Copy link
Cardiac Implantable Electronic Devices: Internal Cardioverter-Defibrillators
Last updated: 08/20/2025
Key Points
- Similar to permanent pacemakers, the internal cardioverter-defibrillator (ICD) is an implanted device that monitors the heart rhythm and provides pacing support if indicated.
- In addition to sensing and pacing functions, ICDs also provide antitachyarrhythmia therapies for ventricular tachycardia and fibrillation.
- Electrosurgery generates electromagnetic interference (EMI) that has the potential to trigger inappropriate ICD shocks in surgeries performed above the umbilicus.
- Antitachyarrhythmia (shock) therapy can be temporarily disabled for at-risk surgeries by either placing a magnet over the pulse generator or reprogramming the device. Magnets applied over ICDs do not alter the sensing function of the ICD.
- When disabling shock therapy for surgery is required, the decision whether to use a magnet or to reprogram the ICD is based on multiple factors, including the type of surgery, patient positioning, pacemaker dependence, and resource availability.
- Pacer-dependent patients with ICDs must have their devices reprogrammed to disable shock therapy and convert to asynchronous pacing in order to prevent both inappropriate shocking and sensing in surgeries with potential for EMI.
- Special considerations exist for patients with subcutaneous ICDs, which differ from traditional ICDs in implanted location, magnet application, and lack of pacing capabilities.
Device Overview and Indications
- The traditional ICD system consists of a pulse generator located in the left chest wall and endovascular leads that extend into the heart.
- The ICD constantly surveils for ventricular tachyarrhythmias using the endovascular leads that sense the heart’s native electrical activity.
- When the ICD detects ventricular tachycardia or ventricular fibrillation, the device initiates a preprogrammed sequence of antitachyarrhythmia therapies.
- This typically includes a burst of rapid antitachycardia pacing, followed by defibrillation if the ventricular tachyarrhythmia persists.
- The defibrillation shock is delivered through a thickened portion of the endovascular lead, often described as the shock coil.
- ICDs are indicated for both primary and secondary prevention of ventricular tachyarrhythmias.
- Patients with ICDs implanted for primary prevention typically have symptomatic heart failure with significantly reduced ejection fraction due to prior myocardial infarction or dilated cardiomyopathy.1
- The main secondary indications for ICDs include prior ventricular fibrillation arrest, hemodynamically unstable ventricular tachycardia, and ventricular tachyarrhythmia after a ST-elevation myocardial infarction.2
- In addition to defibrillation, ICDs are also capable of pacing the heart, a function similar to that of a traditional pacemaker.
Risk of EMI
- EMI can interfere with how ICDs sense native cardiac electrical activity.
- EMI can be mistakenly interpreted as ventricular tachycardia or ventricular fibrillation by an ICD during surgery, leading to inappropriate defibrillation (Figure 1).
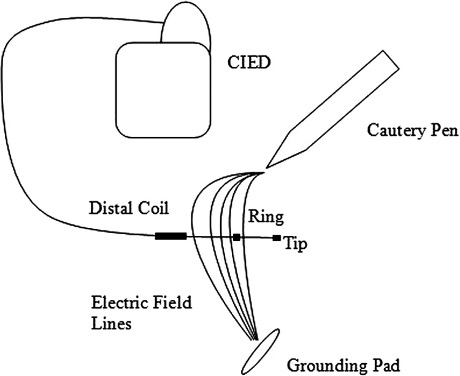
Figure 1. A diagram demonstrating how monopolar electrosurgery can generate electromagnetic interference (EMI). The electric field lines (curved lines) emitted by an electrocautery pen are shown traveling from the pen to the grounding pad. The lead from an implanted pacemaker or implanted cardioverter-defibrillator passes through this field and may perceive EMI as ventricular tachyarrhythmia, leading to inappropriate antitachyarrhythmia therapies such as rapid pacing or defibrillation. Used with permission from Suresh M, et al. Anesth Analg. 2011.
- The most common source of perioperative EMI is monopolar electrosurgery, commonly used by surgeons.
- With monopolar electrosurgery, alternating current is emitted from the electrode tip used by the surgeon to cut or coagulate tissue.
- This current is dispersed through the patient to a grounding electrode pad.
- Current crossing the path of the ICD can generate EMI (Figure 1) and lead to inappropriate sensing or shocking.
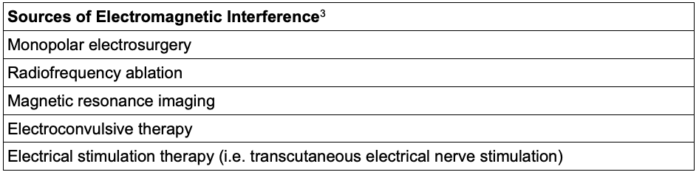
Table 1. Potential sources of electromagnetic interference in the clinical setting
- In a study investigating the risk of EMI based on the anatomical location of surgery, investigators concluded that surgeries below the umbilicus confer a minimal risk of clinically significant EMI for patients with ICDs.4
- In contrast to monopolar electrosurgery, procedures that utilize bipolar electrosurgery have a low risk of clinically significant EMI, given the minimal current dispersion associated with bipolar electrosurgery.
Perioperative Management
Preoperative Planning
- ICDs should be interrogated within 3-6 months prior to surgery, consistent with the consensus of the American Society of Anesthesiology (ASA) task force on perioperative management of patients with cardiac implantable electronic devices.5
- The ICD device interrogation report provides important information about device function, programming, and pacer-dependence (Table 2).
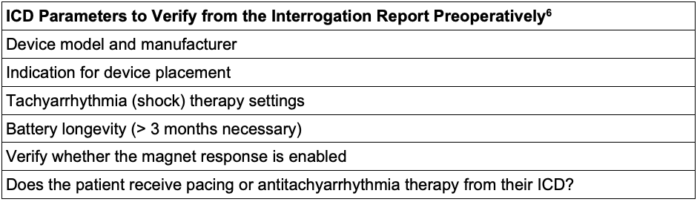
Table 2. Important ICD parameters to verify in the device interrogation report preoperatively6
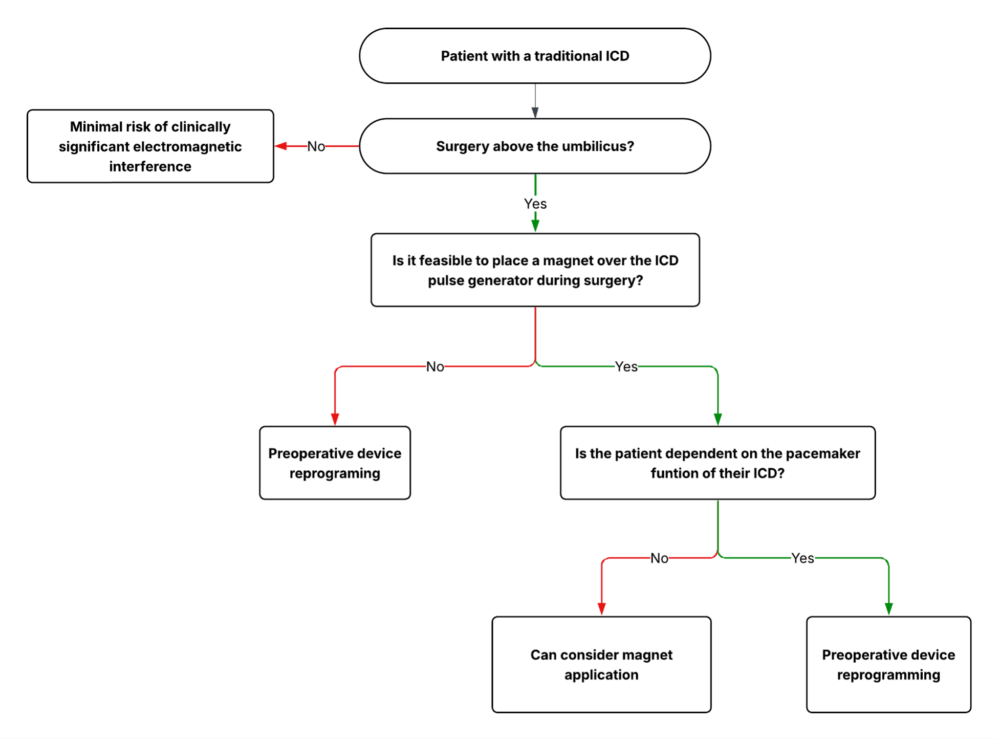
Figure 2. Algorithm for the perioperative management of traditional ICDs
Magnet Versus Reprogramming
- If medical records are unavailable, a chest radiograph can help distinguish the presence and type of ICD device.
- Determining a plan for managing perioperative EMI prior to surgery is critical (Figure 2).
- Surgeries above the umbilicus pose a risk of EMI that can trigger inappropriate shocks for patients with traditional ICDs. In addition, pacer-dependent patients with ICDs remain susceptible to inappropriate sensing from EMI.
- Disabling shock therapy can be accomplished either with preoperative device reprogramming or magnet application.
- The decision whether to use a magnet is individualized and must consider the surgical location, the patient’s history of defibrillation, any concomitant pacing requirement, and resource availability.
- Importantly, unlike pacemakers, a magnet does not convert the ICD to an asynchronous pacing mode.
- Patients who are dependent on the pacing function of their ICD require device reprogramming, rather than magnet application.
- Of note, anytime the ICD defibrillation function is programmed off, external defibrillation pads and supplies should be placed on the patient or made immediately accessible.
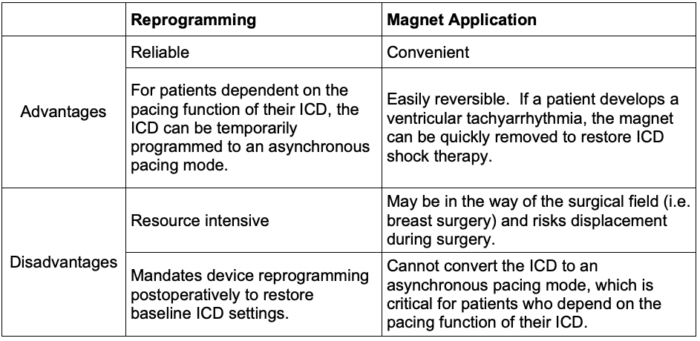
Table 3. Considerations for using a magnet versus reprogramming an ICD prior to surgery
Postoperative Management
- The ASA and Heart Rhythm Society guidelines recommend interrogating a device within one month following surgery.6
- Certain situations merit immediate postoperative interrogation, including external cardioversion or defibrillation, transcutaneous pacing, and emergency surgery where preoperative interrogation was not possible.
ICD Malfunction
- There are multiple causes of unexpected ICD failure, including lead migration, lead fracture, and battery malfunction.
- ICD malfunction can cause two critical issues: failure to defibrillate when indicated and inappropriate defibrillation.
- In some instances, inappropriate defibrillation may occur when the ICD senses rapid supraventricular rhythms, including atrial fibrillation and supraventricular tachycardia.
ICD Lead Removal Complications
- Serious problems related to an ICD lead, including infection, lead fracture, and significant venous obstruction, can necessitate the extraction of a lead.
- Lead extraction is associated with rare, yet highly morbid complications including myocardial rupture, tamponade, and damage to the tricuspid valve.
- Risk factors for life-threatening ICD removal complications include longer lead implant duration, lack of operator experience, and the need to extract more than 3 leads.
- High-risk ICD lead extractions are typically performed in the operating room under general anesthesia to facilitate transesophageal echocardiography monitoring for complications.
Novel Subcutaneous ICDs
- To avoid the known complications associated with traditional endovascular ICD leads (vessel stenosis, infection), a novel “subcutaneous ICD” has been developed over the past decade.
- The subcutaneous ICD employs a single lead in the subcutaneous tissue superficial to the sternum, obviating the need for endovascular leads.
- Because the subcutaneous ICD lead is not in direct contact with the heart, the system must simulate a surface-level electrocardiogram to monitor intracardiac electrical activity.
- This broader sensing “antenna” generally renders subcutaneous ICDs more susceptible to the effects of electromagnetic interference.
- There is minimal clinical evidence to guide the perioperative management of subcutaneous ICDs.
- At a minimum, surgeries above the groin should be considered to have a risk of clinically significant EMI.7
- Unlike traditional ICDs, subcutaneous ICDs are not capable of providing long-term pacing.
References
- Yehya A, Lopez J, Sauer AJ, et al. Revisiting ICD therapy for primary prevention in patients with heart failure and reduced ejection fraction. JACC Heart Fail. 2025;13(1):1-13. PubMed
- Kusumoto FM, Calkins H, Boehmer J, et al. HRS/ACC/AHA expert consensus statement on the use of implantable cardioverter-defibrillator therapy in patients who are not included or not well represented in clinical trials. Circulation (New York, NY). 2014;130(1):94-125. PubMed
- Stuhlinger M, Burri H, Vernooy K, et al. EHRA consensus on prevention and management of interference due to medical procedures in patients with cardiac implantable electronic devices. Europace. 2022;24(9):1512-1537. PubMed
- Schulman PM, Treggiari MM, Yanez ND, et al. Electromagnetic interference with protocolized electrosurgery and dispersive electrode positioning in patients with implantable cardioverter defibrillators. Anesthesiology. 2019;130(4):530-40. PubMed
- Practice advisory for the perioperative management of patients with cardiac implantable electronic devices: Pacemakers and implantable cardioverter–defibrillators 2020: An updated report by the American Society of Anesthesiologists task force on perioperative management of patients with cardiac implantable electronic devices. Anesthesiology (Philadelphia). 2020;132(2):225-52. Link
- Crossley GH, Poole JE, Rozner MA, et al. The Heart Rhythm Society (HRS)/American Society of Anesthesiologists (ASA) expert consensus statement on the perioperative management of patients with implantable defibrillators, pacemakers and arrhythmia monitors: facilities and patient management this document was developed as a joint project with the American Society of Anesthesiologists (ASA), and in collaboration with the American Heart Association (AHA), and the Society of Thoracic Surgeons (STS). Heart Rhythm. 2011;8(7):1114-54. PubMed
- Thompson A, Fleischmann KE, Smilowitz NR, et al. 2024 AHA/ACC/ACS/ASNC/HRS/SCA/SCCT/SCMR/SVM Guideline for Perioperative Cardiovascular Management for Noncardiac Surgery: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2024;150(19):e351-e442. doi:10.1161/CIR.0000000000001285 PubMed
Other References
- Crossley GH, Poole JE, Rozner MA, et al. The Heart Rhythm Society (HRS)/American Society of Anesthesiologists (ASA) Expert Consensus Statement on the perioperative management of patients with implantable defibrillators, pacemakers and arrhythmia monitors: facilities and patient management this document was developed as a joint project with the American Society of Anesthesiologists (ASA), and in collaboration with the American Heart Association (AHA), and the Society of Thoracic Surgeons (STS). Heart Rhythm. 2011;8(7):1114-1154. doi:10.1016/j.hrthm.2010.12.023 PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.