Copy link
Anterior Mediastinal Masses in Children
Last updated: 02/05/2024
Key Points
- Mediastinal masses can arise in any of the three anatomical mediastinal compartments; however, anterior mediastinal masses (AMM) are more commonly linked to potential untoward complications related to respiratory and/or cardiovascular compromise.
- Symptoms secondary to AMM are more common in pediatric patients due to the overall smaller size and compressible nature of their airways and vascular structures.
- Maintaining spontaneous ventilation and natural airway tone when possible is ideal.
Introduction
- The management of patients with mediastinal masses poses several anesthetic challenges.1-3 Mediastinal masses are not a commonly seen pathology in pediatric patients thus leading to decreased overall experience in the intraoperative management amongst anesthesia providers.
- The incidence of perioperative complications related to AMM in pediatric patients is estimated to be about 9-20%. Complications range from transient changes in blood pressure or mild airway obstruction to complete cardiovascular collapse and death.3
- Malignancies are the most common etiology of AMM, with lymphomas being the most common diagnosis.1 Other potential causes include acute lymphoblastic leukemia, vascular malformations, teratomas, thymomas, germ cell tumors, etc.
Pathophysiology
- The severity of symptoms and signs depends on the size of the AMM and its position within the anterior mediastinum.
- Symptoms may worsen with supine positioning due to the gravitational effect of the AMM on the posterior structures and could be magnified under general anesthesia due to the relaxation of smooth muscles of the respiratory system.
- Specific effects of the mass are listed in Table 1.
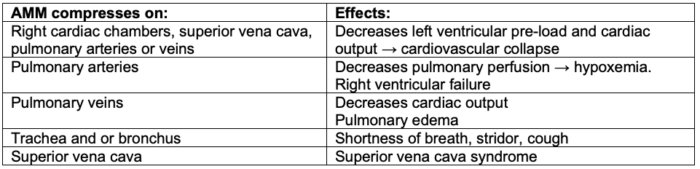
Table 1. Physiological effects of AMMs
Clinical Presentation
- The clinical presentation of AMMs depends on the size of the mass, location, and rapidity of growth. It has been estimated that about 76% of patients with an AMM are symptomatic upon presentation.1
- Common signs and symptoms of AMM include the following.
- Respiratory: cough, stridor, dyspnea, chest fullness, hoarseness, or orthopnea
- Cardiovascular: syncope, tachycardia, jugular venous distention, superior vena cava syndrome, and/or cyanosis
- Constitutional: fever, night sweats, and/or weight loss
- When compared to adults, children with AMMs are more likely to be symptomatic for several reasons.3
- AMMs in children tend to be malignant and thus grow faster.
- Children have smaller intrathoracic volumes with resultant mass effects.
- The pediatric airway and vascular structures are smaller and more compressible.
Diagnostic Workup
- The diagnostic workup of a patient with an AMM typically involves a multidisciplinary team, including oncology, anesthesiology, critical care medicine, surgery, interventional radiology, etc. Open lines of communication between all team members and considering patient-specific risks of general anesthesia to determine the safest approach is critical. Details of the workup are listed in Figure 1.
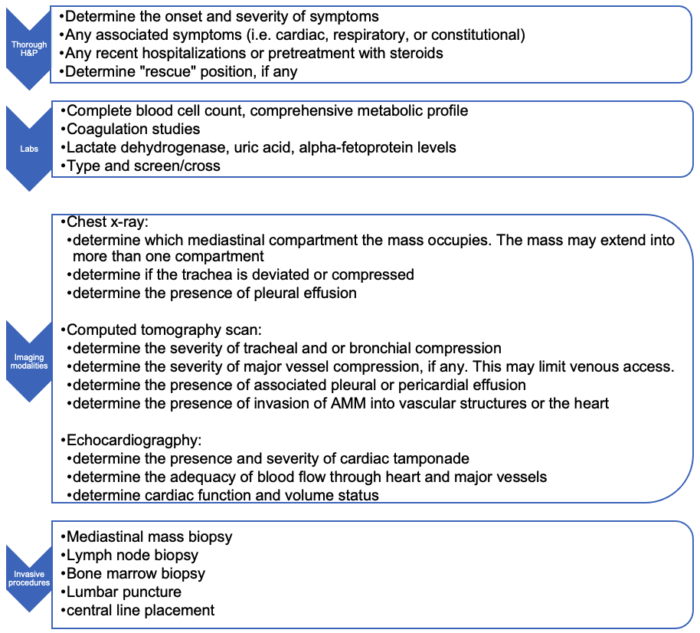
Figure 1. Diagnostic workup of a patient with an AMM
Preanesthetic Workup
- The proposed procedure(s) should be reviewed and discussed with the multidisciplinary team.
- These procedures are typically scheduled as urgent cases to enable the timely initiation of appropriate treatment. However, if the child is severely compromised at presentation, it may be safer to administer the initial treatment before obtaining a definitive diagnosis.
- The appropriate location for the procedure depends on the planned procedure and the patient’s clinical status. Ideally, the procedures should be performed in the operating room or cardiac operating room if the use of extracorporeal bypass is being considered.
- Prior anesthetic records should be reviewed, if available.
- Patients with AMMs can be risk stratified as low-, intermediate-, or high-risk, based on diagnostic imaging and clinical presentation (Table 2).
- The patient’s rescue position, if any, should be determined. For example, the lateral or prone position may alleviate the patient’s symptoms while awake.
- The need for other rescue backup procedures like ECMO standby or ECMO cannulation before other diagnostic procedures should be determined.
- The need for rigid bronchoscopy and ENT surgeons on standby should be considered, especially if general anesthesia is being considered.
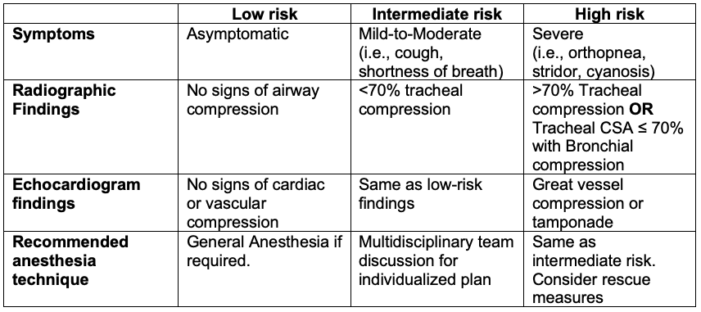
Table 2. Risk stratification of patients with AMMs and recommended anesthesia technique
Intraoperative Considerations
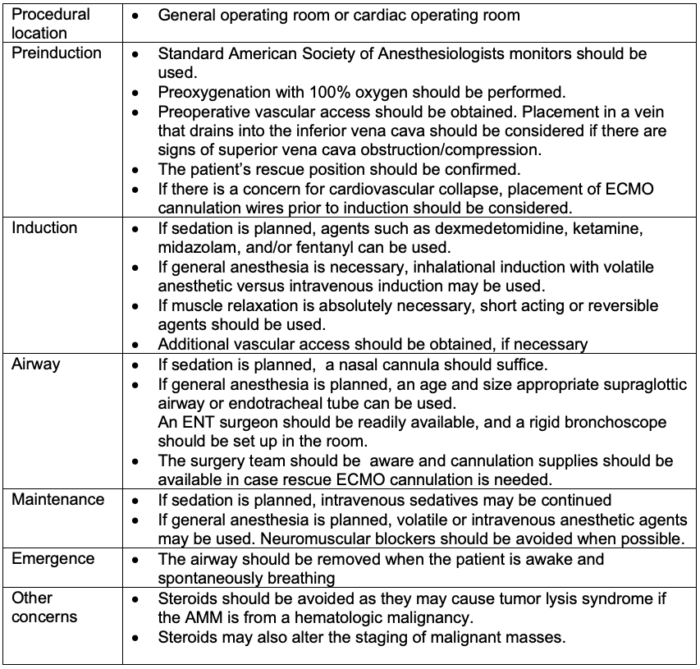
Table 3. Intraoperative anesthetic considerations of AMM
Management of Complications
- If airway or cardiovascular complications occur during general anesthesia and or sedation, the following algorithms can be used.
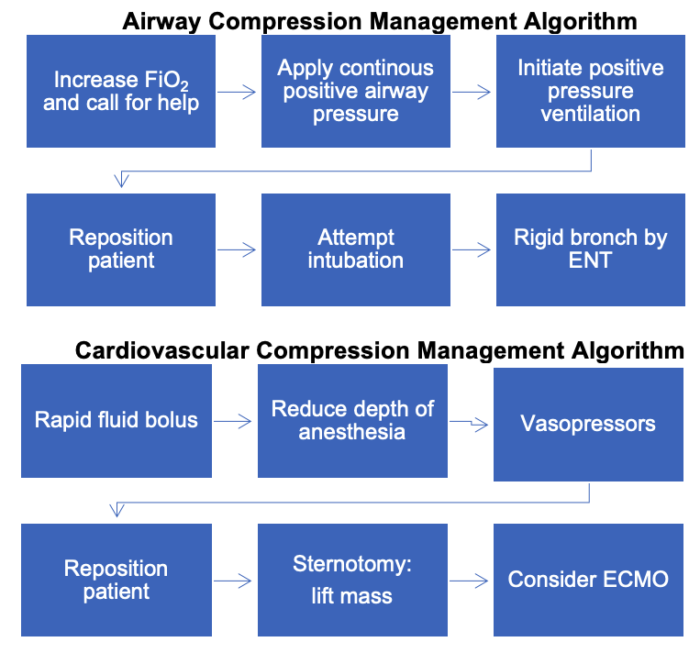
Figure 2. Algorithms for the management of airway and cardiovascular compression from AMM
Postoperative Disposition
Postoperatively, patients should be transported to the intensive care unit (ICU) in the following situations.
- The patient was originally in ICU due to the severity of symptoms and signs.
- There were intraoperative complications, e.g., excessive bleeding, pneumothorax, airway collapse, hypotension, etc.
References
- Tan A, Nolan JA. Anesthesia for children with anterior mediastinal masses. Paediatr Anaesth. 2022;32(1):4-9. PubMed
- McLeod M, Dobbie M. Anterior mediastinal masses in children. BJA Educ. 2019;19(1):21-6. PubMed
- Pearson JK, Tan GM. Pediatric anterior mediastinal mass: A review article. Semin Cardiothorac Vasc Anesth. 2015;19(3):248-54. PubMed
Other References
- Ambardekar A. Anterior mediastinal mass. OpenAnesthesia Podcast. 2019. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.