Copy link
Anesthesia for Patients with Liver Disease
Last updated: 05/08/2024
Key Points
- Patients often present for anesthesia with no documented history of liver disease. Around 75% of the liver must be affected before signs and symptoms become apparent.
- Hepatic dysfunction exists on a spectrum of severity ranging from mild, asymptomatic disease to severe, end-stage liver disease with profound physiologic and metabolic implications.
- As liver disease progresses, multiple critical organ systems, including the heart, kidneys, and nervous system, are affected.1,2
Introduction
- Hepatic dysfunction is a complex and multifaceted medical condition that presents unique challenges in the field of anesthesiology. The liver performs a multitude of metabolic and synthetic functions and plays a pivotal role in drug metabolism, coagulation, and detoxification.
- Hepatic dysfunction can significantly affect the pharmacokinetics and pharmacodynamics of anesthetics and other perioperative medications.1,2
- Anesthesiologists must have a comprehensive understanding of the pathophysiology, assessment, and perioperative management of hepatic dysfunction to ensure safe and effective anesthesia care.
Pathophysiology of Hepatic Dysfunction
- Common causes of liver disease include viral hepatitis, drug and alcohol use, and obesity (see OA Summary on chronic liver disease and cirrhosis Link). Subsequent tissue damage from the inflammatory process leads to hepatocyte destruction and biliary disruption, resulting in:
- Impaired drug metabolism: The liver is a critical site for metabolism of many drugs, and hepatic dysfunction can alter the clearance and bioavailability of many anesthetic agents, potentially leading to drug toxicity or reduced drug efficacy. Common drugs that may be affected include antibiotics, narcotics, benzodiazepines, and anticoagulants.1,2
- Coagulopathy: hepatic dysfunction often results in a deficiency of clotting factors, which can lead to abnormal coagulation ranging from excessive bleeding to hypercoagulability. Coagulation abnormalities are a major concern during surgery, making careful monitoring and correction essential. The coagulopathy of liver disease results from multiple factors: Abnormal number and function of platelets, impaired production of key procoagulant and anticoagulant proteins, hypofibrinogenemia, and abnormal fibrinolysis. As with drug metabolism, the impairment of coagulation in liver disease exists on a spectrum of severity with advanced liver disease presenting with potential profound coagulopathies.2,3
- Portosystemic shunting: In cases of advanced liver disease, portosystemic shunts may spontaneously develop, allowing toxins to bypass the liver and enter the systemic circulation. This can cause hepatic encephalopathy, which poses an additional challenge in anesthesia management.4,5
Preoperative Assessment
- Anesthesiologists must conduct a thorough preoperative assessment to gauge the severity of hepatic dysfunction and identify associated comorbidities. Key considerations should include a determination of the underlying cause and an overall assessment of disease severity using scoring tools such as the Child-Pugh-Turcotte (CPT) or Model for End-Stage Liver Disease (MELD) scores. These tools require laboratory measurement of key physiologic parameters (Table 1).1,5,6
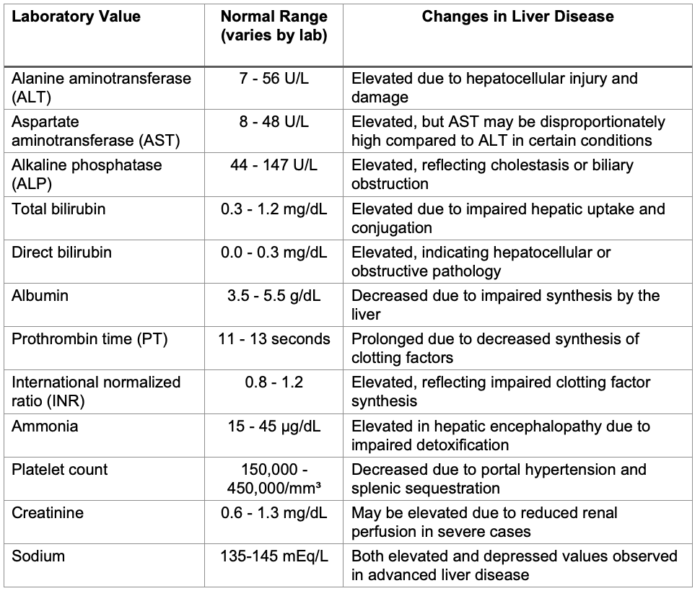
Table 1. Common laboratory tests undertaken for the assessment of liver disease
- Special attention should be paid to identifying:
- Hepatic encephalopathy: Assess for altered mental status and asterixis to determine the risk of cerebral dysfunction during and after anesthesia.5,6
- Ascites and edema: These conditions can impact respiratory and cardiovascular function during surgery. Additionally, complications of ascites, such as spontaneous bacterial peritonitis (SBP), should be identified. As the disease progresses, patients may develop umbilical and/or inguinal hernias secondary to increased intrabdominal pressure from chronic ascites.5,6
- Chronic portal hypertension: As portal hypertension worsens, spontaneous portosystemic shunts can develop that may present as dilated superficial epigastric veins that form a caput medusa. Spider angioma are often found over the trunk/abdomen of patients. Esophageal varices pose an increased risk when placing gastric tubes or transesophageal echocardiography (TEE) probes.5,6
- Jaundice: As the biliary tree becomes increasingly damaged with cirrhosis, normal elimination of bilirubin is disrupted, and patients develop hyperbilirubinemia and jaundice, often accompanied by pruritis.2,5,6
- Organ dysfunction: As liver disease progresses and portal hypertension worsens, other organ systems can be affected (Figure 1). Nearly all organ systems are affected, and with increasing disease severity comes a need for further invasive testing, including consultation of specialized medical services.5,6,7
- Coagulopathy: A common manifestation in advanced liver disease. Existing hypo- or hypercoagulopathy should be assessed and corrected where necessary ahead of surgery.2,3,6
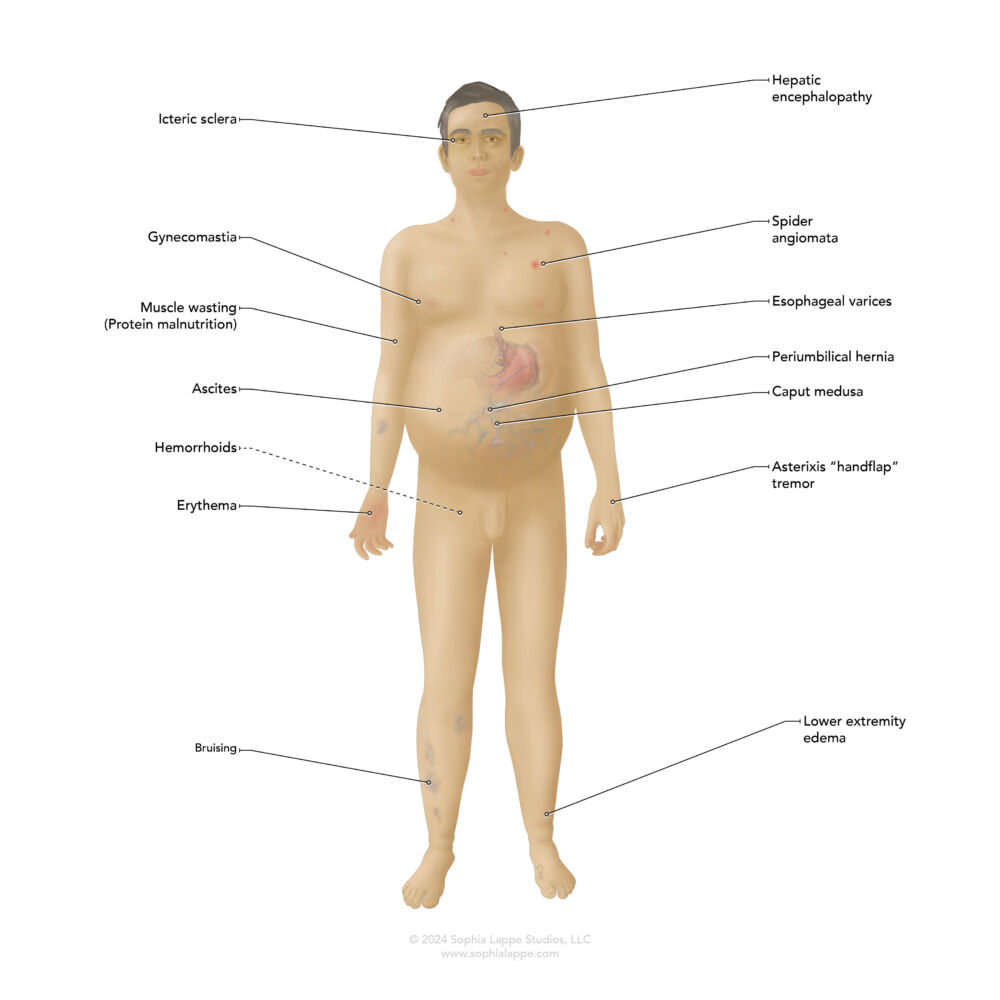
Figure 1. Common signs and symptoms presenting during the development of end-stage liver disease. Most become apparent as portal hypertension worsens.
Perioperative Management
Drug Selection
- Anesthetic drugs with minimal hepatic metabolism should be selected, and dosages adjusted based on the degree of hepatic dysfunction (Table 2). Considerations should include avoiding or minimizing drugs like benzodiazepines and opioids that undergo significant hepatic metabolism.1,5
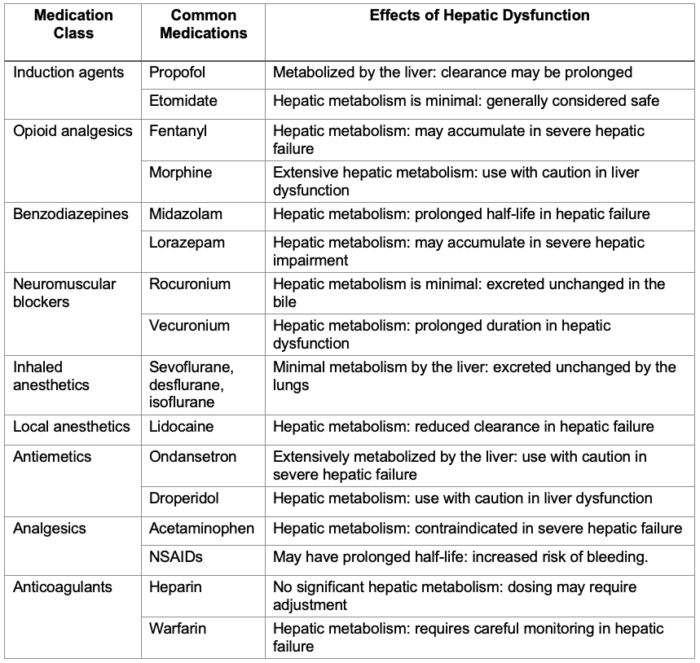
Table 2. Impact of liver disease on the pharmacokinetics of commonly used anesthetics. Abbreviation: NSAID, non-steroidal anti-inflammatory drugs.
Hemodynamic Stability
- Patients with hepatic dysfunction are at risk for circulatory instability; thus, maintaining hemodynamic stability is crucial. Invasive arterial blood pressure monitoring may be necessary to guide fluid management and vasopressor support, depending on the patient’s disease severity and the extent of the intended procedure. TEE may be a useful adjunct to assess cardiac function in patients with advanced liver disease.2
Coagulation Management
- Coagulopathies should be assessed and addressed by using blood products such as fresh frozen plasma, cryoprecipitate, and platelets. The use of desmopressin should be considered to enhance platelet function. Depending on the extent of bleeding during the procedure, the clinician may consider the use of plasma-derived and recombinant clotting factor concentrates (e.g., fibrinogen concentrate, prothrombin complex concentrate, recombinant activated clotting factor VII) to improve coagulation parameters.3
Postoperative Care
- Even for patients with liver disease at the milder end of the spectrum, the risk of decompensation following surgery requires extra care to be taken. Patients with worsening hepatic dysfunction may require specialized care in the intensive care unit for close monitoring of hemodynamics, coagulation status, and the management of hepatic encephalopathy.2
References
- Simmons F, Pustavoitau A, Merritt WT. Diseases of the Liver and Biliary Tract. In: Hines RL, Jones SB. eds. Stoelting’s Anesthesia and Co-existing Disease. 8th ed. Elsevier, Philadelphia, PA; 2022: 333-46.
- Ramsay M. Anesthesia for Patients with Liver Disease. In: Butterworth JF, Mackey DC, Wasnick JD. eds Morgan & Mikhail's Clinical Anesthesiology. 7e. McGraw-Hill Education, Accessed April 27, 2024. Link
- Kujovich JL. Coagulopathy in liver disease: a balancing act. Hematology Am Soc Hematol Educ Program. 2015:2015: 243-9. PubMed
- Nardelli S, Riggio O, Gioia S, et al. Spontaneous portosystemic shunts in liver cirrhosis: Clinical and therapeutical aspects. World J Gastroenterol. 2020;26(15):1726-32. PubMed
- Maher SZ, Schreibman IR. The clinical spectrum and manifestations of acute liver failure. Clin Liver Dis. 2018;22(2):361-74. PubMed
- Friedman LS. Surgery in the patient with liver disease. Trans Am Clin Climatol Assoc. 2010; 121:192-204. PubMed
- European Association for the Study of the Liver. EASL clinical practice guidelines: Liver transplantation. J Hepatol. 2016;64(2):433-85. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.