Copy link
Acute Respiratory Failure in Pregnancy: Clinical Presentation and Diagnosis
Last updated: 07/30/2025
Key Points
- Acute respiratory failure in pregnancy may be due to obstetric conditions, including preeclampsia, or nonobstetric related conditions, including infection, aspiration, and/or hemorrhage.
- The physiologic changes of pregnancy require consideration when monitoring the evolution of illness and initiating treatment.
- Acute respiratory distress syndrome (ARDS) in pregnancy may be associated with nonobstetric illness or obstetric-specific conditions.
Introduction
- Acute respiratory failure is estimated to affect 15-130/100,000 deliveries or 0.1-0.3% of pregnancies.1-4
- Pregnancy may predispose patients to developing ARDS secondary to increased blood volume, decreased oncotic pressure, upregulation of the inflammatory response, and increased capillary leak.5
- Perinatal morbidity and mortality are increased in pregnancies associated with maternal respiratory failure.1
Clinical Presentation
- Presenting signs and symptoms include cough, dyspnea, fatigue, and fever.
- Physical exam findings may be significant for tachypnea, use of accessory respiratory muscles, crackles and/or wheezing on lung auscultation, hypoxia, and altered mental status.
- Vital sign changes may include tachycardia, hypotension in the setting of infection, increased respiratory rate, and hypoxemia (oxygen saturation < 95%).
- Laboratory changes may include hypercarbia (PaCO2 > 40 mmHg) and/or hypoxemia (PaO2 < 75 mmHg). Patients may exhibit early hypocarbia (PaCO2 < 28 mmHg) with tachypnea, which can evolve into hypercarbia as they begin to tire.
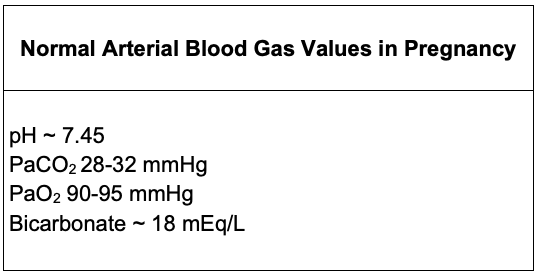
Table 1. Normal arterial blood gas values in parturients
Clinical Diagnosis
ARDS Definition
The Berlin criteria for ARDS include the following:2,3
- Acute onset <7d between risk factor exposure and the development of ARDS
- Abnormal chest imaging (bilateral infiltrates on chest x-ray not fully attributed to cardiac effusions, lobar collapse, or nodule)
- Exclusion of pulmonary edema
- Oxygenation deficits:
- Mild: PaO2:FiO2 (P:F ratio) 200 to <300 mmHg with PEEP or CPAP ≥5 cmH2O
- Moderate: P:F ratio 100 to <200 mmHg with PEEP or CPAP ≥5 cmH2O
- Severe: P:F ratio ≥100 mmHg with PEEP or CPAP ≥5 cmH2O
Differential Diagnosis
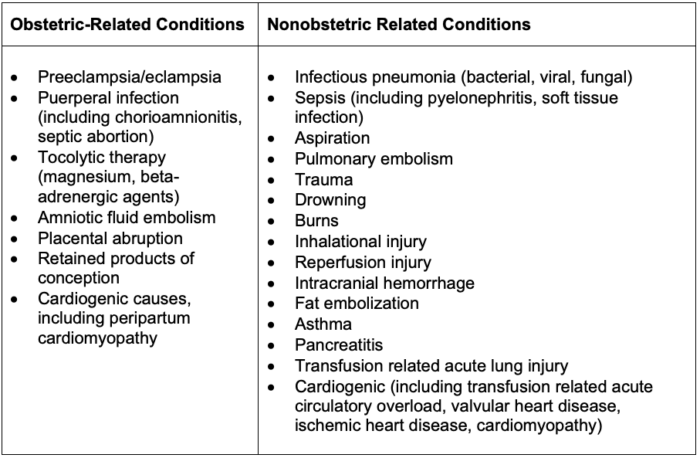
Table 2. Differential for acute respiratory failure in parturients
Initial Management
- Oxygen supplementation to maintain a goal oxygen saturation of ≥ 92% (ideally >95% due to higher oxygen consumption and lower respiratory reserve).
Awake, passive prone positioning is recommended in pregnant patients if feasible and may reduce the risk of intubation.5 - Advanced interventions and obstetric management are discussed in Part II of this summary.
Long-Term Outcomes
- Mortality rates vary across studies from 25-60% in older studies, with newer studies suggesting improved outcomes and mortality rates closer to 5-10%.5
- Mortality risk is associated with a prolonged need for mechanical ventilation, renal failure requiring renal replacement therapy, liver failure, amniotic fluid embolism, septic emboli, and puerperal infection.
- ICU admission is associated with reduced maternal quality of life at 6 months.
- Psychological support is recommended for patients who have had pregnancies complicated by perinatal morbidity and/or mortality or significant organ failure requiring advanced therapies (hemodialysis, invasive ventilation, extracorporeal membrane oxygenation) to support long-term mental health, given the high risk of anxiety, depression, and posttraumatic stress syndrome.
References
- Mighty HE. Acute respiratory failure in pregnancy. Clin Obstet Gynecol. 2010;53(2):360-8. PubMed
- Duarte AG. ARDS in pregnancy. Clin Obstet Gynecol. 2014;57(4):862-70. PubMed
- Watts A, Duarte AG. Acute respiratory distress syndrome in pregnancy: Updates in principles and practice. Clin Obstet Gynecol. 2023;66(1):208-22. PubMed
- Lapinsky SE. Acute respiratory failure in pregnancy. Obstet Med. 2015;8(3):126-32. PubMed
- Rush B, Martinka P, Kilb B, et al. Acute respiratory distress syndrome in pregnant women. Obstet Gynecol. 2017;129(3):530-5. PubMed
Other References
- Naoum E. OpenAnesthesia. OA-SOAP Fellow Webinar Series. Extracorporeal Life Support in Pregnancy. Published: October 1, 2021. Accessed: July 30, 2025. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.