Copy link
Chronic Pain: Definition and Biopsychosocial Model of Pain
Last updated: 04/03/2023
Key Points
- Pain is a subjective experience, modulated by a complex interaction of a wide range of factors, not just nociceptive signaling.
- A thorough pain history is essential to delineate potential causes, red flag symptoms, indicated testing and imaging, as well as guide treatment plans.
- The gold standard of chronic pain rehabilitation is the multidisciplinary approach, including medical, psychological, and functional evaluations and treatments. The goal of pain rehabilitation is to decrease functional disability.
Definition of Pain
- In 2020, the International Association for the Study of Pain (IASP) revised and expanded the definition of pain to convey the complexities of pain, as well as improve the assessment and management of pain. The revised version defines pain as “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.”1,2
- Six key notes and etymology were added for further valuable context:1,2
- Pain is always a personal experience, influenced by biological, psychological, and social factors.
- Pain and nociception are different phenomena. Pain cannot be inferred solely from activity in sensory neurons.
- Through life experiences one learns the concept of pain.
- Although pain serves an adaptive role, it may have adverse effects on function and social and psychological well-being.
- Verbal description is only one of several behaviors to express pain. Inability to communicate does not negate the possibility of one experiencing pain.
- Chronic pain is defined as pain lasting greater than 3 months, exceeding the normal course of tissue healing, and frequently is a combination of different categories of pain.
- A recent study utilizing the National Health Interview Survey found that 20.5% of adults in the U.S. reported pain on most days or every day. The most common areas of pain were hip, knee or foot and low back pain.3
- Chronic pain results in significant functional limitation, substantial economic burden through lost days of work and medical utilization.
- Pain is categorized as nociceptive (from tissue injury), neuropathic (from nerve injury), and nociplastic (from a sensitized nervous system).4
Evaluation
- Pain evaluation is inherently subjective. A thorough exploration of pain history is essential to delineate potential causes, focus the physical exam, identify red flags to determine any indicated testing/imaging or consultations.
Pain-Targeted Assessment
- Pain intensity (i.e., numeric rating scale)
- Description of pain: onset, course (gradual/sudden), location, quality, intensity, areas of referred pain, temporal description (i.e., worse at night, constant), duration.
- History of illness, injury, or event around onset of pain
- Associated symptoms, aggravating/alleviating factors
- Previously utilized therapies, medications, and outcomes of such
- Effect on function (i.e., activities of daily living, work, school, sleepy, quality of life)
- Family history of pain, pain-related disorders/diseases, and disability
Red Flags Signs and Symptoms
- Weight loss
- Unexplained fever
- History of neoplasm
- Chronic steroid use
- Erythema, edema of joint
- Joint instability
- Pain waking up patient at night
- Morning stiffness
- Pain improves with activity
- Radicular pain not responding to conservative treatment
- Derangements of bowel/bladder function
- Neurologic changes, i.e., difficulty walking, foot drop, weakness, loss of reflexes, sensory changes, saddle anesthesia.
Biopsychosocial Model of Pain
- The biopsychosocial model of pain postulates that there is a multidimensional and complex inter-relationship between the biological, psychological, and social factors and their influence, as well as perpetuation of pain and disability (Figure 1).4
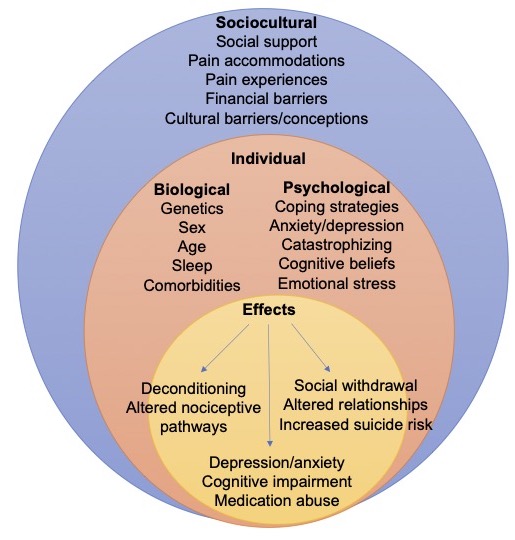
Figure 1. Biopsychosocial model of pain
Management
- The gold standard for the treatment of chronic pain is a multidisciplinary approach based on the biopsychosocial model. The purpose of the multidisciplinary approach is to address factors that modulate pain, with the goal of increasing a patient’s function, resulting in modulation of pain signaling, decrease pain intensity and increase in quality of life.4
- The main components of the multidisciplinary approach include:
- Pharmacotherapy: neuromodulating medications, antidepressants, muscle relaxants, nonsteroidal anti-inflammatory drugs, acetaminophen, opioids
- Interventional procedures
- Restorative therapies: physical therapy, exercise
- Pain-focused psychology: cognitive behavioral therapy, meditation
- Integrative and complementary therapies: massage, acupuncture
References
- International Association for the Study of Pain Terminology Working Group. Definition of pain. IASP. Published 1994. Updated 2022. Accessed December 21, 2022. Link
- Raja SN, Carr DB, Cohen M, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain.2020;161(9):1976-82. PubMed
- Yong RJ, Mullins PM, Bhattacharyya N. Prevalence of chronic pain among adults in the United States. Pain. 2022;163(2): e328-e332. PubMed
- Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. Lancet. 2021; 397(10289): 2082-97. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.