Copy link
Beta Blockers
Last updated: 09/08/2025
Key Points
- Beta blocker medications are commonly used to treat heart conditions, such as arrhythmias, congestive heart failure, angina, and hypertension.
- Beta blockers are valuable in the treatment of conditions such as myocardial infarctions and aortic aneurysms.
- Beta blockers work by binding one or both G-protein-coupled β1 and β2-adrenergic receptors. Beta blockers that only block β1-adrenergic receptors are termed cardioselective blockers.
- Reversal of beta-blocker toxicity includes the administration of glucagon and calcium supplementation.
Introduction
- Beta blockers are β1 and β2-adrenergic receptor blockers that have been widely used for decades, with generally tolerated and well-identified side effects and a clear impact on patient outcomes.1
- Beta blockers are now less often identified as first-line for hypertension, while still remaining very commonly prescribed for cardiac conditions.2
Mechanism of Action
- Beta blockers most commonly act as a competitive antagonist to endogenous catecholamines at one or both G-protein coupled β1 and β2-adrenergic receptors.
- Blockade of β1-adrenergic receptors results in a decrease in heart rate and a reduction in the force of cardiac contractions. Normally, β1 receptors, when activated by endogenous catecholamines, stimulate the Gs protein, increasing cyclic adenosine monophosphate (cAMP) and protein kinase A (PKA) activity. This pathway will then increase heart contractility. Renin can also be released from juxtaglomerular cells in the kidney, which raises blood pressure. Beta blockers are competitive antagonists that block these pathways, reducing cardiac contractions, heart rate, and renin release.
- The β2-adrenergic receptor’s Gs, cAMP, and PKA pathway normally promotes dilation in airways and brain and skeletal muscle vasculature. Blockade of β2-adrenergic receptors by beta blockers leads to bronchoconstriction and vasoconstriction in the brain and skeletal muscle.3
Pharmacologic Properties
- Beta blockers generally have nuanced differences in their effects. Certain beta blockers are chosen based on their specific side effects and the needs of the patient.1
- Beta blockers, in general, contain an aryloxypropanolamine side chain with an aromatic ring and vary in side chains.
- Beta blockers vary in their affinity towards β1 and β2-adrenergic receptors. Those that have a specific affinity towards β1 adrenergic receptors will bind β2 when given a high enough dosage.
- Three generations of beta blockers have been released (Table 1).3
- Nonselective beta blockers
- Cardioselective beta blockers (selective β1 antagonists) help to reduce the potential for adverse effects mediated by the blockade of β2 outside the myocardium, such as cold extremities, erectile dysfunction, or exacerbation of asthma or chronic obstructive pulmonary disease.
- Beta blockers with vasodilatory properties (vasodilating beta blockers) reduce systemic vascular resistance while maintaining or improving cardiac output, stroke volume, and left ventricular function.
- The bioavailability of beta blockers varies based on lipophilicity, first-pass metabolism, renal excretion, and route of administration.
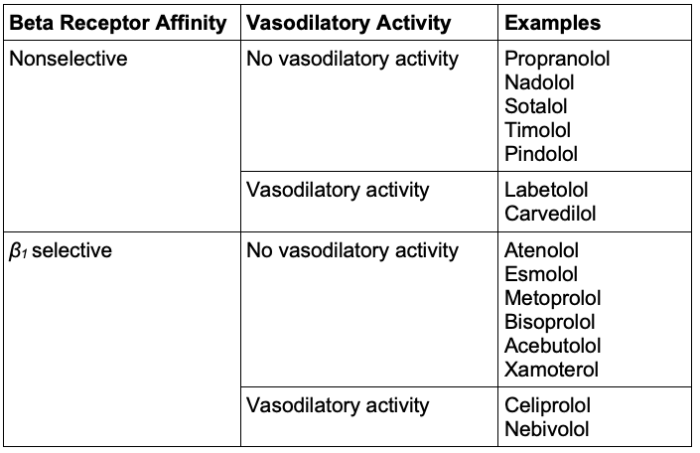
Table 1. Classification of beta blockers3
Clinical Uses
- Beta blockers are widely used to treat various heart and circulatory conditions. These include myocardial infarction, hypertension, tachycardia, arrhythmias, congestive heart failure, hypertrophic obstructive cardiomyopathy, long QT syndrome, and aortic dissection1,3 (Table 2).
- Given the availability of angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and diuretics, beta blockers are not considered first-line in the treatment of hypertension.2
- A less common use of beta blockers is to treat anxiety. While this use is not FDA-approved, beta blockers disrupt the sympathetic nervous system and may decrease anxiety-related symptoms. Propanol may be used to treat stage fright.1
- Beta blockers may also be used to treat glaucoma and migraines.1
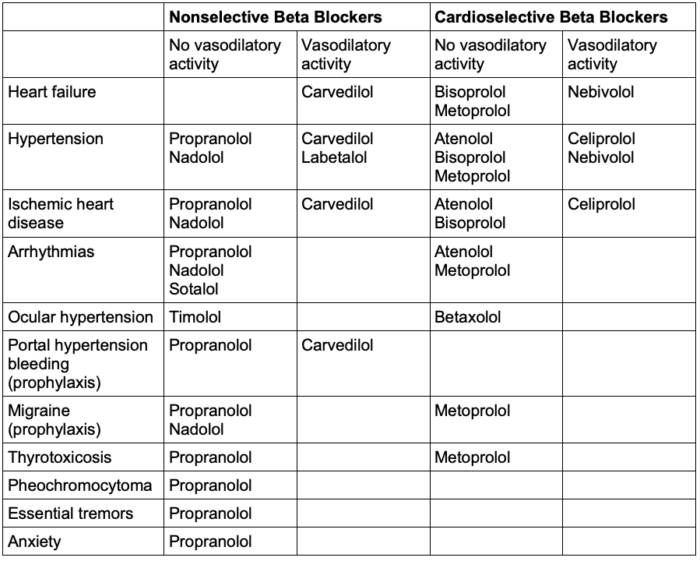
Table 2. Common indications for beta blockers3
Administration and Dosage
- Beta-blocker administration and dosage may vary significantly by use and type of drug.4
- Beta blockers may be administered orally, intravenously, in ophthalmic form, or intramuscularly.1
- Most beta blockers are given once or twice a day and have a half-life between 3 and 7 hours. Some beta blockers have a much longer half-life, such as nadolol with a half-life of 10-20 hours. Dosage may also vary greatly. Depending on the circumstance, the dosage of labetalol, used during hypertensive emergencies, may vary from 200 to 1200 mg.4
- Beta blockers are typically continued in the perioperative setting due to their ability to decrease myocardial oxygen demand, control dysrhythmias, and have a risk of withdrawal with acute discontinuation.
Adverse Effects/Toxicity
- β-adrenergic blocker activity may lead to adverse cardiac events. Inhibition of β1-adrenergic receptors can cause impairment in heart function, such as left-ventricular heart failure or heart block. Inhibition of β2-adrenergic receptors can prevent the opening of airways, leading to bronchospasm. Hypotension, bradycardia, nausea, fatigue, sexual dysfunction, and constipation may also occur.1
- Withdrawal of beta blockers may lead to increased catecholamine sensitivity, arrhythmias, and hypertensive crises.1
- Certain beta blockers, such as sotalol, may cause QT prolongation and increase the risk of torsade de pointes.1
- Reversal of a beta blocker overdose typically consists of intravenous glucagon administration and calcium supplementation.
Contraindications
- Nonselective beta blockers are contraindicated in asthmatic patients due to β2-adrenergic blockage-induced bronchoconstriction.1
- Beta blockers are contraindicated in anyone with chronic hypotension or bradycardia.1
References
- Farzam K, Jan A. Beta blockers. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. PubMed
- Chan YS, Krumholz HM, Suchard MA, et al. Comprehensive comparative effectiveness and safety of first-line β-blocker monotherapy in hypertensive patients: A large-scale multicenter observational study. Hypertension. 2021;77(5):1528-38. PubMed
- Oliver E, Mayor F Jr, D'Ocon P. Beta-blockers: Historical perspective and mechanisms of action. Rev Esp Cardiol (Engl Ed). 2019;72(10):853-62. PubMed
- Wood AJ. Pharmacologic differences between beta blockers. Am Heart J. 1984;108(4 Pt 2):1070-7. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.