Copy link
Adrenal Insufficiency and Perioperative Corticosteroids
Last updated: 05/24/2024
Key Points
- The hypothalamic-pituitary-adrenal axis is essential for response to physiologic stress.
- Adrenal insufficiency occurs when the adrenal glands produce insufficient levels of glucocorticoids.
- An adrenal crisis is a medical emergency that should be recognized and addressed immediately.
- Patients undergoing surgery or other stressors may benefit from glucocorticoid supplementation.
Introduction
- The hypothalamic-pituitary-adrenal axis (HPA) is one of the body’s four main neuroendocrine systems through which the hypothalamus and pituitary gland exert regulatory control over other organ systems.
- The HPA axis works through a complex system of hormone release and negative feedback loops (Figure 1).

Figure 1. Hypothalamic-pituitary-adrenal axis. Negative feedback is in red.
- The adrenal glands are located superior to each kidney. They produce mineralocorticoids, glucocorticoids, and androgens.
- The term adrenal insufficiency (AI) is used to describe a decrease or absence of the production of glucocorticoids. Mineralocorticoids may or may not also be affected.
- Glucocorticoids are released during physiologic stress and help mediate the body’s response to stress.
- Chronic adrenal insufficiency can present with a variety of symptoms, including weakness, tiredness, fatigue, anorexia, gastrointestinal symptoms, salt craving, postural dizziness, and musculoskeletal pain.1
- While chronic AI is an important consideration for any anesthesia provider in the perioperative setting, of particular concern is adrenal crisis, which is an acute insufficient level of glucocorticoids that must be recognized and treated without delay.
Types of Adrenal Insufficiency1,2
- Chronic adrenal insufficiency is divided into three subcategories based on etiology: primary, secondary, or tertiary adrenal insufficiency.
- Adrenal crisis is an acute life-threatening condition that can arise in patients with chronic adrenal insufficiency or patients with no prior diagnosis of adrenal insufficiency.
Primary Adrenal Insufficiency2
- Primary adrenal insufficiency (PAI), also known as Addison’s disease, occurs when the adrenal cortex does not produce sufficient levels of glucocorticoids despite appropriate levels of adrenocorticotropic hormone (ACTH).
- In the developed world, the most common etiology of PAI is autoimmune destruction of the adrenal cortex and is most common in 30- to 50-year-old women.
- Congenital adrenal hyperplasia (CAH) is a congenital form of PAI due to a deficiency of 21-hydroxylase (an enzyme necessary to produce cortisol).
- In tuberculosis-endemic countries, extrapulmonary tuberculosis is a significant cause of damage to the adrenal cortex, causing PAI.
- Drug-induced PAH can occur due to the inhibition of mitochondrial enzymes. Etomidate, a drug used to induce unconsciousness in the operating room, intensive care unit, or emergency room, can transiently cause this inhibition.2 Other medications with similar inhibitory effects are ketoconazole, fluconazole, itraconazole, and metyrapone.
Secondary Adrenal Insufficiency2
- Secondary adrenal insufficiency (SAI) is caused by a lack of stimulation of the adrenal cortex due to insufficient levels of ACTH. This can be due to damage to the pituitary or the lack of corticotropin-releasing hormone (CRH) from the hypothalamus (Figure 1).
- The most common cause of insufficient ACTH release is pituitary tumors, with prolactinomas being the most common. Treatment of pituitary tumors with radiation or surgery can be an iatrogenic cause.
- Other causes of SAI include traumatic brain injury and cancer treatment with immune checkpoint inhibitors. An idiopathic etiology can be considered once all other etiologies are excluded.
Tertiary Adrenal Insufficiency2
- Tertiary adrenal insufficiency (TAI) is caused by the suppression of the HPA axis by excess exogenous glucocorticoid exposure.
- Excess exogenous glucocorticoids can suppress CRH and ACTH release through negative feedback (Figure 1).
- Steroids from any route of administration (intravenous, oral, inhaled, topical) can cause HPA axis suppression.1
Adrenal Crisis
- An adrenal crisis is a medical emergency caused by acute adrenal insufficiency. If an adrenal crisis is suspected, immediate treatment with exogenous glucocorticoids should not be delayed while waiting for confirmatory diagnostic tests.3
- Adrenal crisis should be considered in patients who have continued hemodynamic instability even after administration of fluids and vasopressor support.4
- Other signs can include anorexia, nausea, vomiting, abdominal pain, weakness, fatigue, lethargy, fever, confusion, or coma.1
- For patients with previously diagnosed AI, adrenal crisis can be precipitated by the stress of illness or surgery with inadequate adjustments to exogenous steroid therapy. Other common precipitants for patients with chronic AI are fever, gastrointestinal illness, abrupt withdrawal of steroid therapy, and emotional stress.5
- In patients without known chronic AI, pituitary infarction (pituitary apoplexy) and infarction or hemorrhage of the adrenal glands (Waterhouse-Friderichsen syndrome) should be considered.2
Diagnosis6
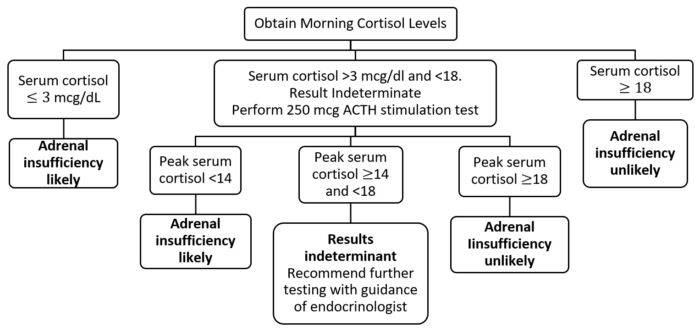
Figure 2. Basic algorithm for diagnosis of chronic adrenal insufficiency. Adapted from Nieman, et al.6
- The morning cortisol level is not a reliable test for patients with abnormal corticosteroid-binding globulin levels, which can be seen in patients with nephrotic syndrome, advanced cirrhosis, or patients taking oral estrogen medications.
- Basal salivary cortisol levels may be helpful if available.
- ACTH, renin, and aldosterone levels are used to classify adrenal insufficiency between primary and central (SAI & TAI) etiologies.
- Diagnosis of adrenal crisis should not be confirmed before treatment. In patients with suspected adrenal crisis, baseline labs should be obtained at the onset of suspicion. If the patient is hypotensive and cortisol is less than 18, a diagnosis of AI should be presumed. ACTH stimulation testing should occur after the patient has stabilized.
- Baseline labs: Basic metabolic panel, cortisol
- If no prior diagnosis of AI: ACTH, aldosterone, and renin
- Baseline labs: Basic metabolic panel, cortisol
Treatment
Chronic Adrenal Insufficiency
- All patients will require glucocorticoid supplementation. Hydrocortisone is the treatment of choice for patients with chronic AI. Dose titration will be necessary and will be based on the clinical course.
- Patients may also require mineralocorticoid therapy based on clinical course and as renin and aldosterone levels are monitored.
Adrenal Crisis

Table 1. Treatment of adrenal crisis. Adapted from Nieman & Desantis.7 Abbreviations: ACTH, adrenocorticotropic hormone; AI, adrenal insufficiency.
Perioperative Corticosteroids4,8
- The amount of cortisol released in response to stress placed on the body by trauma or during surgery is proportional to the stress. Based on the surgery, patients with AI may require perioperative glucocorticoid stress-dosing (Table 2).
- Hydrocortisone is the first-line treatment because it has both glucocorticoid and mineralocorticoid properties.8
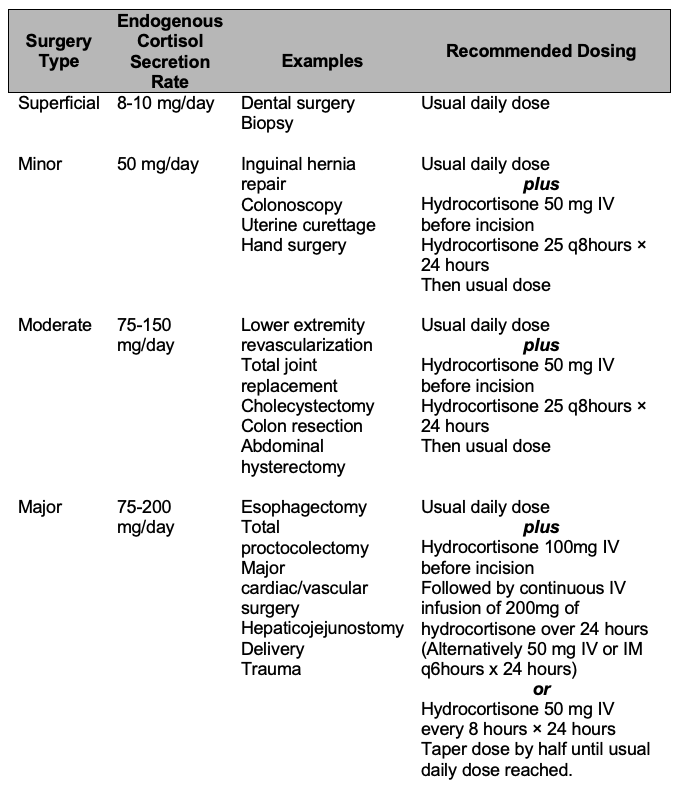
Table 2. Recommended glucocorticoid stress dosage based on surgical type. Adapted from Liu et al.,8 Axelrod,9 and Bornstein et al.10
- Patients who take less than 5 mg/day of prednisone or equivalent or 20 mg/day or equivalent for less than three weeks do not require a stress dose unless they show signs of adrenal crisis perioperatively.
- Patients who take the above doses or more should be administered a stress dose based on the stress response needed for the operation, as they are likely to have a suppressed HPA axis (Table 2).
- Patients taking 5-20 mg/day of prednisone or equivalent doses for three weeks or longer should be referred for HPA axis suppression testing if time permits, as it is unknown if their HPA axis is suppressed.
References
- Nieman LK. Clinical manifestations of adrenal insufficiency in adults. In: Post T, ed. UpToDate; 2024. Accessed Feb 11, 2024. Link
- Martin-Grace J, Dineen R, Sherlock M, Thompson CJ. Adrenal insufficiency: physiology, clinical presentation and diagnostic challenges. Clin Chim Acta. 2020; 505:78–91. PubMed
- Elshimy G, Chippa V, Kaur J, Jeong JM. Adrenal crisis. In: StatPearls (Internet). Treasure Island, FL. StatPearls Publishing; 2024. Accessed Feb 24, 2024. Link
- Seo KH. Perioperative glucocorticoid management based on current evidence. Anesth Pain Med (Seoul). 2021;16(1):8–15. PubMed
- Hahner S, Spinnler C, Fassnacht M, et al. High incidence of adrenal crisis in educated patients with chronic adrenal insufficiency: a prospective study. J Clin Endocrinol Metab. 2015;100(2):407–416. PubMed
- Nieman LK, Raff H, DeSantis A. Diagnosis of adrenal insufficiency in adults. In: Post T, ed. UpToDate; 2024. Accessed Feb 11, 2024. Link
- Nieman LK, DeSantis A. Treatment of adrenal insufficiency in adults. In: Post T, ed. UpToDate; 2024. Accessed Feb 12, 2024. Link
- Liu MM, Reidy AB, Saatee S, Collard CD. Perioperative steroid management: approaches based on current evidence. Anesthesiology. 2017;127(1):166–172. PubMed
- Axelrod L. Perioperative management of patients treated with glucocorticoids. Endocrinol Metab Clin North Am. 2003;32(2):367–383. PubMed
- Bornstein SR, Allolio B, Arlt W, et al. Diagnosis and treatment of primary adrenal insufficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016;101(2):364–389. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.