries, sprains, surgeries, or carpal tunnel syndrome.1-3
- Other risk factors include fibromyalgia, rheumatoid arthritis, and psychological factors (depression and/or posttraumatic stress disorder).1,2
- The impact of genetics is unclear.3
Clinical Presentation
The main clinical findings of CRPS are listed below:
Pain
• Pain is the most common and debilitating symptom of CRPS. It is often described as a burning, stinging, or tearing sensation that is felt deep within the extremity in most cases.1
• The pain is often continuous and undulating but can be paroxysmal.
• It may be worse at night and exacerbated by limb movement, contact, heat/cold, or stress.1
• The pain is not restricted to a specific nerve territory or dermatome, is disproportionate to the degree of tissue injury, and persists beyond the normal expected time for tissue healing.
Sensory Abnormalities
• Hyperalgesia: increased sensitivity to pain; usual painful stimuli cause exaggerated pain.
• Allodynia: pain is experienced in response to stimuli that are typically not painful (light touch, temperature changes, etc.).
• Hypesthesia: decreased capacity for physical sensation
• These sensory disturbances are usually distal in the extremity, often in a glove/stocking pattern.
Motor Symptoms
• Decreased grip strength or tip-toe standing is present in approximately two-thirds of patients with CRPS.
• Limb movement may be limited by pain, edema, or contractures.
• Central manifestations such as tremors, myoclonus, or dystonic postures may occur.
Autonomic Changes
• The most common are skin color changes (mostly livedo or hyperemia), edema, and increased sweating.
• A temperature difference between the affected and unaffected sides may be seen.
• Other skin changes include increased hair growth, increased or decreased nail growth, and skin atrophy.
• Joint contractures may be seen.

Figure 1. Asymmetric edema and discoloration in the right leg of a patient with CRPS. Used with permission from Weinstock LB, et al. A&A Practice. 2016; 6(9):272-6.
Diagnosis
- The diagnosis of CRPS is primarily based on a thorough history and physical examination.
- The Budapest consensus criteria for the clinical diagnosis of CRPS are as follows.2
- 1. Continuing pain, which is disproportionate to any inciting event
- 2. For the clinical diagnosis of CRPS, the patient must report at least one symptom in three of the following four categories:
- Sensory: Reports of hyperesthesia and/or allodynia
- Vasomotor: Reports of temperature asymmetry and/or skin color changes and/or skin color asymmetry
- Sudomotor/edema: Reports of edema and/or sweating changes and/or sweating asymmetry
- Motor/trophic: Reports of decreased range of motion and/or motor dysfunction (weakness, tremor, dystonia) and/or trophic changes (hair, nail, skin)
- 3. For the clinical diagnosis of CRPS, the patient must display at least one sign at the time of evaluation in two of the four following categories:
- Sensory: Evidence of hyperalgesia (to pinprick) and/or allodynia (to light touch and/or temperature sensation and/or deep somatic pressure and/or joint movement)
- Vasomotor: Evidence of temperature asymmetry (>1°C) and/or skin color changes and/or asymmetry
- Sudomotor/edema: Evidence of edema and/or sweating changes and/or sweating asymmetry
- Motor/trophic: Evidence of decreased range of motion and/or motor dysfunction (weakness, tremor, dystonia) and/or trophic changes (hair, nail, skin)
- 4. There is no other diagnosis that better explains the signs and symptoms.
- There is no gold-standard test for confirming the diagnosis. Nonetheless, certain testing measures have been proven useful.
- Triple-bone scans illustrating increased radiotracer uptake in joints distant from the trauma site.1
- Side-by-side plain radiographs illustrating patchy osteoporosis.1
- Skin temperature measurements show a temperature difference of more than 1°C between the affected and unaffected sides.1
- Increased resting sweat output1
- Testing obtaining abrupt transient relief from pain and dysesthesia with a systemic chemical sympatholysis (i.e., a “Bier block”).1 However, the role of the sympathetic nervous system in the pathogenesis of CRPS remains unclear. Thus, a positive test is no longer considered a diagnostic indicator of CRPS.1 Rather, this response is an important indicator of sympathetically maintained pain.
- Although these tests mentioned above may support the diagnosis of CRPS, they are rarely implemented; the diagnosis of CRPS is largely clinical and one of exclusion.3
Treatment
- A multidisciplinary approach is suggested for the management of CRPS. The goals of therapy include restoring function, reducing pain and disability, and enhancing quality of life while minimizing medication side effects.5
- Treatment is most successful when implemented early in the disease course.5 Table 1 illustrates the different treatment options for CRPS.
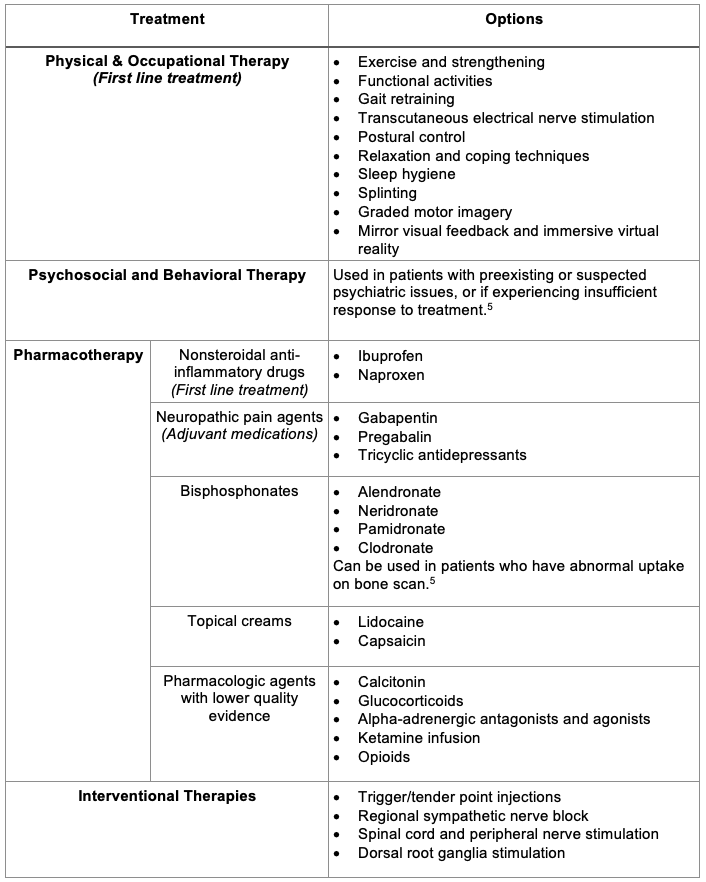
Table 1. CRPS treatment options
References
- Salahadin A. Complex regional pain syndrome in adults: Pathogenesis, clinical manifestations, and diagnosis. In: Post T, ed. UpToDate; 2024. Accessed on April 5th, 2025. Link
- Harden RN, Bruehl S, Stanton-Hicks M, et al. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med. 2007; 8(4): 326-31. PubMed
- Dey S, Guthmiller KB, Varacallo M. Complex regional pain syndrome. In: StatPearls (Internet). Treasure Island, FL. 2025. PubMed
- Taylor S, Noor N, Urtis I, et al. Complex regional pain syndrome: A Comprehensive Review. Pain and Therapy. 2021;10(2): 875–92. PubMed
- Salahadin A. Complex regional pain syndrome in adults: Treatment, prognosis, and prevention. In: Post T, ed. UpToDate; 2024. Accessed on April 5th, 2025. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.