Copy link
Antiplatelet Agents
Last updated: 05/14/2025
Key Points
- There are five main categories of antiplatelet agents, including cyclooxygenase-1 (COX-1) inhibitors, P2Y12 inhibitors, glycoprotein IIb/IIIa (GP IIb/IIIa) inhibitors, phosphodiesterase (PDE) inhibitors, and protease-activated receptor-1 (PAR-1) antagonists, each with distinct mechanisms of action.
- Managing antiplatelet therapy for surgery involves assessing bleeding risk, stopping antiplatelets for high-risk procedures, and adjusting for low-risk procedures based on pharmacokinetics and patient factors.
Introduction
- Antiplatelet agents are primarily used to prevent and manage cardiovascular and cerebrovascular diseases.1
- Arterial thrombus formation heavily relies on platelet activation to generate thrombin, establish a physical barrier, and provide a base for fibrin accumulation.1
- Targeting platelet aggregation can prevent complications like acute coronary syndrome, ischemic stroke, and peripheral artery disease.1
Categories
- Clinically, five main categories of antiplatelet agents are used, alone or in combination: COX-1 inhibitors, P2Y12 inhibitors, GP IIb/IIIa inhibitors, PDE inhibitors, and PAR-1 antagonists.1
- Most antiplatelet agents are available orally except for GPIIb/IIIa inhibitors and cangrelor, a P2Y12 inhibitor, which are given intravenously (IV).2
- Oral agents are commonly used for long-term therapy, while IV agents are reserved for acute settings like during percutaneous coronary intervention (PCI).2
Mechanisms of Action
- COX-1 inhibitors (e.g., aspirin): Irreversibly inhibits COX-1, blocking thromboxane A2 (TXA2) production, which reduces platelet activation and aggregation.1,2
- P2Y12 inhibitors (e.g., clopidogrel, prasugrel, ticagrelor, ticlopidine, cangrelor): Block the P2Y12 receptor on platelets, preventing ADP-mediated platelet activation and stabilization of the platelet plug.1,2
- GPIIb/IIIa inhibitors (e.g., abciximab, eptifibatide, tirofiban): Inhibit the GPIIb/IIIa receptor on platelets, preventing fibrinogen and von Willebrand factor binding, thus inhibiting platelet cross-linking and aggregation.1,2
- PDE inhibitors (e.g., dipyridamole, cilostazol): Inhibits phosphodiesterase that results in an increase in cAMP and cGMP levels in platelets, reducing platelet activation and promoting vasodilation.1,2
- PAR-1 antagonist (e.g., vorapaxar): Block the protease-activated receptor-1 on platelets, inhibiting thrombin-induced platelet activation.1
Uses
- Prevention and management of cardiovascular events
- Primary prevention for patients at high risk of developing coronary artery disease (e.g., diabetes, hypertension, hypercholesterolemia, smoking)2,3
- Management of acute coronary syndrome, including unstable angina, non-ST elevation myocardial infarction, and ST elevation myocardial infarction2
- Postprocedural thrombosis prevention includes PCI with stenting, PCI for peripheral arterial disease, and coronary artery bypass grafting surgery (CABG)2
- Stroke and embolism prevention
- Secondary prevention after noncardioembolic stroke or transient ischemic attack2,3
- Prevention in mechanical heart valves in combination with warfarin2
- Aspirin is clinically used for conditions such as Kawasaki disease, acute pericarditis, atrial fibrillation with high stroke risk, acute rheumatic disease, and during the first six months after patent ductus arteriosus device closure.2
Complications
- The most common adverse effects of antiplatelet therapy are related to an increased risk of bleeding: 1,2
- Epistaxis
- Upper gastrointestinal bleeding, often due to chronic gastritis
- Hematuria
- Ecchymosis
- Hemorrhage
- Thrombocytopenia, including GPIIb/IIIa inhibitor-induced thrombocytopenia
- Drug-drug interactions
- Morphine: Delays the absorption of oral P2Y12 inhibitors, resulting in delayed/attenuated antiplatelet effects1
- Omeprazole: Competitively inhibits CYP2C19, interfering with the activation of clopidogrel.1
- Ibuprofen: When administered prior to acetylsalicylic acid (ASA), it binds to the catalytic site of COX-1, preventing aspirin’s antiplatelet action.1
- Statins: There is a risk of rhabdomyolysis if ticagrelor is given with an increased dose of simvastatin/lovastatin.
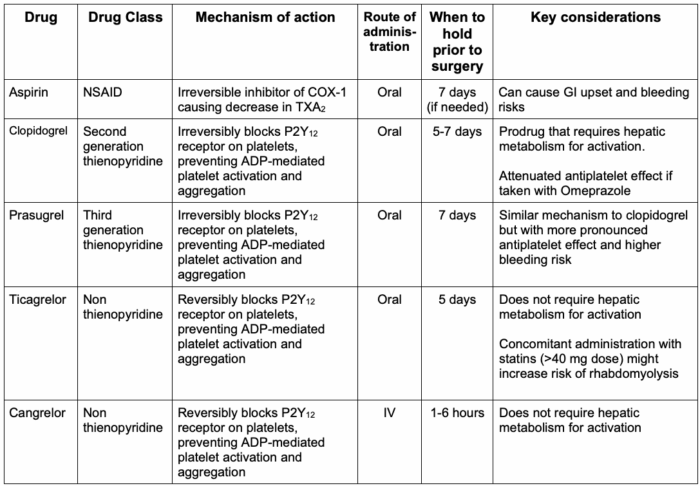
Table 1. Common antiplatelet medications
Perioperative Care
Risk Assessment
- Before initiating antiplatelet therapy, patients should be evaluated for bleeding risk factors such as impaired renal function, advanced age, and female gender.2
- Surgical factors:
- Procedures with high bleeding risk (≥2% 30-day risk) require no residual anticoagulant effect at the time of the procedure (i.e., 4-5 drug half-life interruption prior to procedure). Low to moderate bleeding risk procedures (0%-2% 30-day risk) permit some residual anticoagulant effect (i.e. 2-3 drug half-life prior to the procedure). Minimal bleeding risk procedures (~0% 30-day risk) can proceed with full anticoagulation3,4 (Table 2).
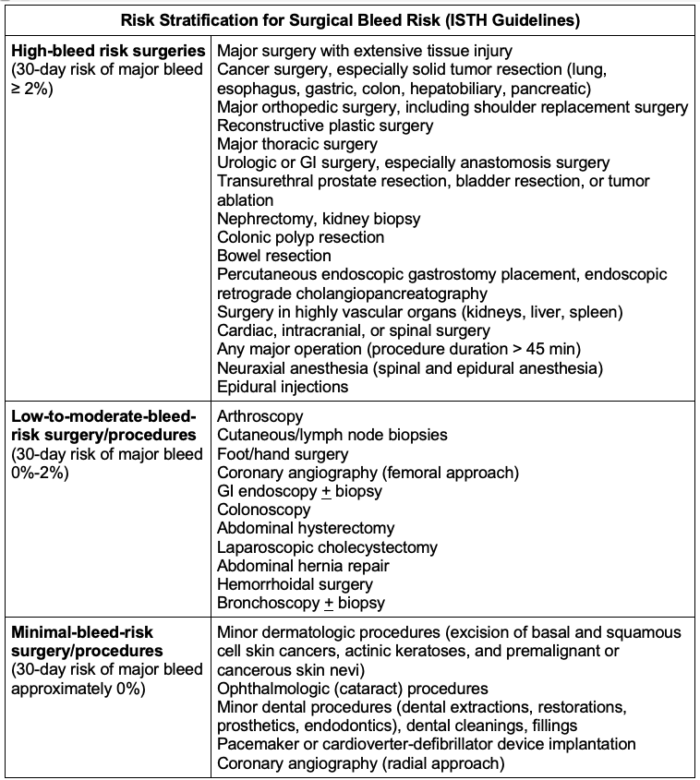
Table 2. Risk stratification for surgical/procedural bleed risk from the International Society on Thrombosis and Haemostasis (ISTH). Adapted from Spyopoulos AC, et al. J Thromb Haemost. 2019; 17(11); 1966-72.3
- Patient factors and contraindications:
- History of recurrent vascular events (e.g., stroke, intracranial hemorrhage, esophageal varices)2,4
- Bleeding history (e.g., prior perioperative hemorrhage, acute clinically significant bleed, decompensated liver cirrhosis)2
- Genetic and platelet function testing can optimize therapy by mitigating bleeding risk and guiding antiplatelet regimen adjustments.1
Management Strategies
- Noncardiac surgery
- Aspirin interruption is preferred for patients with stable coronary artery disease, no history of coronary revascularization, or undergoing high bleeding-risk surgery. Continuation is favored in patients with a history of revascularization or recent myocardial infarction (<1 year).5
- For patients who had coronary revascularization and are on dual antiplatelet therapy with aspirin and P2Y12 inhibitors, P2Y12 inhibitors are interrupted. Bridging with GPIIb/IIIa inhibitors or cangrelor is considered in high-risk cases, particularly with recent stenting (2–4 weeks).5
- Cardiac surgery
- Most guidelines suggest continuing aspirin preoperatively to reduce early thromboembolic events and mortality.6
- For elective cardiac surgery, it is recommended that P2Y12 inhibitors are stopped before surgery to reduce bleeding risks despite potential ischemic protection.5
- Timing of antiplatelet discontinuation before surgery2,5,8
- Ticagrelor: 3-5 days prior
- Clopidogrel: 5 days prior
- Prasugrel: at least 7 days prior
- Regional anesthesia
- If planning for neuraxial anesthesia and deep nerve blocks, discontinue clopidogrel and prasugrel for 7 to 10 days and ticagrelor 5 days before the procedure.6
- Superficial nerve blocks may be performed without discontinuation of antiplatelet therapy.6
- Please see the OA summary on Regional Anesthesia in Patients Receiving Antithrombotic or Thrombolytic Therapy: Part 2 for more details. Link
- Cerebrovascular patients
- Initiating dual antiplatelet therapy with ASA and clopidogrel within 24 hours reduces recurrent ischemic stroke at 90 days when continued for 21 days compared to monotherapy.4
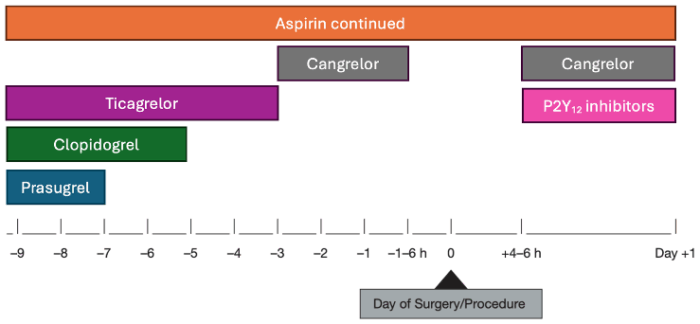
Figure 1. Perioperative management of anti-platelet drugs. Adapted from Douketis JD, et al. Perioperative management of antithrombotic therapy: An American College of Chest Physicians Clinical Practice Guideline. Chest. 2022;162(5):e207-e243.8
Legend: The decision to continue or hold aspirin and P2Y12 inhibitors depends on the surgery bleed risk assessment (Table 2).
- Aspirin and P2Y12 inhibitors can be continued perioperatively in patients undergoing minor dental, minor dermatological, and minor ophthalmologic procedures.8
- Aspirin should be continued perioperatively in patients undergoing vascular procedures (e.g., carotid endarterectomy) or in patients with a recent myocardial infarction (1 year of less) or with prior coronary revascularization.
- Aspirin interruption for 7 days is suggested for patients undergoing noncardiac surgery with stable coronary artery disease, no history of revascularization and undergoing high bleeding risk surgery.
- Aspirin should be continued in patients undergoing coronary artery bypass grafting. Meanwhile, P2Y12 inhibitors should be held perioperatively.
- Aspirin should be resumed within 24 hours after surgery.8
- Among the P2Y12 inhibitors, clopidogrel should be stopped 5 days prior, ticagrelor should be stopped 3-5 days prior, and prasugrel should be stopped 7 days prior to surgery.
- P2Y12 inhibitors can be resumed at the maintenance dose within 24 hours after surgery.8
Postoperative Care
- Antiplatelet therapy should be started quickly and safely if essential (e.g., poststenting).2
- The choice of antiplatelet agents can lead to optimal or suboptimal outcomes. The provider must consult with the pharmacist and other care team members to monitor adverse events and bleeding.2
- Strategies to enhance adherence to medication regimens include engaging in open discussions with patients to improve their understanding of the medication’s side effects and the rationale for its selection. Key factors to consider are race, language barriers, socioeconomic status, older age, and the use of multiple medications. These measures are particularly beneficial for secondary prevention of stroke and ischemic events.4
References
- Gelbenegger G, Jilma B. Clinical pharmacology of antiplatelet drugs. Expert Rev Clin Pharmacol. 2022;15(10):1177-97. PubMed
- Iqbal AM, Lopez RA, Hai O. Antiplatelet medications. In: StatPearls. Treasure Island (FL): StatPearls Publishing; November 7, 2022. Link
- Spyropoulos AC, Brohi K, Caprini J, et al. Scientific and standardization committee communication: Guidance document on the periprocedural management of patients on chronic oral anticoagulant therapy: recommendations for standardized reporting of procedural/surgical bleed risk and patient-specific thromboembolic risk. J Thromb Haemost. 2019: 17(11): 1966-72. PubMed
- Kamarova M, Baig S, Patel H, et al. Antiplatelet use in ischemic stroke. Ann Pharmacother. 2022;56(10):1159-73. PubMed
- Douketis JD, Spyropoulos AC. Perioperative Management of Anticoagulant and Antiplatelet Therapy. NEJM Evid. 2023;2(6): EVIDra2200322. PubMed
- Moster, M., Bolliger, D. Perioperative guidelines on antiplatelet and anticoagulant agents: 2022 update. Curr Anesthesiol Rep. 2022;12, 286–96. Link
- Horlocker TT, Vandermeuelen E, Kopp SL, et al. Regional anesthesia in the patient receiving antithrombotic or thrombolytic Therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Fourth Edition). Reg Anesth Pain Med. 2018;43(3):263-309. PubMed
- Douketis JD, Spyropoulos AC, Murad MH, et al. Perioperative management of antithrombotic therapy: An American College of Chest Physicians Clinical Practice Guideline. Chest. 2022;162(5):e207-e243. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.