Copy link
Blunt Cardiac Injuries
Last updated: 12/21/2022
Key Points
- Cardiac symptoms due to blunt cardiac injury (BCI) are often absent on the initial presentation and may manifest days to months after the initial injury.
- An extended focused assessment with sonography in trauma (FAST) exam, transthoracic echocardiogram (TTE), or transesophageal echocardiogram (TEE) can provide useful diagnostic information to guide the perioperative management of these trauma patients.
- Clinicians should be aware of the possibility of underlying cardiogenic shock due to BCI, which can be masked as refractory hypovolemic shock.
Epidemiology
- BCI is defined as an injury to the heart from blunt force trauma.1,2 Approximately 30,000 cases of BCI occur each year in the US.1
- The most common causes include motor vehicle collisions and falls from heights.1 Less common causes include sports trauma with associated lethal arrhythmias (commotio cordis) and acts of violence, blasts, and explosions.
- BCI symptoms range from mild to life-threatening. Most BCIs are self-limited myocardial contusions that typically resolve on their own.1 Severe BCI patients often expire at the scene of injury or before hospital arrival.1
- Among blunt chest trauma patients who arrive at hospitals, only 3.8% have identifiable BCIs.1
- BCI patients at high risk of cardiac-related death include:
- Patients with significant polytrauma (46%-76% expire from cardiac injury).1
- Trauma patients with occult BCIs requiring emergent noncardiac surgery.
Clinical Presentation
- Most patients are asymptomatic for sequelae of BCIs on initial presentation. The sequelae of BCIs may manifest days to months after injury. Therefore, clinicians need a high index of suspicion to diagnose BCIs.
- The initial evaluation may not reveal a cardiac injury due to the presence of other concomitant traumatic injuries, which often leads to a delay in the diagnosis of BCI.
- Common clinical manifestations of BCI include:1
- Heart failure
- Arrhythmias
- Pulmonary edema
- Hypotension/low cardiac output
- Symptoms of acute coronary syndrome
- Injuries that should raise suspicion for BCI include:1
- Refractory precordial pain
- Structural chest wall injuries
- Falls from > 20 feet
- Fracture of the first rib
- Multiple rib fractures
- Displaced sternal fractures
Myocardial Injuries and Mechanisms
- Blunt trauma can result in a laceration or tear in the walls of the atria, ventricles, or papillary muscles. The right ventricle and atrium are more commonly involved than the left ventricle and atrium.2
- The most common mechanism of injury is a direct impact to the anterior aspect of the chest at the end of diastole when the ventricles are maximally distended.2 Other less common mechanisms of injury include:2
- indirect or hydraulic pressure caused by a large force applied to the abdominal or extremity veins causing a massive increase in preload;
- bidirectional forces compressing the heart between the sternum and vertebral bodies;
- acceleration/deceleration forces resulting in myocardial or coronary artery injury;
- blast forces resulting in septal or ventricular rupture.
- Myocardial injuries are associated with high mortality rates. Myocardial lacerations with an intact pericardium can result in acute tamponade physiology, often necessitating a pericardiocentesis. Associated pericardial lacerations result in hemorrhage into the thoracic cavity.
- Septal injuries resulting in ventricular or atrial septal defects are rare.1,2
- Valvular injuries are also rare, with the aortic and mitral valves more commonly affected secondary to higher left-sided pressures. Rupture of the papillary muscles (most common) or chordae tendineae result in acute valvular regurgitation.1,2
- Myocardial contusions are intramural hematomas of the ventricles from blunt trauma. The clinical presentation depends on the extent of myocardial damage and ranges from minor arrhythmias to cardiovascular collapse.1
Arrhythmias
- Electrocardiographic (ECG) abnormalities are noted in 1-6% of BCI cases.1
- Atrial fibrillation is the most common arrhythmia. However, most atrial fibrillations after BCI are transient and not clinically significant. Bundle-branch block or complete heart block can occur and may be treated with a transvenous pacemaker.1
- Ventricular arrhythmias are uncommon in the hospital setting. The true incidence is possibly underreported as many patients expire on the field. Treatment includes antiarrhythmic agents, electrical defibrillation/cardioversion, and evaluation with TTE or TEE.1
- Commotio cordis are lethal arrhythmias secondary to minor blunt force trauma from projectiles and typically during sporting events. Baseballs are the most common cause. Commotio cordis is the third leading cause of death in young athletes, after hypertrophic cardiomyopathy and congenital coronary artery anomalies.1,2 Arrhythmias are induced when the projectile impacts the chest during the upslope of the T wave (repolarization), an “R on T” phenomenon. This may lead to polymorphic ventricular tachycardia, which can progress to ventricular fibrillation.
- Treatment
- Early defibrillation and cardiopulmonary resuscitation (CPR) are vital to survival.
- 40% of patients who receive early CPR (within 3 minutes) survive.
- Only 2% of patients who did NOT receive early CPR (after 3 minutes) survive.1
Workup and Imaging
- The workup of a patient with suspected BCI includes:
- ECG and cardiac enzymes (Troponin I)
- Chest x-ray
- Extended-FAST
- TTE/TEE
- Computed tomography (CT)
- Cardiac magnetic resonance imaging (MRI)
- The Eastern Association for the Surgery of Trauma made the following recommendations for the evaluation of BCI Injuries:3
- Level 1 recommendation
- An admission ECG should be performed on all patients with suspected BCI.
- Level 2 recommendations
- If the admission ECG shows a new abnormality (arrhythmia, ST changes, ischemia, heart block, etc.), the patient should be admitted for continuous ECG monitoring.
- If the patient has a normal ECG and normal troponin I level, BCI can be ruled out.
- For patients with hemodynamic instability or persistent arrhythmias, an ECG must be performed. If a TTE cannot be performed, a TEE should be considered.
- A sternal fracture alone does not predict the presence of BCI.
- Creatinine phosphokinase levels and nuclear medicine studies add little value.
- Level 3 recommendations
- Elderly patients with known cardiac disease, unstable patients, and those with an abnormal admission ECG can safely undergo surgery and should be monitored.
- Troponin I levels should be measured routinely for patients with suspected BCI. If the troponin I levels are elevated, the patient should be monitored.
- Cardiac CT or MRI can be used to help differentiate acute myocardial infarction from BCI in trauma patients with abnormal ECGs, cardiac enzymes, or echocardiograms.
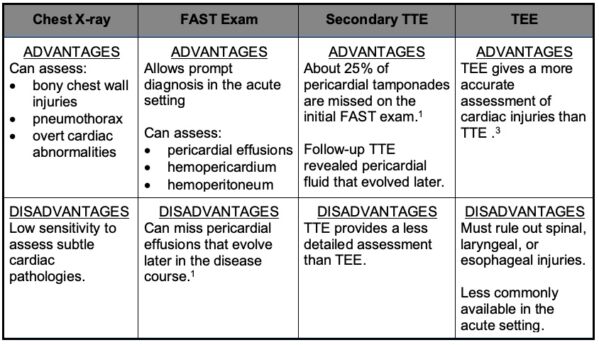
Table 1A. Advantages and Disadvantages of Imaging Modalities to Assess for BCI.
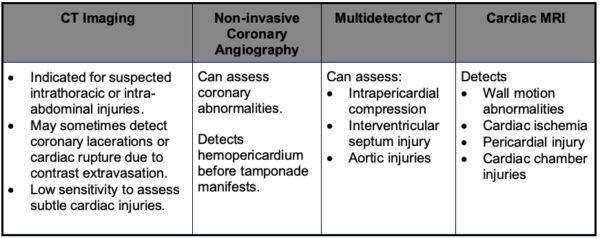
Table 1B. Utility of CT Imaging and Cardiac MRI to Assess for BCI.1
Anesthetic Considerations
- Some patients with BCI require surgical interventions for cardiac or noncardiac injuries.
- Airway management should be performed with careful consideration of associated injuries. The anesthesia team must pay attention to the hemodynamic effects of induction agents, positive pressure ventilation, and the presence of pericardial effusion/tamponade or other cardiac injuries.
- Hypovolemic shock and blood loss are common in trauma patients. Adequate vascular access and goal-directed volume resuscitation are the mainstays of treatment.
- TTE or TEE can quickly assess for cardiac injuries as the cause for refractory hypotension despite volume resuscitation.
- Inotropic support, paired with fluid resuscitation, should be initiated.
- Volume resuscitation alone, without inotropic support, can precipitate decompensated heart failure and/or hemodynamic collapse.1
- TTE or TEE can also be used to rule out cardiac injuries and guide perioperative management (Table 2).
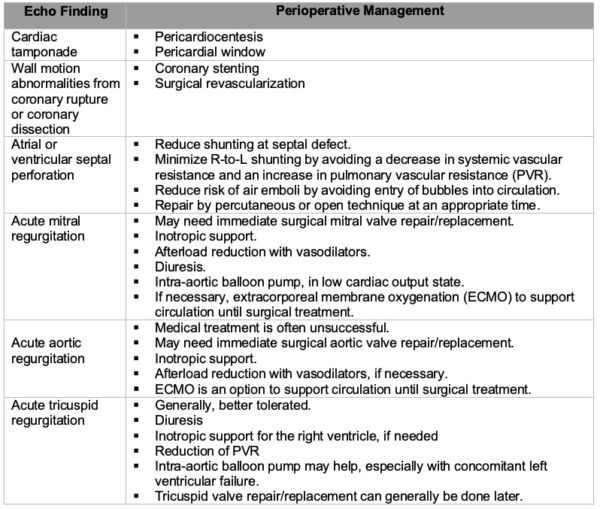
Table 2. Sequelae of BCI found on TTE/TEE and Perioperative Management
References
- Patel KM, Kumar NS, Desai RG, et al. Blunt Trauma to the Heart: A Review of Pathophysiology and Current Management. J Cardiothorac Vasc Anesth. 2022; 36 (8 Pt A): 2707-18. PubMed
- Huis in’t Veld MA, Croft CA, Hood RE. Blunt cardiac trauma review. Cardiol Clin. 2018: 36:183-91. PubMed
- Clancy K, Velopulos C, Bilaniuk JW, et al. Screening for blunt cardiac injury: An Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73: S301-6. PubMed
- Nan YY, Lu MS, Liu KS, et al. Blunt traumatic cardiac rupture: therapeutic options and outcomes. Injury. 2009; 40 (9): 938-45. PubMed
- Karalis DG, Victor MF, Davis GA, et al. The role of echocardiography in blunt chest trauma: a transthoracic and transesophageal echocardiographic study. J Trauma. 1994; 36 (1): 53-8. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.