Copy link
Anesthesia for Patients with Altered Kidney Function
Last updated: 06/27/2025
Key Points
- Chronic kidney disease (CKD) impairs fluid, electrolyte, and acid-base balance, and leads to anemia, coagulopathy, and cardiovascular complications. These systemic effects have a significant impact on perioperative risk and anesthetic planning.
- Renal dysfunction alters drug metabolism and clearance, necessitating avoidance of agents like morphine and meperidine, while favoring drugs such as remifentanil and cisatracurium that are not renally dependent. Neuromuscular blockers and their reversal agents require careful selection and monitoring.
- Regional techniques are preferred when appropriate to minimize systemic drug exposure. General anesthesia requires adjusted dosing and vigilant monitoring, while postoperative pain is best managed with a multimodal regimen that avoids nephrotoxic agents.
Introduction
- In 2024, the Kidney Disease Improving Global Outcomes group updated the clinical practice guidelines for the evaluation and management of CKD.1
- CKD is defined as abnormalities of kidney structure or function, present for a minimum of three months, with implications for health (Table 1).1
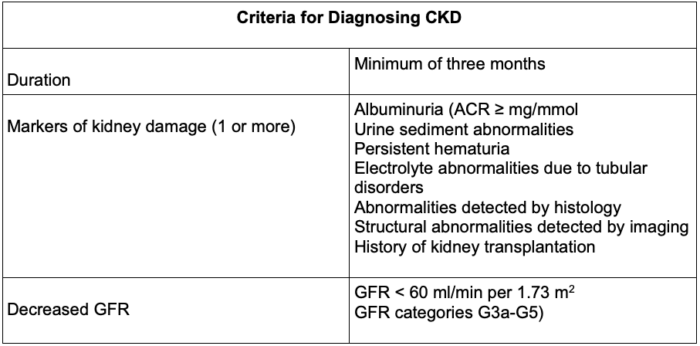
Table 1. Diagnosis of CKD. Abbreviations: CKD, chronic kidney disease; ACR, albumin-to-creatine ratio; GFR, glomerular filtration rate
- CKD is classified based on cause, glomerular filtration rate (GFR), and albuminuria (Tables 2 and 3).
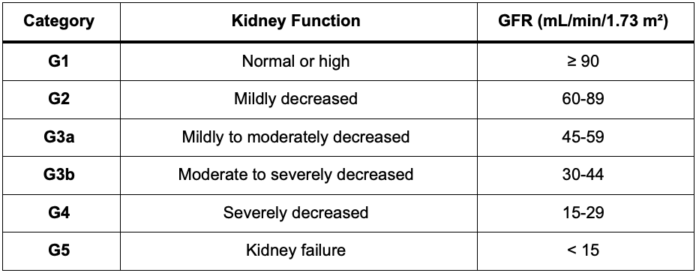
Table 2. GFR categories of CKD1 Abbreviations: CKD, chronic kidney disease; GFR, glomerular filtration rate
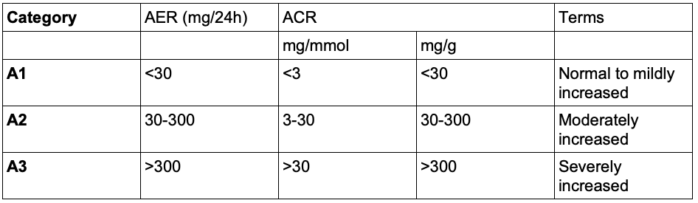
Table 3. Albuminuria categories of CKD1 Abbreviations: AER, albumin excretion rate; ACR, albumin-to-creatine ratio
- The most frequent causes of CKD include hypertensive nephrosclerosis, diabetic nephropathy, chronic glomerulonephritis, and polycystic kidney disease.2,3
- Clinical manifestations typically become apparent once the GFR declines below 25 mL/min. When the GFR falls below 10 mL/min, survival becomes dependent on renal replacement therapy, such as hemodialysis, hemofiltration, or peritoneal dialysis.3
- Creatinine clearance remains the most accurate assessment of kidney function.3
- It is essential to recognize that renal function declines with age, with renal reserve at 80 years reduced to less than half that at 40 years. Serum creatinine may not accurately reflect true renal function in older adults, as GFR can decline by up to 50% without a corresponding increase in creatinine. Therefore, renal function should be estimated using formulas such as the Cockcroft-Gault, Modification of Diet in Renal Disease, or the current CKD-exocrine pancreatic insufficiency (EPI), especially in the elderly, patients with elevated creatinine levels or CKD risk factors.1
- In clinical practice, calculation of the creatinine-based estimated GFR using the CKD-EPI equation is recommended in adults at risk for CKD.1
- Please see the OA summary on assessment of renal function for more details. Link
Pathophysiology of Chronic Renal Failure
Metabolic Manifestations
- Hypervolemia:
- In CKD, total body sodium and water content are typically elevated. Still, clinical signs of hypervolemia may be delayed until GFR is markedly reduced, with weight gain from volume expansion often obscured by concurrent lean body mass loss.4
- Resulting extracellular fluid overload and hyponatremia are commonly managed with loop diuretics in combination with metolazone, which inhibits sodium-chloride reabsorption in the distal convoluted tubule and helps overcome diuretic resistance.4
- Electrolyte Disturbances:
- Common metabolic abnormalities include hyperkalemia, hyperphosphatemia, hypocalcemia, hypermagnesemia, hyperuricemia, and hypoalbuminemia.3
- Hyperkalemia, though uncommon at higher GFRs, is potentially life-threatening and may be precipitated by trauma, hemolysis, infection, or potassium administration.3,7 While gastrointestinal excretion offers partial compensation, impaired renal clearance and altered cellular handling contribute significantly to potassium accumulation.4
- Hypermagnesemia is typically mild unless intake is excessive, often due to magnesium-containing antacids.4
- Hypocalcemia arises from parathyroid hormone resistance, reduced synthesis of 1,25-dihydroxycholecalciferol, and calcium-phosphate deposition in bone; symptoms are uncommon unless accompanied by alkalosis.3
- Acid-Base Disturbances:
- Although urinary acidification is generally maintained, ammonia production is impaired, limiting acid excretion. Early acidosis is typically nonanion gap, progressing to an increased anion gap and reduced bicarbonate levels in advanced disease. Acidemia is often tolerated but may worsen postoperatively, requiring dialysis.4
Hematologic Manifestations
- Anemia:
- Anemia typically develops when the GFR falls below 30 mL/min and is characterized by normochromic, normocytic red blood cells, with hemoglobin levels often between 6 and 8 g/dL, primarily due to reduced erythropoietin production, decreased red blood cell survival, and impaired erythropoiesis.1,4
- Contributing factors include iron deficiency, gastrointestinal bleeding, frequent phlebotomy, hemodilution, and bone marrow suppression from recurrent infections, with transfusion often insufficient to maintain hemoglobin levels above 9 g/dL.1,4
- Hemostasis
- In kidney failure, platelet dysfunction, including reduced factor III activity, impaired adhesiveness, and aggregation, leads to prolonged bleeding times, while leukocyte dysfunction increases susceptibility to infection.
- Coagulation defects may persist despite dialysis but can be managed with treatments such as desmopressin, cryoprecipitate, conjugated estrogens, blood transfusions, and erythropoietin.3,4
Cardiovascular and Pulmonary Manifestations
- In kidney failure, cardiac output increases to compensate for the decreased oxygen-carrying capacity, while sodium retention and disruptions to the renin-angiotensin system leads to hypertension and left ventricular hypertrophy.3,4
- This, along with fluid overload, anemia, and metabolic disturbances, contributes to congestive heart failure, pulmonary edema, arrhythmias, uremic pericarditis, and accelerated atherosclerosis, all of which can be managed with diuretics or dialysis, though hypertension often persists due to renin-angiotensin system activation.3,4
Gastrointestinal Manifestations
- Uremia can commonly cause anorexia, nausea, vomiting, and, while increased gastric acid secretion and delayed gastric emptying due to autonomic neuropathy raise the risk of peptic ulceration, gastrointestinal bleeding, and perioperative aspiration.3
- Patients with CKD also have a higher prevalence of hepatitis B and C, with potential hepatic dysfunction.3
- The multisystem manifestations of CKD are summarized in Table 4.
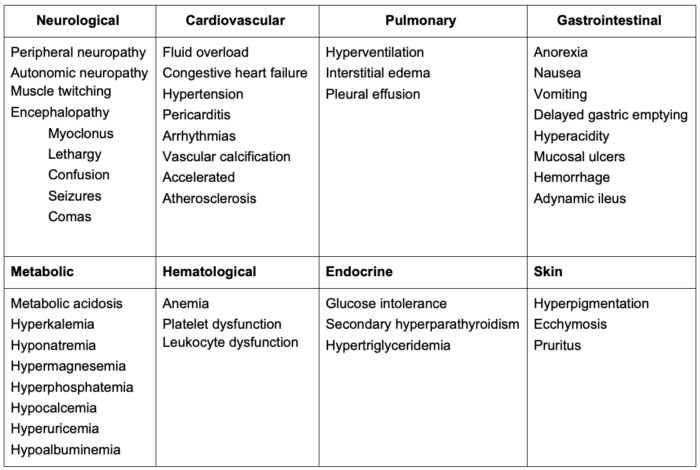
Table 4. Multisystem manifestation of chronic kidney disease (CKD)
Anesthetic Drug Considerations
- Most anesthetic agents are weak electrolytes that, in their un-ionized and lipid-soluble form, are reabsorbed by renal tubules and inactivated through redistribution and hepatic metabolism rather than renal clearance. In contrast, agents that are highly ionized or poorly lipid-soluble — such as certain muscle relaxants, diuretics, and antibiotics — may demonstrate prolonged activity in the setting of renal dysfunction due to reduced urinary excretion.4
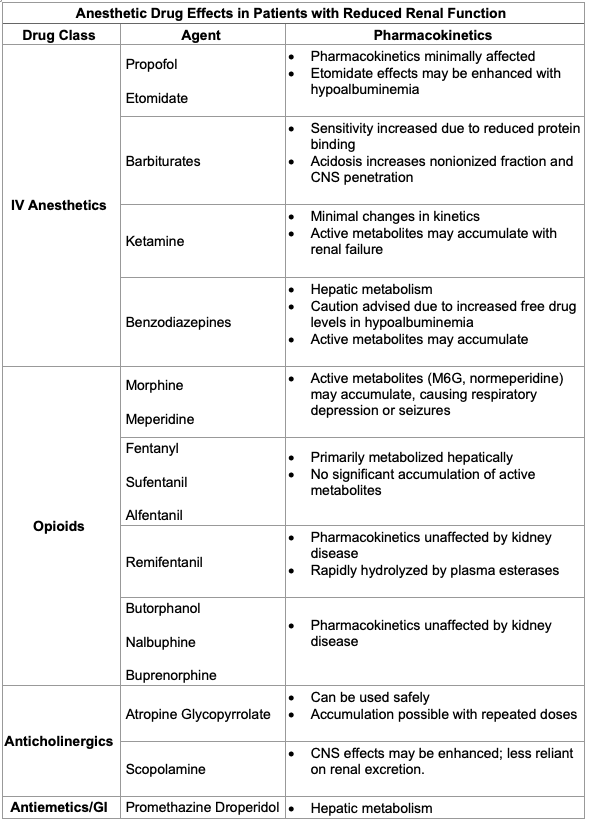
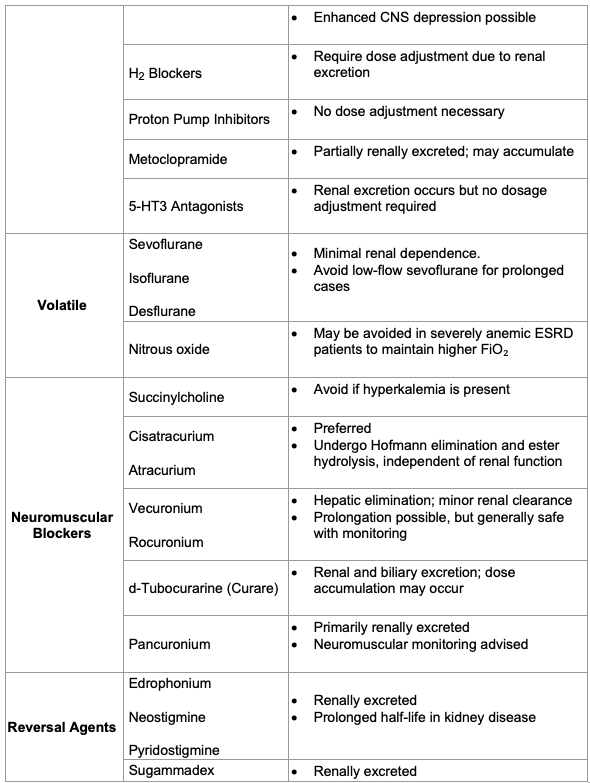
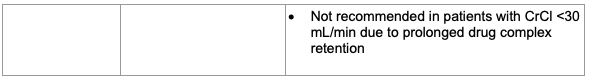
Table 5. Effects of altered renal function on anesthetic drugs3 Abbreviations: CNS, central nervous system; IV, intravenous; ESRD, end-stage renal disease
Preanesthetic Management
General Considerations
- For dialysis patients, peripheral venous access should prioritize hand veins or the dominant arm if more proximal access is required, while preserving the nondominant arm (which is usually used for arteriovenous access) and avoiding peripherally inserted central catheters (so that superficial veins can be used for future arteriovenous fistula [AVF]) unless absolutely necessary.5
- The subclavian vein should be avoided for central venous catheter placement to prevent possible stenosis that could prevent future AVF and the same side as existing dialysis access, with ultrasound guidance preferred to minimize complications and preserve future vascular access sites.5
- In patients with end-stage renal disease (ESRD), it is crucial to avoid using the current AVF or graft sites for venipuncture or vascular access, except in emergencies. The extremity with the currently functioning fistula or graft should be avoided for arterial line monitoring.5
Elective Surgery Considerations
- Patients with ESRD are at an increased risk of perioperative morbidity and mortality, regardless of the type of surgery.6 A multidisciplinary team approach is recommended.
- Patients with ESRD undergoing surgery should be evaluated for comorbidities such as cardiovascular disease, diabetes (Hgb A1c target range 6-8%), hypertension (predialysis goal of less than140/90 mmHg and postdialysis goal of 130/80mmHg), anemia (Hgb maintained at 9.0-10.0 g/dL using erythropoiesis stimulating agent), bleeding tendencies (heparin is first-choice anticoagulant for hemodialysis), and malnutrition, as these may influence anesthetic and surgical management.5,6
- Patients with less than 4 metabolic equivalents of task or unknown functional capacity should referred for a cardiology consultation.6
- Dialysis access type and site should be documented, and preoperative routine dialysis needs assessed.5
- An elective surgery should be scheduled at least 6 hours after dialysis with heparin.
- Chronic medications are generally managed similarly to non-ESRD patients. However, aspiration risk due to gastroparesis warrants prophylaxis, and preoperative use of anxiolytic midazolam and opioids should be minimized and titrated carefully, given altered protein binding and reduced clearance in ESRD.5
Emergent Surgery Considerations
- In emergency surgical settings involving patients with ESRD, collaboration with nephrology is advised when urgent dialysis may help manage severe hyperkalemia, metabolic acidosis, or volume overload.5
- In CKD, potassium homeostasis is generally maintained through tubular secretion until the GFR drops below approximately 8 mL/min. Hyperkalemia may result from decreased renal excretion, intracellular potassium shifts, or excessive intake, with contributing factors including potassium-sparing medications, aldosterone inhibition, metabolic acidosis, insulin deficiency, and exogenous potassium sources such as transfusions.6
- Hyperkalemia is particularly concerning perioperatively, as electrocardiogram findings are unreliable indicators of severity, and succinylcholine is avoided if serum potassium is ≥5.5 mEq/L. When dialysis, the most effective means of potassium excretion, is not immediately feasible, hyperkalemia is managed with intravenous calcium, insulin with glucose, and bicarbonate in cases of severe acidosis.5,7
- Please see the OA summary on hyperkalemia for more details. Link
- Volume overload requires individualized assessment; preoperative dialysis may be considered if time permits, while loop diuretics may assist in patients with residual renal function.5
- Uremic bleeding is addressed with desmopressin and platelet transfusion, though their efficacy is limited. Intraoperative coagulation and platelet function are monitored using standard and point-of-care tests to guide management.5
Intraoperative and Postoperative Anesthetic Management
Local and Regional Anesthesia for CKD/ESRD Patients
- Local anesthesia with monitored anesthesia care and regional techniques, such as peripheral nerve or neuraxial blocks, should be used whenever possible to minimize the need for general anesthesia and multiple medications.3,4
- Advantages include reduced risks associated with poor drug metabolism and superior postoperative pain relief, particularly for dialysis access surgeries.5 The patient’s coagulation status should be assessed before undergoing neuraxial or regional anesthesia blocks due to the risk of bleeding.6
General Anesthesia
- Induction
- Induction typically involves a reduced dose of propofol, avoiding higher doses due to risks of hypotension.
- Succinylcholine is preferred for rapid sequence intubation in patients with normal potassium levels (less than 5.5 mEq/L). The normal hyperkalemic response (increase by approximately 0.5 to 1 mEq/L) is not exaggerated in patients with ESRD.
- Rocuronium is often used for those with elevated potassium levels, though prolonged effects are possible due to reduced renal clearance.3,5
- For patients who do not require rapid sequence induction, nondepolarizing neuromuscular blockers, such as cisatracurium or atracurium, are preferred because they are not affected by kidney function.5
- Maintenance of Anesthesia
- Maintenance of anesthesia can involve either inhalational agents such as sevoflurane or isoflurane or total intravenous anesthesia using propofol and remifentanil, with opioids carefully titrated to prevent respiratory depression.3,5
- Intraoperative fluid management can be challenging, as hypervolemia can lead to pulmonary edema, and hypovolemia can cause hemodynamic instability. Stroke volume variation is a useful indicator of hypovolemia. Balanced salt solutions, such as normal saline or PlasmaLyte, are preferred. Lactated Ringer’s solution should be avoided in ESRD patients with hyperkalemia.
- Glucose-containing fluids should be avoided. The patient’s glucose levels should be monitored perioperatively. Moderate glucose control (less than 180 mg/dL) is recommended.6
- Red blood cell transfusion should be considered for patients with a hemoglobin less than 7 g/dL.6
- Intraoperative hemodialysis is usually not necessary except under specific situations in cardiac surgery.6
- Emergence and Recovery
- Either neostigmine or sugammadex can be used to reverse neuromuscular blockade, though sugammadex’s effects are prolonged in ESRD and can be removed by dialysis.3,5
- Quantitative monitoring of neuromuscular blockade is recommended.3,5
- Postoperative Analgesia
- Postoperative pain management typically involves a multimodal strategy incorporating nonpharmacologic options (such as neuraxial techniques, peripheral nerve blocks, or local anesthetic wound infiltration), along with nonopioid agents like acetaminophen and ketamine, and short-acting opioids (for example, fentanyl patient-controlled analgesia).5
- Agents such as gabapentinoids, meperidine, long-acting opioids, and nonsteroidal anti-inflammatory drugs are avoided due to safety concerns.3,5
- Postoperative Dialysis
- Assessment of fluid balance, electrolyte levels, urea, and creatinine is used to guide decisions on dialysis modality, dosing, and the urgency of postoperative dialysis initiation.
- Routine hemodialysis should be maintained three times weekly, and heparin administration is typically resumed 12 hours postoperatively once hemostasis is stabilized to minimize bleeding risk.6
References
- KDIGO 2024 clinical practice guidelines for the evaluation and management of chronic kidney disease. Kidney Int. 2024;105(4S):s117-314. PubMed
- Gropper MA, Miller RD, Eriksson LI, Chapter 31: Preoperative Evaluation. In: Miller’s Anesthesia. Elsevier; 2019.
- Butterworth JF, Mackey DC, Wasnick JD. Chapter 31: Anesthesia for Patients with Kidney Disease. In: Morgan and Mikhail’s Clinical Anesthesiology,7e. McGraw Hill Medical; 2025.
- Gropper MA, Miller RD, Eriksson LI, Chapter 59: Anesthesia and the Renal and Genitourinary Systems. In: Miller’s Anesthesia. Elsevier; 2019.
- Campbell JP, Cousins JM. Anesthesia for dialysis patients. In: Post T, ed. UpToDate. April 16, 2025. Link
- Kanda H, Hirasaki Y, Iida T, et al. Perioperative management of patients with end-stage renal disease. J Cardiothorac Vasc Anesth. 2017; 31(6): 2251-67. PubMed
- Chatterjee D, Shah A. Hyperkalemia. OpenAnesthesia. Created: April 3, 2023. Accessed: June 27, 2025. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.