Copy link
Basics of Palliative Care
Last updated: 09/09/2025
Key Points
- Palliative care is an interdisciplinary approach to care that provides symptom relief, support, and comfort to patients with serious illness and their caregivers.
- Palliative care encompasses various forms of support, including social, emotional, spiritual, and religious support.
- Palliative care is not the same as hospice care and can begin as early as when a patient is diagnosed with a serious illness and occur while a patient is receiving curative treatment.
- End-of-life conversations are critical conversations held between a patient and their healthcare team regarding the patient’s medical care and quality of life as they near death. Topics discussed include resuscitation, ventilators, artificial nutrition and hydration, pain control, advanced care planning, and end-of-life goals.
Introduction
- Palliative care is an interdisciplinary approach to medicine that aims to improve the quality of life of individuals with serious illnesses.
- Palliative care involves comprehensive treatment of a patient’s physiological, psychological, social, and spiritual suffering.
- Palliative care involves collaboration among physicians, nurses, social workers, chaplains, psychologists, and therapists. This team-based approach collaborates with other medical specialists, such as oncologists or organ failure experts, to ensure that all aspects of the patient’s care are well-managed and communicated effectively.
Palliative Care vs. Hospice Care
- A common misconception is that palliative care is synonymous with hospice care. The goal of both services is to improve the quality of life for seriously ill patients; however, they differ in terms of care goals, timing, service location, and insurance coverage.
- Palliative care can be utilized in both inpatient and outpatient settings.
- Early introduction to palliative care can help patients with serious illnesses discuss goals and values for care with their physicians and loved ones, address symptom management, and understand disease and treatment options.
- Most importantly, palliative care is appropriate at any age, at any stage of serious illness, and can be provided along with curative treatment.
- Inpatient palliative care involves an interdisciplinary team that works together with the primary team to provide an additional layer of support to both the patient and family caregiver.
- Outpatient palliative care is typically delivered through interdisciplinary clinics that collaborate to offer comprehensive symptom management, access to social support, and care coordination.
- While less common, in-home palliative care may also be available in select cases, often through home health agencies, but is typically more limited in scope.
- Table 1 compares palliative and hospice care.1
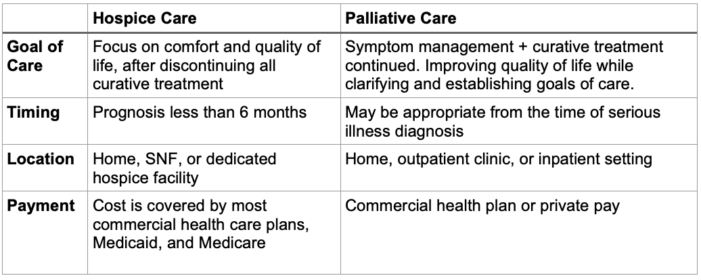
Table 1. Comparison of Palliative and Hospice Care; SNF, skilled nursing facility
- Understanding these differences ensures patients receive the appropriate care without unnecessary delays.
- Decisions regarding palliative or hospice care should involve the patient, their family, and an interdisciplinary team of medical and social professionals.
- Providing clear information and encouraging open communication allows for informed decisions with respect for the patient’s wishes.
- Understanding palliative care options early is crucial for patients to be aware of their choices and to engage in palliative or hospice care in a timely manner.2
Role of Anesthesiologists in Palliative Care
- The work of an anesthesiologist in Palliative Care encompasses palliative analgesia, regional anesthesia, and sedation, as well as the anesthesiologist’s role as an educator and advocate for the patient and their family.
- Anesthesiologists possess the expertise to manage complex pain and other distressing symptoms (such as nausea or dyspnea), to optimize a patient’s functional status, and to facilitate end-of-life care discussions.3
Advance Care Planning and Goals of Care Conversations
- Advance care planning (ACP) is a process to support patients in delineating their goals, values, and preferences regarding future medical care.
- Goals of care (GOC) conversations are critical conversations held between a patient, their loved ones, and their healthcare team regarding the patient’s goals and values in the face of serious illness.
- While ACP conversations may occur at any age or state of health, GOC conversations typically occur at transition points when a person’s health has changed and new goals need to be determined.
- These conversations may include setting treatment limitations on medical interventions such as resuscitation, mechanical ventilation, and artificial nutrition and hydration.
- It is essential to communicate openly and honestly with patients, using clear and simple language. Involving a patient’s religious or spiritual leader can help facilitate conversations. The REMAP: A Framework for Goals of Care Conversations is a tool that helps provide an understanding and adaptable method for GOC conversations.4
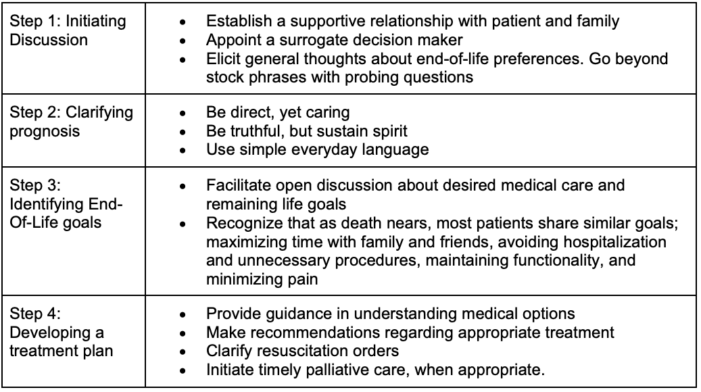
Table 2. Reference for talking about end-of-life care
When to Involve Palliative Care?
- Palliative care can be involved at any stage of a patient’s hospital course. However, the palliative care team is commonly consulted when a patient may experience complications from surgery.
- When patients are unable to wean from assistive/support devices, require increasing vasopressor support, or when the family is requesting clarification on interventions from the surgery team.
- Palliative care can also help manage symptoms. Table 3 shows common symptoms that are addressed during end-of-life care.
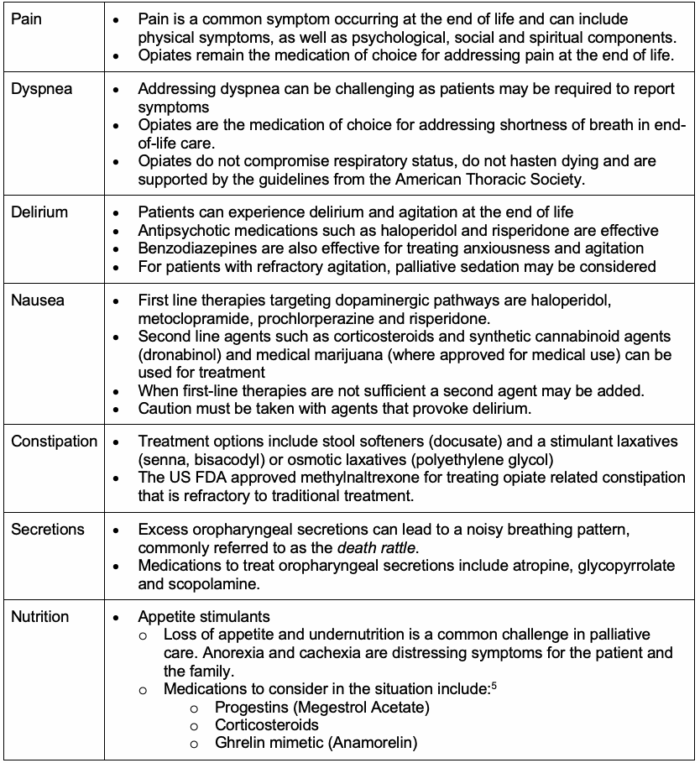
Table 3. Symptom management during end-of-life care; US FDA, United States Food and Drug Administration
Palliative Sedation
- Palliative sedation is the process of reducing a patient’s awareness of distressing symptoms through sedative medication or procedures.6 This decision should closely consider the patient’s goals, family involvement, and multidisciplinary coordination.7
- Midazolam is an effective first-line choice agent for palliative sedation.7
Support Groups
- Palliative care also addresses the psychosocial needs of patients and their families. This may include counseling to help patients and families cope with the emotional and psychological impact of the illness.
- Connecting the patient and family with support groups can provide a sense of community and shared experience.
- There may also be assistance with advance care planning to ensure the patient’s wishes and preferences are communicated and respected. Additionally, support is available to facilitate end-of-life decision-making, ensuring patients receive care that aligns with their values.
Multidisciplinary Model
- Providing comprehensive palliative care involves a multidisciplinary model where the medical team works closely with other disciplines, including nursing, social work, chaplaincy, physical therapy, occupational therapy, and nutrition. This may include counseling to help patients and families cope with the emotional and psychological impact of the illness, support groups to provide a sense of community and shared experience, and assistance with advance care planning to ensure the patient’s wishes and preferences are known and respected, as well as end-of-life decision-making to ensure the patient receives care that aligns with their values.
- Other important multidisciplinary team members and responsibilities can include:
- Outpatient center, chaplain/religious support, family/social support, oncology
- Physical Therapy/Occupational Therapy
- Palliative care interventions may also include physical therapy and occupational therapy to help maintain function, improve mobility, and enhance quality of life.
- Nutrition
- Speech therapists and nutritionists can also work closely to assess and plan feeding options. Balancing oral intake, enteral feeds (via orogastric or nasogastric tubes), and intravenous feeding with total parenteral nutrition can be used to maintain nutrition, weight, and avoid complications of severe malnutrition.
Conclusions
- Palliative care is an interdisciplinary approach to care that provides symptom relief, support, and comfort to patients with serious illness and their caregivers.
- Palliative care uses an interdisciplinary team composed of physicians, nurses, social workers, physical therapists, and champions.
- Palliative care is not the same as hospice care.
- Palliative care can begin as early as when a patient is diagnosed with a serious illness and occur while a patient is receiving curative treatment.
- Hospice care is intended when a clinical diagnosis of <6 months exists
- Palliative care can be provided at home, in an assisted living facility, an outpatient clinic, or a hospital.
- Palliative care encompasses various forms of support, including social, emotional, spiritual, and religious support.
- Palliative care can help with symptom management, including anxiety, nausea, secretions, pain, dyspnea, or constipation.
- Patients who receive palliative care support have less stress, greater satisfaction, and longer survival rates.8
References
- Buss MK, Rock LK, McCarthy EP. Understanding Palliative Care and Hospice: A Review for Primary Care Providers. Mayo Clin Proc. 2017;92(2):280-6. PubMed
- Kelley AS, Morrison RS. Palliative care for the seriously ill. N Engl J Med. 2015;373(8):747-55. PubMed
- Cotogni P, Saini A, De Luca A. In-hospital palliative care: should we need to reconsider what role hospitals should have in patients with end-stage disease or advanced cancer? J Clin Med. 2018;7(2):18. PubMed
- Childers JW, Back AL, Tulsky JA, Arnold RM. REMAP: a framework for goals of care conversations. J Oncol Pract. 2017;13(10):e844-e850. PubMed
- Childs DS, Jatoi A. A hunger for hunger: a review of palliative therapies for cancer-associated anorexia. Ann Palliat Med. 2019;8(1):50-8. PubMed
- Bruera E. Palliative sedation: when and how? J Clin Oncol. 2012;30(12):1258-1259. PubMed
- de Graeff A, Dean M. Palliative sedation therapy in the last weeks of life: a literature review and recommendations for standards. J Palliat Med. 2007;10(1):67-85. PubMed
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733742. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.