Copy link
Brain Health and Postoperative Cognitive Dysfunction
Last updated: 03/08/2024
Key Points
- Postoperative cognitive dysfunction (POCD) is frequently encountered among elderly patients following surgery under general anesthesia and is associated with both short- and long-term adverse outcomes.
- Several validated screening tools exist for identifying high-risk patients during the preoperative phase. Out of all devices used, Mini-Cog is the most time-efficient tool.
- There is a lack of clinical evidence that regional anesthesia or any specific anesthetic agent can reduce the incidence of POCD.
Definition
- Cognitive impairment following surgery and anesthesia was first documented over a century ago. Cognitive issues occurring postsurgery or by anesthesia can manifest as a worsening of existing disorders such as noncommunicable diseases (NCD), onset of confusion (delirium), or the development of postoperative cognitive dysfunction (POCD).1
- The Diagnostic and Statistical Manual of Mental Disorders 5th Edition (DSM 5) outlines the criteria for diagnosing NCD:
- Mild NCD: noticeable decline in cognitive function, requiring adjustment to maintain independence in activities of daily living
- Major NCD: significant burden of cognitive impairment that results in impaired activities of daily living
- Delirium, though not explicitly defined by the DSM 5, is marked by fluctuating changes in attention, consciousness levels, and cognition that emerge rapidly within hours or days after surgery. It is often linked to surgery and anesthesia and tends to occur 24 to 72 hours postsurgery.
- POCD is one of the most common complications among the elderly undergoing surgery under general anesthesia. It does not have a definition in the DSM 5. It manifests as new-onset cognitive deficits postsurgery, typically marked by memory impairment and diminished performance on intellectual tasks, possibly lasting from months to years.
- Considering the lack of definitions, new ideas are emerging to understand the decline in health that occurs after anesthesia and surgery (Table 1).
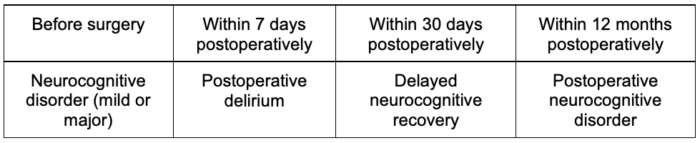
Table 1. Proposed new definitions for POCD
Incidence, Prevalence, and Outcomes
- The reported rates of POCD exhibit variation as a result of differences in research methods and cognitive assessment tools. In cardiac surgery patients, the incidence of POCD has been documented as high as 60%. A recent comprehensive review of 36 articles found that most studies with postoperative delirium (POD) occurred at rates between 10% and 15% with an incidence of 14.8%2 (Table 2).
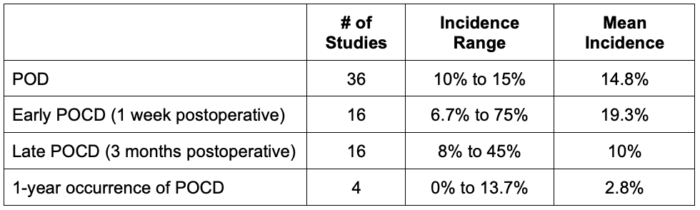
Table 2. Incidence of POD and POCD
- POD can worsen the recovery process in both the short- and long-term. Research indicates that POD is connected to increased rates of health issues and deaths, an increase in surgery complications, longer stays in intensive care units and hospitals, reduced independence, lasting disability, higher healthcare costs, and more medication use.2 Moreover, POD is tied to an increased likelihood of dementia.2
Screening and Assessment Tools
- Several validated screening tools are available to evaluate multiple cognitive domains. These tools offer convenience for surgeons and anesthesiologists as they can be administered in 15 minutes or less (Table 3 and 4).
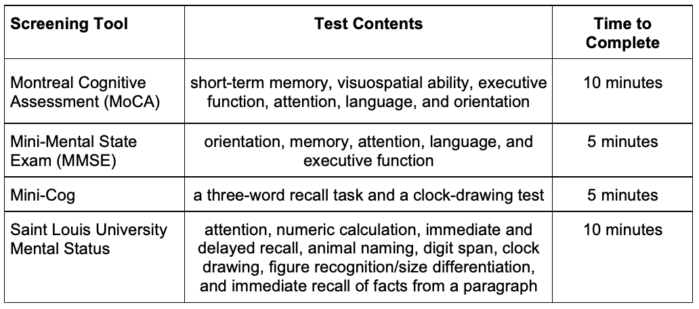
Table 3. Preoperative screening tools
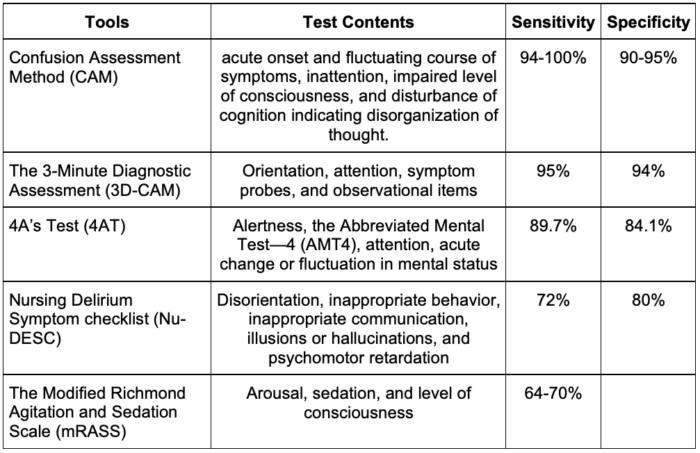
Table 4. POCD assessment tools
Assessment of Delirium Severity (Table 5)
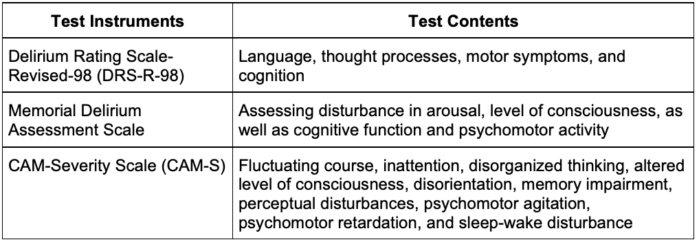
Table 5. Assessment of delirium severity
- The CAM-S scores had a strong association with important clinical outcomes related to delirium, such as length of stay, hospital expenditures, placement in nursing homes, and mortality rates.
Anesthesia and POCD
- The topic of whether anesthesia may play a role in the development of dementia has been receiving increased attention. Despite studies on the subject, a firm answer is still not clear.
General Anesthesia vs Regional Anesthesia
- In a trial involving 950 patients undergoing hip fracture surgery across multiple centers, POD was observed in 29 individuals (6.2%) in the regional anesthesia (RA) group and 24 individuals (5.1%) in the general anesthesia (GA) group (unadjusted risk difference [RD], 1.1%; 95% CI, 1.7% to 3.8%; P =.48; unadjusted relative risk [RR] 1.2 [95% confidence interval [CI], 0.7 to 2.0]; p =0.57).3 The study authors concluded that using anesthesia without sedation did not significantly lower the occurrence of delirium compared to general anesthesia.
- A recent systematic meta-analysis examined thirteen articles involving a total of 3,633 patients, with half in the RA group and half in the GA group. The analysis found no differences between RA and GA regarding cognitive dysfunction.4
- There is insufficient evidence that regional anesthesia can reduce the incidence of POCD.
Inhalation vs TIVA
- In this randomized clinical trial, the impact of volatile anesthesia compared to propofol-based total intravenous anesthesia (TIVA) on postoperative delirium following on-pump cardiac valve surgery was investigated. Among the 684 patients analyzed, postoperative delirium occurred in 63 out of 337 patients (18.7%) receiving volatile anesthesia, compared to 76 out of 339 patients (22.4%) receiving propofol-based TIVA (relative risk, 0.80; 95% CI, 0.55-1.16; p= 0.231).5 Thus, anesthesia maintenance with propofol-based TIVA did not lead to significantly fewer occurrences of postoperative delirium compared to a volatile agent.5
- There is insufficient evidence that TIVA can reduce the incidence of POCD.
References
- Evered L, Silbert B, Knopman DS, et al. Recommendations for the nomenclature of cognitive change associated with anesthesia and surgery. Br J Anaesth. 2018; 121: 1005e12. PubMed
- Kitsis P, Zisimou T, Gkiatas I, et al. Postoperative delirium and postoperative cognitive dysfunction in patients with elective hip or knee arthroplasty: A narrative review of the literature. Life (Basel). 2022;12(2):314. PubMed
- Li T, Li J, Yuan L, et al. Effect of regional vs. general anesthesia on incidence of postoperative delirium in older patients undergoing hip fracture surgery: The RAGA randomized trial. JAMA. 2022; 327(1):50-58. PubMed
- Viderman D, Nabidollayeva F, Aubakirova M, et al. Postoperative delirium and cognitive dysfunction after general and regional anesthesia: A systematic review and meta-analysis. J Clin Med. 2023;12(10):3549. PubMed
- Jiang JL, Zhang L, He L, et al. Volatile versus total intravenous anesthesia on postoperative delirium in adult patients undergoing cardiac valve surgery: A randomized clinical trial. Anesth Analg. 2023;136(1):60-9. PubMed
Other References
- Brain Safety: Then, Now, and Beyond. Anesthesia Patient Safety Foundation Podcast Episode #47. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.