Copy link
Angiotensin-Converting Enzyme Inhibitors
Last updated: 09/09/2025
Key Points
- Angiotensin-converting enzyme (ACE) inhibitors are foundational therapies in cardiovascular and renal disease, providing benefits through manipulation of the renin-angiotensin-aldosterone system (RAAS) that leads to reduced blood pressure, decreased afterload, and slowed progression of conditions such as heart failure, myocardial infarction, and diabetic nephropathy.
- ACE inhibitors block the conversion of angiotensin I to angiotensin II, resulting in vasodilation, reduced aldosterone-mediated volume retention, and prevention of adverse cardiac remodeling. ACE inhibitors also increase bradykinin levels, which can cause side effects like cough and angioedema.
- Clinical use of ACE inhibitors requires careful dosing, starting low and titrating based on renal function, potassium levels, and blood pressure, with particular preoperative considerations due to risk of intraoperative hypotension, especially in hypovolemic or elderly patients.
Introduction
- ACE inhibitors are cornerstone medications in the management of cardiovascular and renal disease.1
- They act on RAAS, reducing blood pressure and afterload, and slowing the progression of kidney disease.1,2
- Clinical indications of ACE inhibitors include hypertension, heart failure with reduced ejection fraction (HFrEF), post-myocardial infarction (MI) remodeling and survival, and chronic kidney disease, especially in diabetics with proteinuria.1,2
- In the setting of acute MI, ACE inhibitors are started early to reduce afterload and left ventricular remodeling, improving survival and supporting neurohormonal recovery.1
- Important considerations include renal function monitoring and potassium levels due to the risk of hyperkalemia and renal impairment.1
Mechanism of Action
- In the absence of ACE inhibitors, when decreased blood flow (e.g., in hypovolemia, dehydration, heart failure, or liver failure) is detected by the kidneys, renin is released, triggering a cascade that ultimately leads to the production of angiotensin II and aldosterone. 3 This leads to vasoconstriction and aldosterone-mediated sodium retention and potassium excretion, which increases circulating volume and restores perfusion.3
- Angiotensin II constricts both afferent and efferent renal arterioles, increasing efferent resistance to maintain glomerular filtration pressure.3
- ACE inhibitors block the conversion of angiotensin I to angiotensin II by inhibiting angiotensin-converting enzyme.3
- Inhibition leads to:
- Vasodilation
- Decreased aldosterone results in decreased sodium and water retention
- Decreased sympathetic activity
- Decreased fibrosis and ventricular remodeling
- Inhibition leads to:
- Additionally, ACE inhibitors prevent the degradation of bradykinin, a vasodilator.3
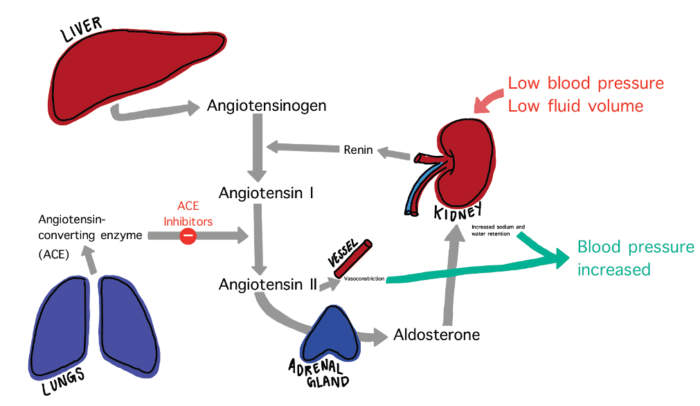
Figure 1. Overview of the Renin-Angiotensin-Aldosterone System (RAAS) and the site of action of ACE inhibitors.
Pharmacokinetics
- The metabolism and excretion of ACE inhibitors vary depending on the specific drug.4
- Prodrugs require conversion to the active form in the liver. These include enalapril, ramipril, and quinapril.5
- Active drugs, such as captopril and lisinopril, are active and do not require hepatic conversion. As such, these drugs are suitable for patients with hepatic dysfunction.4
- The primary route of elimination is via the kidneys. Dosage adjustments are required in patients with impaired renal function.4,5
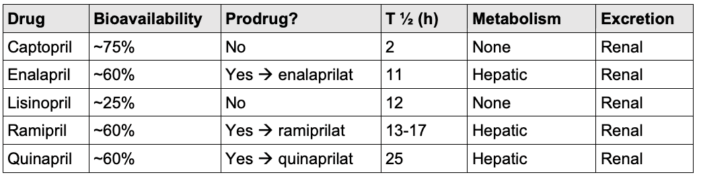
Table 1. Pharmacokinetic properties of common ACE inhibitors.4,5
Systemic Effects
- ACE inhibitors have several systemic effects.
- Cardiovascular effects include decreased preload and afterload, resulting in reduced left ventricular hypertrophy, which in turn decreases mortality in HFrEF and post-MI.6
- In heart failure, ACE inhibitors improve symptoms, reduce hospitalizations, and prolong survival in HFrEF through afterload reduction and prevention of remodeling.6
- Renal effects include decreased intraglomerular pressure, which slows the progression of chronic kidney disease (CKD).
- Respiratory effects include increased bradykinin, which can result in the production of a dry cough.
Clinical Uses
- ACE inhibitors are commonly indicated for cardiovascular and renal diseases, including heart failure, acute coronary syndrome, nephrotic syndrome, diabetes, and hypertension.7
- The most common use is treatment of hypertension due to their reduction in the production of angiotensin II, thus resulting in decreased vasoconstriction.7
- ACE inhibitors aid in improving heart function by decreasing preload and afterload. For a similar reason, ACE inhibitors are used in the regimen of medications prescribed post-MI, allowing the heart to heal more effectively and preventing remodeling.7
- ACE inhibitors are useful in diabetes and diabetic nephropathy by managing blood pressure, preventing damage to the kidneys, and reducing proteinuria. This can delay the need for dialysis or kidney transplantation. For similar reasons, ACE inhibitors are utilized in CKD.7
- Scleroderma renal crisis is characterized by the abrupt onset of severe hypertension accompanied by rapidly progressive renal failure and heart failure. 8 Activation of RAAS plays a role in the pathogenesis of scleroderma renal crisis; therefore, the current practice for management is rapid lowering of blood pressure with ACE inhibitors.8 Captopril is the drug of choice due to its rapid onset of action.8
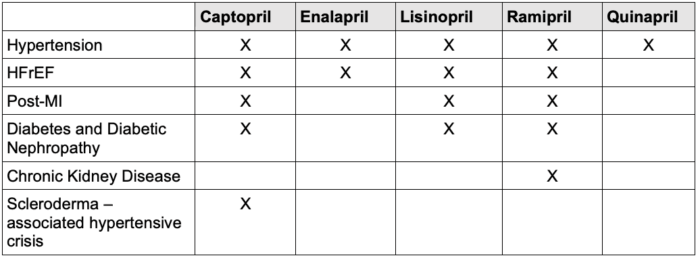
Table 2. Common indications for ACE inhibitors. Abbreviations: HFrEF, heart failure with reduced ejection fraction; MI, myocardial infarction.2,3,7,8
Preoperative Considerations
- It is recommended to hold ACE inhibitors at least 24 hours prior to elective surgery in select patients with controlled blood pressure to reduce the risk of intraoperative hypotension. If they are not withheld, patients may experience significant hypotension during anesthesia induction that is resistant to fluids and may require vasopressor support. However, randomized trials, such as the STOP-or-NOT trial, are still assessing for a difference in major cardiovascular events between continuation and omission strategies.9
- This is more common in patients who are hypovolemic, elderly, on multiple antihypertensives, or undergoing surgeries with blood loss or neuraxial blockade.8
- ACE inhibitors may exaggerate hypotension following spinal or epidural anesthesia due to loss of sympathetic tone.9
- This is more common in patients who are hypovolemic, elderly, on multiple antihypertensives, or undergoing surgeries with blood loss or neuraxial blockade.8
- There is no clear consensus on holding in urgent/emergent cases. In emergencies, ACE inhibitors are often continued, but anesthesia teams should be prepared with vasopressin and other advanced hemodynamic support. Additionally, for patients with heart failure with reduced ejection fraction, the American College of Cardiology recommends that continuation of ACE inhibitors perioperatively is reasonable, given the established benefits of these agents in this population.9
- ACE inhibitor continuation may be reasonable in patients with uncontrolled hypertension or in short, low-risk procedures with minimal fluid shifts or blood loss. This decision should be individualized.9
Dosage
- Dosing of ACE inhibitors should start low and be titrated based on blood pressure, renal function, and potassium. Dosing may require adjustment in renal impairment. 10
- If CrCl is 10-50 mL/min, reduce the initial recommended dose by 25%, then titrate to effect.10
- If CrCl < 10 mL/min, reduce the initial recommended dose by 50%, then titrate to effect.10
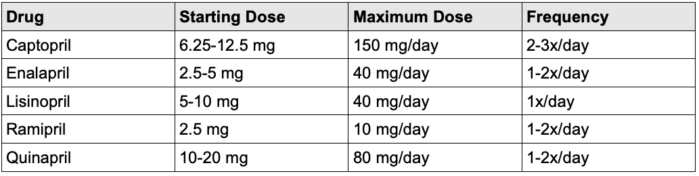
Table 3. Dosing ACE inhibitors10
Side Effects
- ACE inhibitors can result in a variety of side effects, including:
- Dry cough due to the accumulation of bradykinin. The cough can start one week after initiation and usually continues up to 6 months. However, it is a common reason for low medication adherence and discontinuation.2
- Hyperkalemia due to decreased aldosterone, resulting in decreased excretion of potassium at the collecting ducts.2
- Angioedema is a rare but life-threatening side effect. The mechanism of angioedema is thought to involve the excessive accumulation of bradykinins.2
- Hypotension is a side effect due to the vasodilatory effect of ACE inhibitors. It is another source of discontinuity in a small population of patients.2
- Fatigue and dizziness are byproducts of possible hypotension.2
- Hypovolemia-induced acute kidney injury with increased blood urea nitrogen and creatinine, which especially occurs in patients with heart failure or on diuretics.2
Contraindications
- Absolute contraindications include:
- Pregnancy because ACE inhibitors are teratogenic, resulting in fetal renal malformation and oligohydramnios.2
- Bilateral renal artery stenosis
- History of angioedema and allergic reactions to ACE inhibitors.2
- Relative contraindications include:
- Aortic stenosis or hypertrophic cardiomyopathy, as these patients may not tolerate the reduction in afterload.2
- Severe hyperkalemia or acute kidney injury, as ACE inhibitors can cause an elevation of potassium and worsen renal function. Patients with abnormal renal function should be routinely monitored if on an ACE inhibitors.2
References
- Sobhy M, Eletriby A, Ragy H, et al. ACE inhibitors and angiotensin receptor blockers for the primary and secondary prevention of cardiovascular outcomes: recommendations from the 2024 Egyptian cardiology expert consensus in collaboration with the CVREP foundation. Cardiol Ther. 2024; 13 (4): 707-736. PubMed
- Singh B, Cusick AS, Goyal A, et al. ACE Inhibitors. In: StatPearls (Internet). Treasure Island, FL. StatPearls Publishing; 2025. Accessed August 6, 2025. Link
- Cutrell S, Alhomoud I, Mehta A, et al. ACE-Inhibitors in hypertension: a historical perspective and current insights. Curr Hypertens Rep. 2023; 25 (9): 243-250. PubMed
- Kelly JG, O’Malley K. Clinical pharmacokinetics of the new ACE inhibitors. A review. Clin Pharmacokinet. 1990; 19 (3): 177-196. PubMed
- Vertes V, Haynie R. Comparative pharmacokinetics of captopril, enalapril, and quinapril. Am J Cardiol. 1992; 69 (10): 8C-16C. PubMed
- CONSENSUS Trial Sutdy Group. Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med. 1987; 316 (23): 1429-1435. PubMed
- Herman LL, Padala SA, Ahmed I, et al. Angiotensin-converting enzyme inhibitors (ACEI). In: StatPearls (Internet). Treasure Island, FL. StatPearls Publishing; 2025. Accessed August 6, 2025. Link
- Basyal B, Finnigan NA. Scleroderma and renal crisis. In: StatPearls (Internet). Treasure Island, FL. StatPearls Publishing; 2025. Accessed August 6, 2025. PubMed
- Thompson A, Fleischmann K, Smilowitz N, et al. 2024 AHA/ACC/ACS/ASNC/HRS/SCA/SCCT/SCMR/SVM: Guideline for perioperative cardiovascular management for noncardiac surgery: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2024; 150 (19): e351-e442. PubMed
- Dalpoas SE, Lipika S. ACE Inhibitors. Johns Hopkins Diabetes Guide, The Johns Hopkins University, 2017. Johns Hopkins Guides. Accessed August 6, 2025. Link
Other References
- Bechtel A, Chiao S. ACE inhibitors, MOA, Contraindications. OA Keys to the Cart. 2017. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.