Copy link
Achondroplasia
Last updated: 09/24/2025
Key Points
- Achondroplasia is the most common form of skeletal dysplasia, affecting approximately one in every 40,000 births. Only about one out of five cases is hereditary: the rest result from spontaneous mutations.1
- Achondroplasia is the most common cause of disproportionate dwarfism.
- Achondroplasia patients can present unique challenges to anesthesia providers, such as a higher risk of bleeding, cardiopulmonary complications, abnormal healing, technical difficulties with placing regional blocks, and patient positioning. Understanding these challenges can help anesthesia providers better care for their patients.
Introduction
- Achondroplasia is a genetic condition affecting the fibroblast growth factor receptor, slowing down the growth of bone in the cartilage of the growth plate. This leads to shorter bones, abnormally shaped bones, and short stature.2
- Twenty to 50 percent of children born with the condition will experience neurological impairment.
- Characteristically, patients have normal intelligence with foramen magnum stenosis, genu varum, kyphoscoliosis, and short stature.
Epidemiology
- Achondroplasia occurs in approximately 1:20,000 to 1:30,000 live births per year.
- As achondroplasia follows an autosomal dominant inheritance pattern, both males and females are equally affected.3
- There is an increase in the estimated occurrence rate for this form of skeletal dysplasia with increasing paternal age.3
Pathophysiology
- Achondroplasia results from a point mutation in the gene coding for the transmembrane portion of fibroblast growth factor receptor 3 (FGFR3), which resides on the short arm of chromosome 4.1
- In more than 80% of cases, the condition occurs due to a sporadic or de novo mutation. The other 20% exhibit an autosomal dominant inheritance pattern. It is fully penetrant, meaning all individuals who have the FGFR3 heterozygous pathogenic variant show the clinical manifestations of the disorder.
- The homozygous form is usually incompatible with life, usually resulting in early neonatal death from respiratory insufficiency due to a small thoracic cage and neurologic deficits from cervicomedullary stenosis.
- The resultant abnormal chondroid production affects endochondral ossification, resulting in decreased linear bone growth, among other functions. This pathologic process generally spares intramembranous ossification, which takes place in flat bones such as those in the skull (except the base of the skull), face, and clavicles.4
Clinical Presentation
Musculoskeletal System
- Patients with achondroplasia are typically short-statured with poor muscle tone and loose joints. They have shortened arms and legs (rhizomelia), with prominent shortening of proximal limbs when compared to distal. Those affected have an average torso size, and their sitting height may be within normal limits, but their standing height will often be below the 5th percentile.5
- They also have varus deformities of the legs with flat feet that are short and broad. This deformity is structurally complex, originating from a combination of internal tibial torsion, lateral bowing, and some dynamic instability and laxity of the knee.
- They may present with limited elbow extension. A prominent gap between the middle and ring fingers (trident hand) with short digits (brachydactyly) is a common finding.
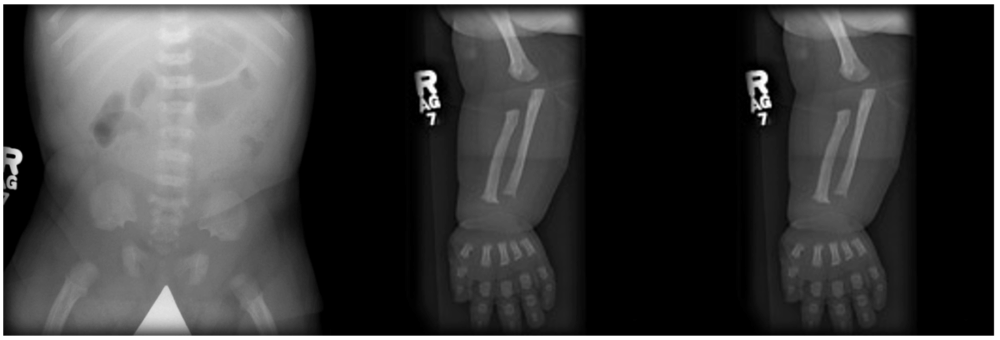
Figure 1. Plain radiographs of the upper and lower limbs demonstrate shortened long bones. The lumbar spine has a decreased transverse diameter. The iliac wings have a tombstone morphology. Gaillard F, Walizai T, Ranchod A, et al. Achondroplasia. Reference article, Radiopaedia.org. Accessed on 24 Sep 2025. Link
- They present with a large head size (macrocephaly), prominent forehead bossing, and a mid-face hypoplasia manifesting as a flattened nasal bridge and crowded, misaligned teeth (Figure 2). The pelvis is uniquely described to be champagne glass-shaped. This radiological appearance is characterized by flattened iliac blades, horizontal acetabulum, and narrowed sacroiliac notches.
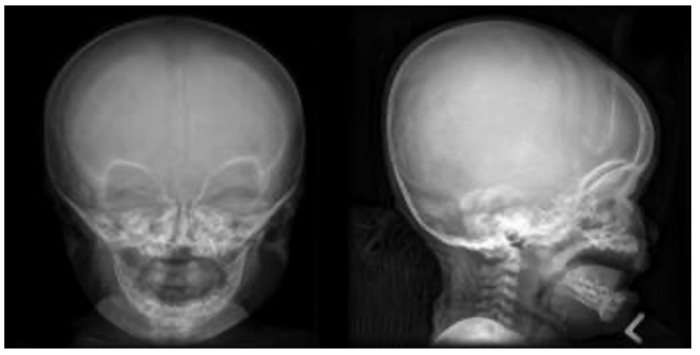
Figure 2. Relatively large cranial vault with small skull base, prominent forehead with a depressed nasal bridge. Gaillard F, Walizai T, Ranchod A, et al. Achondroplasia. Reference article, Radiopaedia.org. Accessed on 24 Sep 2025. Link
Spinal Deformities
- Patients with achondroplasia present with poor muscle tone and loose joints. Thoracolumbar kyphoscoliosis is a common presentation. Upper cervical instability is uncommon, T12 and L1 apical wedging are frequently seen on X-rays, and the deformity usually involves vertebrae of T10 to L4. A narrow vertebral canal increases the risk for cord compression.
Developmental motor delay is also associated with unresolved thoracolumbar kyphoscoliosis. It is recommended that patients with kyphotic curves between 20 and 40 degrees be monitored for progressive deformity and symptoms of spinal cord compression. As the child begins to stand and walk, lumbosacral hyperlordosis may become apparent. This additional deformity is likely due to excessive anterior pelvic tilt in these children while standing.5 - Foramen magnum stenosis is the first spinal manifestation in an infant with achondroplasia (Figure 3). Common presenting symptoms include respiratory difficulty, excessive snoring, or apnea. Other symptoms that can present are apnea, lower cranial nerve dysfunction, difficulty swallowing, hyperreflexia, hypotonia, weakness/paresis, and clonus.5
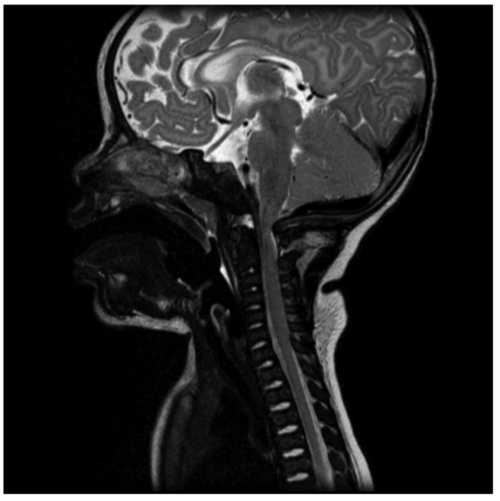
Figure 3. Foramen magnum stenosis with significant compression of the cervicomedullary junction. Gaillard F, Walizai T, Ranchod A, et al. Achondroplasia. Reference article, Radiopaedia.org. Accessed on 24 Sep 2025. Link
Sleep-Disordered Breathing
- The American Academy of Pediatrics recommends a sleep study and then computed tomography or magnetic resonance imaging, if the sleep study is positive. Sleep-disordered breathing in these children could be multifactorial. Central sleep apnea may occur due to cervicomedullary compression.6
- The etiology of obstructive sleep apnea in these patients is multifactorial and results from:
compression of the lower motor neurons, altered craniofacial features, small upper airway, adenoidal hypertrophy, and hypotonia of nasopharyngeal airway muscles. In infants, hypotonia and attenuated arousal response could play a role in sudden infant death syndrome.7
Pulmonary System and Ear, Nose, and Throat
- Restrictive lung disease resulting from kyphoscoliosis may lead to pulmonary hypertension.
- Frequent middle ear infections may lead to hearing loss.
Common Surgical Interventions
Common surgical interventions in patients with achondroplasia include:
- Ventriculoperitoneal shunt placement
- Chiari decompression
- Decompression for spinal canal stenoses
- Spinal fusion for kyphoscoliosis
- Genu varus correction [hemi epiphysiodesis]
- Tonsillectomy/pharyngoplasty for airway obstruction
- Tympanostomy tubes
Anesthetic Considerations
Airway Considerations
- Difficult mask ventilation, difficult laryngoscopy and intubation should be expected in these patients. Endotracheal tube correlates with that expected for age. Due consideration should be given to a narrow nasopharynx due to midface hypoplasia when planning a nasal intubation. Mayhew et al report better endotracheal tube size prediction with weight rather than age in this patient population.8
- Fiberoptic bronchoscopy or video laryngoscopy-guided intubation should be considered with manual inline stabilization when C spine mobility is of concern.9
- Downsizing the size of the endotracheal tube should be considered due to a narrow nasopharynx.
- Supraglottic airway devices may have to be downsized because of a large tongue and a small mouth.10
- Clinicians should plan intraoperative ventilation strategies depending on the degree of restricted lung disease. Mechanical ventilation should be initially set to 6 mL/kg of ideal body weight for height and adjusted as necessary.
Positioning Concerns
- Careful consideration of positioning and padding is necessary to accommodate lax knee joints with hypermobility, as well as contracted elbow/hip joints.
- Active warming should be considered as a high body surface area-weight ratio and large heads may increase heat loss, especially in younger patients.
Regional Anesthesia Considerations
- The unique anatomy in achondroplasia that includes hypertrophy of superior and inferior articular facets, shortened and thickened pedicles of the vertebral body from premature fusion with scalloping on the posterior surface, prominent bulging of intervertebral discs, spinal canal tapering caudally from decreases in the interpedicular distance in the lumbar region (as opposed to widening caudally in normal anatomy), and thin dura. These mechanical features can lead to spinal stenosis and nerve root compromise. In patients who had previously undergone lumbar decompression surgeries, scar tissue and altered anatomy can further complicate neuraxial techniques.11,12
- Dose and volume calculation would have to be personalized for each patient, as blocks can present with unpredictable height or uneven coverage. Consider lower local anesthetic volumes.
- Since local anesthetic (LA) doses and spread of LA can vary from patient to patient, epidural blocks are better titratable than single-shot spinal blocks.
- Ultrasound can facilitate access to neuraxial spaces. Fluoroscopy can help with positioning catheter tips.13
Pharmacological Considerations
- Neuromonitoring is often used in these patients either because of intraoperative surgical needs [e.g., scoliosis correction, spine decompression] or because of ‘spine at risk’ diagnosis. Paralytics should be avoided if neuro monitoring with motor evoked potentials is planned. Pharmacologic management to optimize somatosensory evoked potentials monitoring should be employed per standard recommendations.14
- Due consideration should be given to respiratory depression from opioids. Multimodal analgesia techniques with non-steroidal anti-inflammatory drugs and regional blocks should be employed when feasible.
References
- Horton WA, Hall JG, Hecht JT. Achondroplasia. Lancet. 2007;370(9582):162–172. PubMed
- Vajo Z, Francomano CA, Wilkin DJ. The molecular and genetic basis of fibroblast growth factor receptor 3 disorders: the achondroplasia family of skeletal dysplasias, Muenke craniosynostosis, and Crouzon syndrome with acanthosis nigricans. Endocr Rev. 2000;21(1):23-39. PubMed
- Coi A, Santoro M, Garne E, et al. Epidemiology of achondroplasia: A population-based study in Europe. Am J Med Genet A. 2019;179(9):1791-98. PubMed
- Di Nardo SK. Anesthetic consideration for the achondroplastic dwarf. AANA J 1988;56(1):422 PubMed
- Richette P, Bardin T, Stheneur C. Achondroplasia: from genotype to phenotype. Joint Bone Spine. 2008;75(2):125-30. Link
- American Academy of Pediatrics Committee on Genetics. Health supervision for children with achondroplasia. Pediatrics. 1995;95(3):443–451. PubMed
- Sisk EA, Heatley DG, Borowski BJ, et al. Obstructive sleep apnea in children with achondroplasia: Surgical and anesthetic considerations. Otolaryngol Head Neck Surg. 1999; 120:248-54. PubMed
- Mayhew JF, Katz J, Miner M, et al. Anaesthesia for the achondroplastic dwarf. Can Anaesth Soc J. 1986;33(2):216-21. PubMed
- Krishnan BS, Eipe N, Korula G. Anaesthetic management of a patient with achondroplasia. Paediatr Anaesth. 2003;13(6):547-9. PubMed
- Kalla GN, Fening E, Obiaya MO. Anaesthetic management of achondroplasia. Br J Anaesth. 1986;58(1):117-9. PubMed
- Giglio GC, Passariello R, Pagnotta G, Crostelli M, Ascani E. Anatomy of the lumbar spine in achondroplasia. Basic Life Sci. 1988; 48:227-39. PubMed
- Carson BS, Groves M, Yassari R: Neurologic problems of the spine in achondroplasia. Schmidek and Sweet’s Operative Neurosurgical Techniques. Quinones-Hinojosa A (ed): Elsevier, Amsterdam, Netherlands; 2012. 1:2091-9.
- Wight JM, Male D, Combeer A: Ultrasound-guided combined spinal-epidural anaesthesia for elective caesarean section in a patient with achondroplasia. Int J Obstet Anesth. 2013, 22:168-9. PubMed
- Craven C, Jankovic I, Dyson E, et al. Association of the achondroplasia foramen magnum score and intraoperative neuromonitoring. Arch Dis Child. 2024;109(9):755-758. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.