Copy link
Cirrhotic Cardiomyopathy: Anesthetic Considerations
Last updated: 08/20/2025
Key Points
- Cirrhotic cardiomyopathy (CCM) is defined as the syndrome of cardiac dysfunction that arises in the context of cirrhosis or chronic liver disease (CLD) and occurs in the absence of pre-existing cardiac disease.
- The pathophysiology is characterized by a chronic hyperdynamic circulatory state that results in both diastolic and systolic dysfunction.
- There are no validated or universally accepted diagnostic tests for CCM.
- Management strategies are predominantly supportive and directed toward mitigating cardiac dysfunction, while liver transplantation remains a treatment option in patients with advanced liver disease refractory to medical management.
Introduction
- As cirrhosis or CLD progresses, patients frequently develop portal hypertension, which contributes to the establishment of a persistent hyperdynamic circulatory state. Over time, this hemodynamic burden imposes chronic strain on the heart, potentially culminating in cardiac dysfunction and, in some cases, overt heart failure.
- The diagnosis of CCM is inherently challenging, as patients are often asymptomatic at rest. Subclinical cardiac dysfunction is likely prevalent to varying degrees in most individuals with advanced cirrhosis or CLD. Diagnostic evaluation typically involves echocardiography to assess both diastolic and systolic performance, in addition to electrocardiographic studies and measurement of cardiac biomarkers.1,2
Pathophysiology (Figure 1)
Hyperdynamic Circulation
- In patients with cirrhosis or CLD, a hyperdynamic circulation develops secondary to portal hypertension, which arises from the distortion of liver architecture and compromised hepatocyte function.
- Enhanced production of vasodilatory mediators combined with diminished responsiveness to vasoconstrictors leads to general hypotension and vasodilation along with splanchnic vascular congestion.
- The effective arterial blood volume declines as a consequence, stimulating activation of the renin-angiotensin-aldosterone system and promoting sodium and water retention. The hypotension also activates the sympathetic nervous system (SNS).
- The result is a hyperdynamic state marked by increased cardiac output (CO), expanded plasma volume, decreased systemic vascular resistance, and continued low blood pressure. Over time, this sustained condition contributes to cardiac stress and eventual myocardial remodeling.2,3
Diastolic Dysfunction
- Often the earliest manifestation of CCM, diastolic dysfunction is characterized by impaired ventricular relaxation and increased myocardial stiffness. These changes are typically driven by myocardial hypertrophy, fibrosis, and subendothelial edema. As a result, the stiffened ventricular chamber requires elevated diastolic pressures to sustain adequate filling and for the maintenance of CO.1
Systolic Dysfunction
- Often subtle and may only become evident during conditions of stress such as physical exertion, pharmacologic stimulation, or surgery. It is characterized by a blunted contractile response to stress, reduced beta-adrenergic receptor sensitivity, increased parasympathetic tone, and excessive vasodilation driven by mediators like nitric oxide, carbon monoxide, interleukin-6, tumor necrosis factor-alpha, and endocannabinoids.3
Prolonged QT Interval
- Around 50% of patients with cirrhosis or CLD experience a prolonged QT interval. This is often due to increased SNS activity and electrolyte imbalances – particularly hypokalemia, hypomagnesemia, and hyponatremia – often present in advanced liver disease. These conditions can interfere with cardiac repolarization, increasing the risk of ventricular arrhythmias.
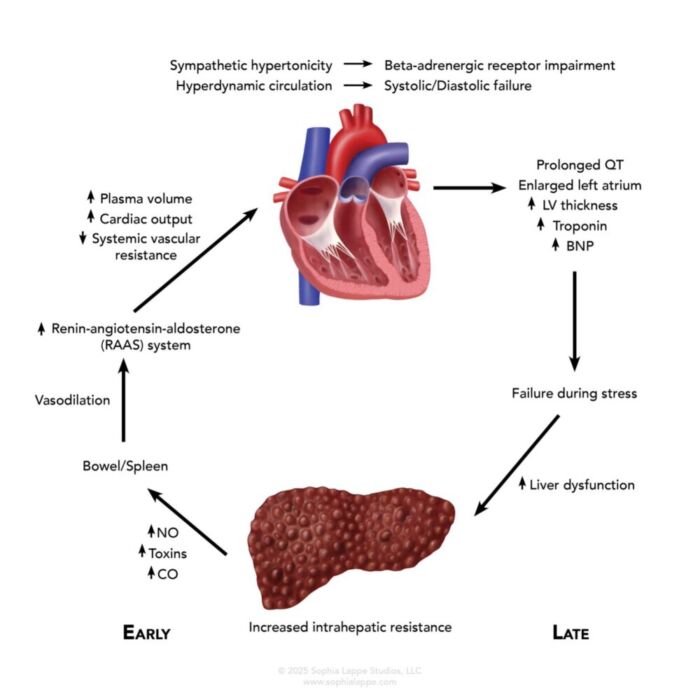
Figure 1. Cirrhotic cardiomyopathy: Destruction of hepatic architecture causes a spiral of worsening hepatic and cardiac function. Abbreviations: NO, nitric oxide; CO, carbon monoxide; LV, left ventricle; BNP, brain natriuretic peptide.
Clinical Features
- Patients with CCM are typically asymptomatic at rest but can become fatigued with physical activity or other stressors such as infections, hemorrhage, or surgery.
- They often exhibit a baseline hyperdynamic state characterized by an increased cardiac output with a reduced systemic vascular resistance, leading to hypotension.
- In many cases, typical cardiac stressors (e.g., infection and exercise) fail to trigger an appropriate increase in heart rate.
Diagnosis
- Diagnostic Criteria
- Clinical evaluation: Patients typically present with exercise intolerance that can progress to heart failure symptoms such as dyspnea and fatigue.
- Echocardiography: Transthoracic echocardiography (2-D and Doppler) can be used to assess cardiac function.
- Systolic function can be evaluated using speckle-tracking echocardiography, which measures global longitudinal strain to assess the ventricle’s ability to contract.
- Diastolic function is assessed using Doppler ultrasound techniques to measure blood and tissue velocities during diastole, and to calculate E/A or E/e’ ratios.
- The Cirrhotic Cardiomyopathy Consortium (CCM) has published criteria for diagnosis.2,4
- Biomarkers: Elevated serum levels of N-terminal pro-BNP, a precursor of brain natriuretic peptide, and troponin indicate ongoing myocardial injury or strain.
- Electrocardiography (ECG): QT interval prolongation is observed in about 50% of patients with CCM and correlates with the severity of the cirrhosis or CLD. While dysrhythmias are uncommon, they can be serious when present.
General Management
- Managing CCM is challenging due to its close association with the broader spectrum of cirrhosis and CLD. There are no disease-specific treatments, and management is largely supportive and symptom-driven.
- Volume management: Fluid and sodium restriction, along with diuretic therapy, is used to control volume overload. Long-term diuretic use must be monitored closely to avoid electrolyte imbalances and the risk of acute kidney injury.
- Symptom relief: Oxygen therapy may help alleviate symptoms of dyspnea and fatigue.
- Beta-blockers: Nonselective beta-blockers – such as propranolol, nadolol, and carvedilol – have been effectively used for decades to manage portal hypertension and prevent variceal bleeding in patients with cirrhosis and CLD. However, their use specifically for the treatment of CCM remains controversial.
- Experimental therapies: Animal studies have identified several potential therapeutic options, including anti-inflammatories, antioxidants, and anti-apoptotic agents, which have not yet translated into clinical practice.5
- Liver transplantation: A successful transplant may address the cardiac-associated issues in CLD. However, the decision to undertake this hazardous procedure must carefully weigh the cardiovascular risks, especially given the already compromised heart function in these patients.
Anesthetic Considerations
- Patients with CCM frequently undergo procedures related to cirrhosis and CLD such as transjugular intrahepatic portosystemic shunt placement, paracentesis and other interventions for portal hypertension. Anesthetic management in these patients requires careful attention to both cardiac and hepatic function, with special focus on hemodynamic stability.
Preoperative Assessment
- Cardiac Evaluation: Screening should be undertaken for signs of heart failure, arrhythmias, and reduced ejection fraction. Echocardiography is useful to evaluate both systolic and diastolic function.
- Liver Function: Liver function tests and coagulation status should be reviewed. It is also prudent to assess for complications such as ascites or encephalopathy, which could affect anesthetic choices.
- Hemodynamic Instability: Due to baseline hyperdynamic circulation with poor compensatory mechanisms, these patients are at risk for both hypotension and fluid overload.
Anesthetic Technique
- General Anesthesia: Volatile and intravenous agents should be used cautiously. Drugs that significantly depress myocardial contractility (e.g., high doses of volatile agents, opioids and benzodiazepines) should be avoided. Propofol is often preferred as because of its predictable pharmacokinetic profile.
- Regional Anesthesia: This technique may be used carefully in stable patients, but the hypotension associated with sympathetic blockade can be problematic. Epidural anesthesia, while effective for pain management, may cause significant hypotension.
- Vascular Tone and Fluid Management
- These patients often have impaired vascular tone, so vasopressors (e.g., norepinephrine and vasopressin) may be needed to maintain an adequate blood pressure.
- Fluid balance is delicate: over-resuscitation can worsen ascites or push the patient into pulmonary congestion or heart failure. Maintaining normovolemia is key.
Monitoring and Postoperative Care
- Hemodynamic monitoring: Continuous blood pressure and ECG monitoring are essential. Invasive arterial lines and central venous access may be necessary in higher-risk patients.
- Postoperative management: Delayed emergence from anesthesia may occur due to both hepatic dysfunction (slower drug clearance) and myocardial dysfunction. Close monitoring in a high-acuity setting (e.g., a step-down unit or intensive care unit the duration of the postoperative phase is recommended.
- Risk of arrhythmias
- In patients with cirrhosis and CLD, electrolyte disturbances are common, and the risk is subsequently higher for arrhythmias. Continuous ECG monitoring with aggressive electrolyte correction is a key component of perioperative management.
References
- Møller S, Henriksen JH. Cirrhotic cardiomyopathy. J Hepatol. 2010;53(1):179-190. PubMed
- Ndakotsu A, Nduka TC, Agrawal S, Asuka E. Cirrhotic cardiomyopathy: comprehensive insights into pathophysiology, diagnosis, and management. Heart Fail Rev. 2025;30(4):739-748. PubMed
- Ruiz-del-Árbol L, Serradilla R. Cirrhotic cardiomyopathy. World J Gastroenterol. 2015;21(41):11502-11521. PubMed
- Izzy M, VanWagner LB, Lin G, et al. Redefining cirrhotic cardiomyopathy for the modern era. Hepatology. 2020; 71(1):334-345. PubMed
- Liu H, Ryu D, Hwang S, Lee SS. Therapies for cirrhotic cardiomyopathy: Current perspectives and future possibilities. Int J Mol Sci. 2024;25(11):5849. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.