Copy link
Adductor Canal Block
Last updated: 05/23/2025
Key Points
- The adductor canal is a musculoaponeurotic tunnel bordered by the muscles of the anterior thigh. It contains important neurovascular structures such as the femoral artery, femoral vein, and saphenous nerve.
- The adductor canal block is a common nerve block used in various lower extremity surgeries.
- Pathology involving the adductor canal can cause symptoms resulting from compression of neurovascular structures.
Adductor Canal: Borders
- The adductor canal, also known as “Hunter’s canal” or “subsartorial canal,” is a musculoaponeurotic tunnel that is approximately 8cm in length and runs through the medial thigh. Its borders are defined as follows: (Figure 1).1,2
- Proximal border: The adductor canal begins at the apex (distal end) of the femoral triangle, where the medial border of the adductor longus intersects with the medial border of the sartorius.
- Distal border: The adductor hiatus, a gap between the adductor magnus muscle and the femur, marks the termination of the adductor canal and transmits the contained neurovascular structures from the anterior thigh into the popliteal fossa of the posterior leg.
- Anteromedial border (roof): sartorius muscle
- Lateral border: vastus medialis muscle
- Posterior border: adductor longus and magnus muscles
- The vastoadductor membrane (VAM) is a fascial band connecting the medial edge of the vastus medialis muscle to the lateral edge of the adductor magnus muscle. It forms the roof of the adductor canal, runs immediately deep to the sartorius muscle, and helps create a distinct compartment known as the subsartorial space.3
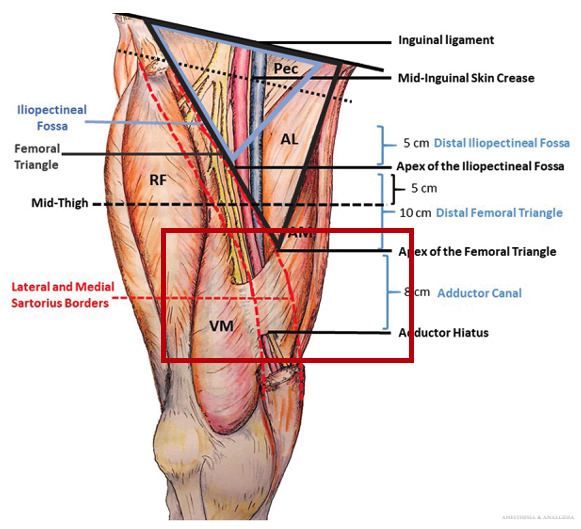
Figure 1. Anatomy of the adductor canal. Abbreviations: ALM, adductor longus muscle; AM, adductor magnus muscle; ASIS, anterior superior iliac spine; IL, inguinal ligament; Pec, pectineus muscle; RFM, rectus femoris muscle; VM, vastus medialis muscle. Source: Woodworth GE, et al. Pro and Con: How Important Is the Exact Location of Adductor Canal and Femoral Triangle Blocks? Anesth Analg. 2023;136(3):458-469.
Contents: Blood Vessels
Femoral Artery
- Proximally, the femoral artery gives off the deep femoral artery before continuing through the femoral triangle as the superficial femoral artery and then entering the adductor canal.
- Travels anterior to the femoral vein and medial to the saphenous nerve as it enters the adductor canal.
- Becomes the popliteal artery as it passes through the adductor hiatus into the popliteal fossa.
Femoral Vein
- Distally, the popliteal vein becomes the femoral vein as it ascends through the adductor hiatus into the adductor canal.
- Travels posterior to the femoral artery.
- Proximally, the femoral vein joins with the great saphenous vein and deep femoral vein to become the common femoral vein.
Contents: Nerves
Saphenous Nerve
- Arising from the L3 and L4 nerve roots, the saphenous nerve is a terminal branch of the posterior division of the femoral nerve.
- As the largest cutaneous branch of the femoral nerve, it is a purely sensory nerve that provides innervation to the anteromedial aspects of the knee, leg, and ankle.
- After descending through the femoral triangle, it enters the adductor canal, initially running lateral to the femoral artery. In the mid-thigh, it crosses anterior to the artery and continues alongside its medial aspect.
- The saphenous nerve exits the adductor canal just proximal to the adductor hiatus, between the sartorius and gracilis muscles, before the femoral artery.4
- After exiting the adductor canal, it gives off an infrapatellar branch that innervates the anteromedial and inferior aspects of the knee.
- Below the knee, it gives off medial crural cutaneous branches that innervate the anteromedial aspect of the lower leg.
Nerve to Vastus Medialis
- The nerve to vastus medialis (NVM) plays a significant role in the sensory innervation of the knee, with some reports suggesting it contributes more than the saphenous nerve due to the presence of sensory fibers within the NVM and its terminal branch, the medial retinacular nerve.5
- A branch of the femoral nerve, the NVM divides into anterolateral branches, which provide motor innervation to the vastus medialis muscle, and posteromedial branches, which provide sensory innervation to both the muscle and the knee joint.
- Previously thought to travel within the adductor canal, the NVM is now known to course through the subsartorial space within its own fascial compartment, separated from the saphenous nerve and femoral vessels by the VAM3 (Figure 2).
- At the mid-thigh, the most common site to perform an adductor canal block, the NVM is typically located 1-2cm lateral to the saphenous nerve (Figure 2).
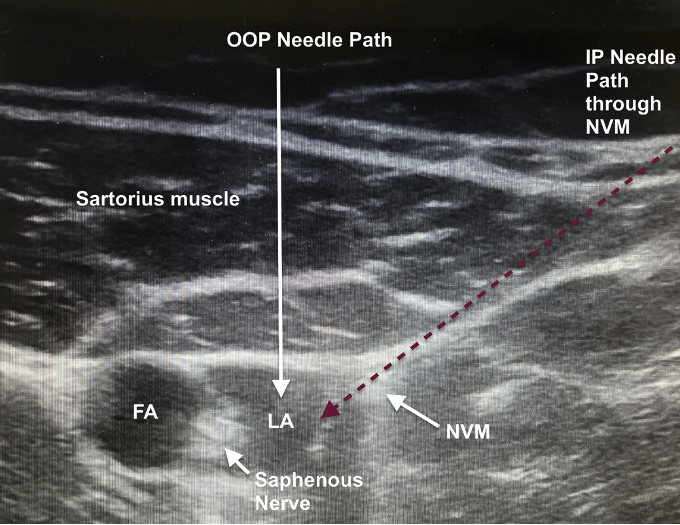
Figure 2. Ultrasound image after an adductor canal block showing the location of the nerve to vastus medialis in relation to the saphenous nerve. Abbreviations: FA = femoral artery; LA = local anesthetic; NVM = nerve to vastus medialis.
Adductor Canal Block
Indications
- Foot and ankle surgery (in combination with a sciatic nerve block)7
- Knee surgery, including total or partial knee arthroplasty, ligamentous knee reconstruction, arthroscopic knee surgery, and tibial plateau surgery
- Saphenous vein stripping or harvesting
Technique
- To perform the block, the patient is typically positioned supine with the leg in slight external rotation (Figure 3).
- A high-frequency linear ultrasound probe is placed transversely and anteromedially at the mid-thigh, at the level where the medial borders of the sartorius and adductor longus muscles meet. The femoral artery lies deep to the sartorius and superficial to the adductor longus.
- The probe is then translated laterally to identify the vastus medialis. The nerve to the vastus medialis lies in the intermuscular plane between the sartorius and vastus medialis muscles, separated from the saphenous nerve by the VAM.
- A needle is inserted in-plane, in a lateral-to-medial direction, beneath the sartorius toward the lateral aspect of the femoral artery. Alternatively, a needle may be inserted out-of-plane to minimize potential injury to the NVM.
- To block the saphenous nerve, 10-20 mL of local anesthetic is injected at the lateral aspect of the femoral artery.
- Local anesthetic may track back from the needle puncture site of an adductor canal block through the VAM, or via fenestrations in the membrane, allowing blockade of both the NVM and the saphenous nerve. However, some advocate for separately targeting the NVM rather than relying solely on diffusion through the fascia.
- If specific coverage of the NVM is desired, such as for knee procedures, 10 mL of local anesthetic can be deposited in the fascial plane between the sartorius and vastus medialis muscles, above the VAM where the NVM is located (Figure 3).
- Because the NVM is often difficult to visualize, a nerve stimulator may be used to evoke a motor response of the medial vastus head, aiding in identification and minimizing the injury to the nerve.7
- Cadaveric studies have demonstrated that a proximal injection within the canal stains both the saphenous nerve and the posteromedial (sensory) branches of the NVM, while sparing the anterolateral (motor) branches, which emerge and course laterally, superior to the proximal adductor canal.8 In contrast, more distal injections within the canal have been shown to stain only the saphenous nerve.
- Another important consideration is that local anesthetic from distal injections within the canal may track along the artery through the adductor hiatus to reach the sciatic nerve, potentially causing lower extremity weakness.9
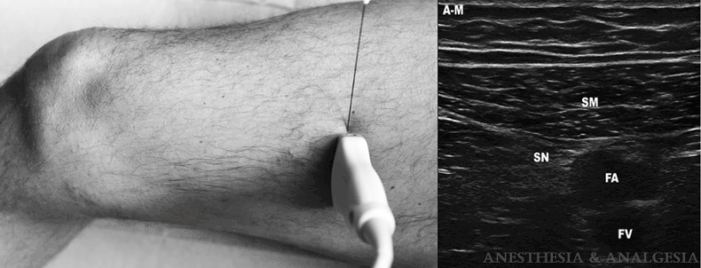
Figure 3. Position of the transducer, direction of the needle insertion, and ultrasound image obtained in the adductor canal block. A-M = antero-medial; SM = sartorius muscle; SN = saphenous nerve; FA = femoral artery; FV = femoral vein. Source: Gautier PE, et al. Distribution of Injectate and Sensory-Motor Blockade After Adductor Canal Block. Anesth Analg. 2016;122(1):279-82.
Adductor Canal Pathologies
Due to the narrow and restrictive nature of the adductor canal space, many of the pathologies of the adductor canal arise from compression of its neurovascular contents.1
Adductor canal compression syndrome is a relatively uncommon disease in which the superficial femoral artery is compressed in the adductor canal. It is often caused by an abnormal musculotendinous band of the adductor magnus or hypertrophy of the adductor magnus or vastus medialis muscles, typically in young males. This condition can lead to arterial occlusion and potential limb ischemia, requiring surgical intervention.
Femoral Artery
- Femoral artery compression can result from various factors such as atherosclerosis, muscle pathologies, anomalous musculotendinous bands, or lesions/tumors inside or outside of the canal. Compression of the artery can result in symptoms of claudication such as pain, weakness, and numbness/tingling, and in severe cases lead to limb ischemia, vessel injury, or arterial thrombosis.
Saphenous Nerve
- The saphenous nerve is most prone to compression as it exits the adductor canal and can lead to pain over the medial aspect of the knee.
Femoral Vein
- Femoral vein compression within the adductor canal is rarely reported but can occur particularly at the outlet of the canal and lead to femoral vein thrombosis or other symptoms of venous stasis.
References
- Mettu S, Saran S, Shirodkar K, et al. Anatomy and pathology of adductor canal (Hunter's canal). Skeletal Radiol. 2025;54(6):1169-77. PubMed
- Wong WY, Bjørn S, Strid JM, et al. Defining the location of the adductor canal using ultrasound. Reg Anesth Pain Med. 2017;42(2):241-5. PubMed
- Tubbs RS, Loukas M, Shoja MM, et al. Anatomy and potential clinical significance of the vastoadductor membrane. Surg Radiol Anat. 2007;29(7):569-73. PubMed
- Burckett-St Laurant D, Peng P, Girón Arango L, et al. The nerves of the adductor canal and the innervation of the knee: An anatomic study. Reg Anesth Pain Med. 2016;41(3):321-7. PubMed
- Bendtsen TF, Moriggl B, Chan V, et al. The optimal analgesic block for total knee arthroplasty. Reg Anesth Pain Med. 2016; 41:711–9. PubMed
- Joe HB, Choo HS, Yoon JS, et al. Adductor canal block versus femoral nerve block combined with sciatic nerve block as an anesthetic technique for hindfoot and ankle surgery: A prospective, randomized noninferiority trial. Medicine (Baltimore). 2016;95(52):e5758. PubMed
- Dooley J, Bullock WM, Kumar AH, et al. Systematic sonographic and evoked motor identification of the nerve to vastus medialis during adductor canal block. Reg Anesth Pain Med. 2020;45(11):937-8. PubMed
- Tran J, Chan VWS, Peng PWH, et al. Evaluation of the proximal adductor canal block injectate spread: a cadaveric study. Reg Anesth Pain Med. 2020; 45:124-30. PubMed
- Gautier PE, Lecoq JP, Vandepitte C, et al. Impairment of sciatic nerve function during adductor canal block. Reg Anesth Pain Med. 2015; 40:85–9. PubMed
Other References
- Gadsden J. Adductor canal block (2024 Update). Duke Regional Anesthesia. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.