Copy link
Anesthesia for Patients with Hypertension
Last updated: 10/22/2025
Key Points
- Home blood pressure (BP) readings are the most accurate measure of baseline BP, while readings in the preoperative area are commonly higher than baseline.
- Beta-blockers, alpha blockers, calcium channel blockers, potassium-sparing diuretics, and centrally acting vasodilators are continued up to and including the day of surgery.
- Holding or continuing renin-angiotensin-aldosterone system inhibitors (RAASi) does not appear to affect postoperative outcomes.
- Holding RAASi reduces the incidence of intraoperative hypotension and vasopressor use but results in increased postoperative hypertension.
- A reasonable approach is to continue RAASis in patients having low-risk surgery or patients having moderate-risk surgery with poorly controlled hypertension and interrupt RAASis in patients having high-risk surgery or having moderate-risk surgery with well-controlled hypertension.
- It is important to support normotension intraoperatively. Maintaining a BP above an absolute threshold or within a range relative to baseline BP is an equally effective strategy to reduce postoperative complications.
- Intraoperative hypertension should be treated by first addressing the likely cause of the elevated BP and then with short-acting intravenous (IV) medications.
- Postoperative hypertension is common and can be addressed first by treating the likely cause, administering short-acting IV medications, and/or restarting home medications.
Introduction
- Globally, chronic hypertension is the leading modifiable risk factor for heart disease and stroke.
- Hypertension is defined as an average BP of more than 130 mmHg systolic (sBP) and/or more than 80 mmHg diastolic (dBP)1 (Table 1).
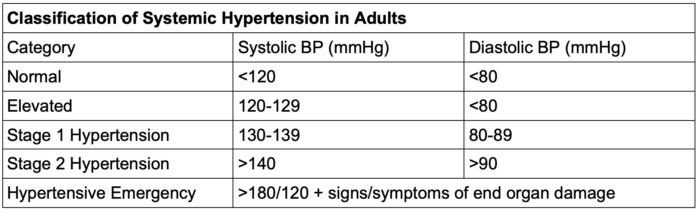
Table 1. Classification of hypertension in adults
- Patients with an average BP greater than 140/90 or greater than 130/80 with another comorbidity (diabetes mellitus, cerebrovascular disease, coronary artery disease, or chronic kidney disease) should be on prescribed antihypertensive therapy.
Outpatient Management
- Chronic hypertension should be addressed in the outpatient setting so that an appropriate treatment regimen can be initiated with a goal of a BP less than 130/80.1
- Undiagnosed or untreated obstructive sleep apnea, noncompliance with medical therapy, subtherapeutic antihypertensive regimens, pain, anxiety, tobacco use, and/or illicit drug use can be addressed during an outpatient preoperative visit to optimize hypertensive patients prior to surgery.2
- In patients with persistent hypertension despite compliance with three or more medications, secondary causes of hypertension should be considered (primary aldosteronism, renal artery stenosis, pheochromocytoma).1
- Antihypertensive medications may be started or escalated in the outpatient setting if there is adequate time before surgery to do so (weeks to months).2
Medication Management
- Alpha, beta-, and calcium channel blocker therapy should be continued preoperatively.
- Interruption of beta- or calcium channel blocker therapy increases perioperative risk of major adverse cardiac events. For this reason, missed doses should be administered in the preoperative period.
- Interruption of clonidine therapy can result in severe rebound hypertension. It should be continued and can be administered orally or transdermally.
- Loop diuretics are commonly held to avoid hypovolemia, but may be continued in patients with severe heart failure.
- Thiazide and potassium-sparing diuretics can be continued
- RAASi have historically been held prior to surgery, but this management strategy is currently under scrutiny and an area of active research.
- There is an increased incidence of intraoperative hypotension in patients who continue RAASi. Conversely, patients who hold RAASi have significantly higher rates of postoperative hypertension.2
- Neither strategy (interrupting or continuing RAASi) is associated with better outcomes; therefore, at this time, either approach is acceptable.
- Stop-or-Not trial: continuing versus stopping RAAS inhibitors before major noncardiac surgery:3
- Randomized clinical trial of 2,222 patients being treated with a RAASi for at least 3 months scheduled to undergo a major noncardiac surgery between January 2018 and April 2023 at 40 hospitals in France
- Patients were randomized to continue use of RAASIs (n = 1107) until the day of surgery or to discontinue use of RAASIs 48 hours prior to surgery (n = 1115).
- No difference in mortality or postoperative complications between groups
Preoperative Management
- Hypertension on the day of surgery is a common occurrence. Preoperative BP readings are often much higher than home values due to anxiety, pain, or medication interruption. Repeating the measurement when a patient is more relaxed, allowed to empty their bladder, or after treating pain or anxiety often results in improvement in these numbers.
- As mentioned, missed doses of beta-blockers, calcium channel blockers, and/or clonidine should be administered in the preoperative area.
- A patient with an elevated BP (>180/120) experiencing any of the following symptoms meets the diagnostic criteria for hypertensive emergency: headache, blurred vision, chest pain, focal neurologic signs, or dyspnea.
- Patients meeting criteria for hypertensive emergency should be treated prior to emergency surgery and should not proceed to the operating room if not emergently necessary.
- Current guidelines suggest that there is no benefit to delaying elective surgery in an asymptomatic hypertensive patient if dBP is <110mmHg and sBP is <180mmHg.
- Initiating new therapy in the immediate preoperative period to rapidly achieve normotensive BP values in an asymptomatic patient is not recommended.
Intraoperative BP Management
- The most commonly accepted strategies for maintaining BP intraoperatively are:
- Absolute: maintaining a BP above a specific mean arterial pressure (MAP)
- Relative: maintaining a BP within a range of baseline
- For absolute BP management, sBP greater than 90mmHg and a MAP greater than 65mmHg were associated with reduced risk of overall mortality, acute kidney injury, myocardial injury, and stroke in multiple studies.
- For chronically hypertensive patients with high baseline BPs (MAP >100mmHg), MAP targets should be higher to avoid myocardial injury and kidney injury.
- For a relative BP control strategy, home BP readings are considered the most accurate measure of baseline when available. BPs obtained in the preoperative area are commonly higher than home values.
- Most evidence supports a goal of BP within 20% of baseline.
- One study showed that attempting to maintain sBP within 10% of baseline led to fewer complications (composite of systemic inflammatory response syndrome with renal, respiratory, cardiovascular, or neurologic dysfunction).
- Profound hypotension after induction of anesthesia in a chronically hypertensive patient occurs frequently. Relative to normotensive patients, patients with systemic hypertension have a reduced intravascular volume due to chronic vasoconstriction. The vasodilatory effects of induction medications in the setting of relative hypovolemia leads to an abrupt drop in preload. Gentle hydration with ~250mL of crystalloid just prior to induction can help blunt this response.
- Euvolemia should be maintained and vasoactive medications should be administered as needed to achieve target BPs.
Intraoperative Hypertension
- Clinicians should consider and treat reversible causes of hypertension.
- If acute hypertension is severe or persists for longer than several minutes, use IV antihypertensive medications.
- Start with short-acting agents to avoid overtreatment and persistent hypotension (for example, esmolol, hydralazine, or nicardipine)
- Longer-acting agents such as labetalol or metoprolol can be given, especially in the setting of concomitant tachycardia.
- Infusions may be necessary to achieve BP control in patients with persistent hypertension.
- Typical causes of intraoperative hypertension include:
- Laryngoscopy and endotracheal intubation
- Surgical stimulation
- Hypoxemia and hypercarbia (can cause hypertension and tachycardia due to sympathetic stimulation)
- Hypervolemia
- Antihypertensive medication withdrawal
- Emergence and tracheal extubation
- Bladder distention
- Elevated intracranial pressure
- Alcohol or benzodiazepine withdrawal
- Recent cocaine or methamphetamine use
Postoperative Hypertension
- Hypertension in the postanesthesia care unit is typically treated if sBP is greater than 180mmHg or dBP is greater than 110mmHg in similar ways as stated above.
- Common causes of postoperative hypertension include:
- Pain
- Nausea/vomiting
- Hypoxemia
- Hypercarbia
- Delirium/agitation
- Hypothermia with shivering
- Bladder distension
- Hypervolemia
- Withdrawal from alcohol or opioids
- Recent cocaine/methamphetamine/phencyclidine use
- Treat reversible causes as appropriate: analgesics, antiemetics, benzodiazepines, noninvasive ventilatory support, and/or catheterization for bladder emptying
- Clinicians should reinstate preoperative oral antihypertensive therapy as soon as possible or use an IV alternative if the patient remains nil per os in the acute postoperative setting.
- Postoperative BPs within 20% of baseline are typically acceptable for discharge from the postanesthesia care unit.
References
- Writing Committee Members*; Jones DW, Ferdinand KC, Taler SJ, et al 2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Hypertension. 2025;82(10):e212-e316. PubMed
- Schonberger R, Fontes M, Selzer A, Anesthesia for Patients with Hypertension. In: UpToDate; 2025. Accessed Oct 13, 2025. Link
- Legrand M, Falcone J, Cholley B, et al Stop-or-Not Trial Group. Continuation vs discontinuation of renin-angiotensin system inhibitors before major noncardiac surgery: The Stop-or-Not Randomized Clinical Trial. JAMA. 2024 ;332(12):970-978. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.