Copy link
Hyperthyroidism
Last updated: 05/30/2025
Key Points
- Hyperthyroidism results from excessive thyroid hormone synthesis or secretion, commonly due to Graves' disease, toxic multinodular goiter, toxic adenoma, or thyroiditis.
- Patients with hyperthyroidism typically present with symptoms of increased sympathetic activity: anxiety, tachycardia, tremor, and weakness. Clinical presentation can range widely.
- Anesthetic management of hyperthyroid patients involves achieving a euthyroid state preoperatively, controlling sympathetic stimulation intraoperatively, and careful postoperative monitoring for complications such as arrhythmias or thyroid storm.
- Thyroid storm is a life-threatening condition requiring immediate management to reduce thyroid hormone synthesis, minimize adrenergic effects, and provide supportive care.
Introduction
- Hyperthyroidism is an endocrine disorder characterized by excessive synthesis and secretion of thyroid hormones, leading to a hypermetabolic state.1
- Hyperthyroidism affects approximately 2.5% of adults globally, with higher prevalence in iodine-deficient regions, and is more common among women and individuals over 60 years of age.2,3
- Hyperthyroidism exists along a spectrum, with slight hormone elevations and minimal clinical symptoms classified as subclinical hyperthyroidism that is often occult, whereas higher hormone elevations leading to more significant symptoms are often described as overt hyperthyroidism or thyrotoxicosis.2–4
- Thyroid storm is a severe presentation of exacerbated hyperthyroidism with multiorgan involvement and has a high mortality rate.1,5
Etiology
- Almost all hyperthyroidism is primary hyperthyroidism, driven by the overproduction or inappropriate release of thyroid hormone at the thyroid gland, with an associated low level of thyroid-stimulating hormone (TSH) via negative feedback (Figure 1).1,6
- Much more rarely, a pituitary lesion can instigate the thyroid gland’s overproduction through pathological release of TSH, and would be classified as secondary hyperthyroidism.4,6
- Further upstream in the hypothalamic-pituitary-thyroid axis, a hypothalamic lesion causing hyperthyroidism would be tertiary, and is extremely rare.4
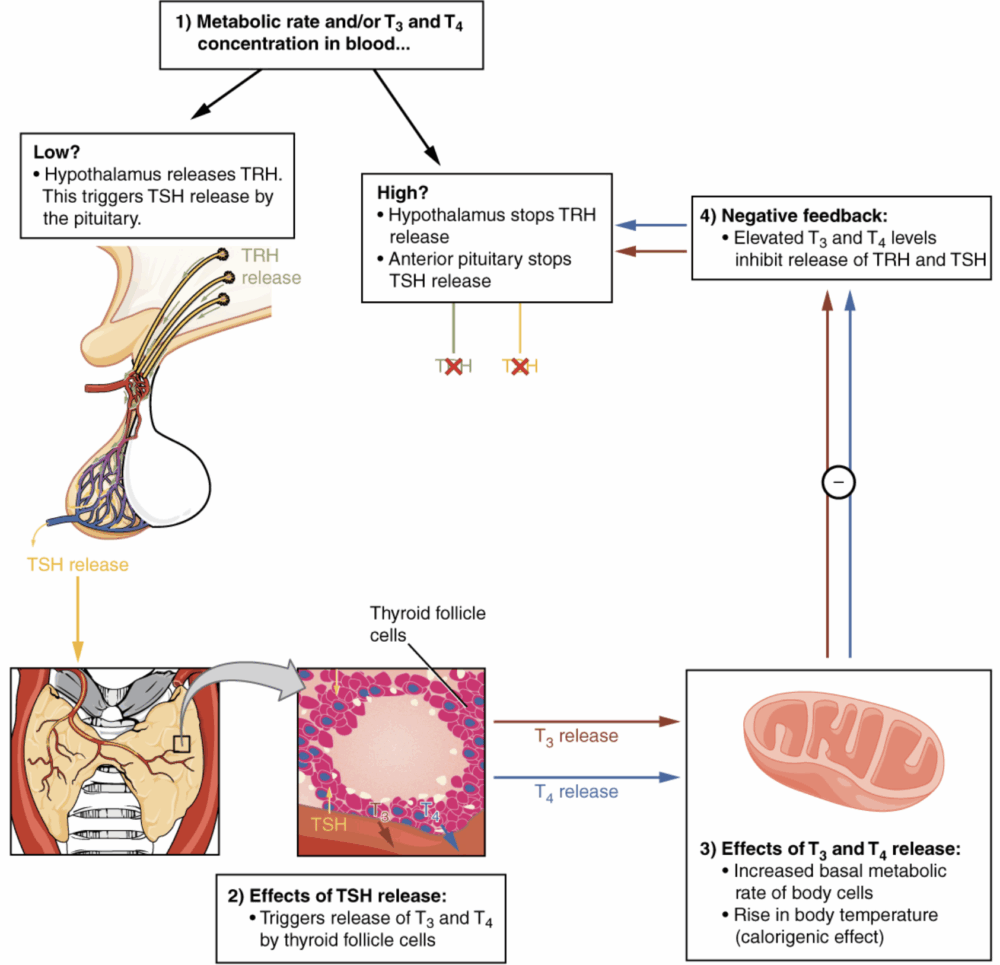
Figure 1. Negative feedback mechanism of thyroid hormone synthesis. Source: OpenStax College. Wikimedia Commons. 2013. Accessed 26 February 2025. Link
- The three most common causes of hyperthyroidism are Graves’ disease, toxic multinodular goiter, and toxic adenoma. These are all categorized as primary hyperthyroidism.2,6
Graves Disease2,7
- It is an autoimmune disorder and the most common cause of hyperthyroidism.
- Thyroid-stimulating immunoglobulins bind to TSH receptors, mimicking TSH action and stimulating thyroid hormone synthesis and gland growth, with diffuse enlargement.
- It may present with proptosis or pretibial myxedema (Figure 2).
Toxic Multinodular Goiter2,6
- Multiple benign nodules within the thyroid gland that autonomously produce thyroid hormones
- Often developing in regions with iodine deficiency
Toxic Adenoma2
- A single benign thyroid nodule that autonomously secretes thyroid hormones

Figure 2. Proptosis and lid retraction from Grave’s disease. Source: Trobe J. Wikimedia Commons. 2011. Accessed 26 February 2025. Link
- Primary hyperthyroidism has several other potential causes. Thyroiditis can cause inflammation of thyroid follicular cells, releasing stored thyroid hormone, and can be due to Hashimoto’s thyroiditis, postpartum thyroiditis, and drug-induced thyroiditis.7,8
- Excessive replacement of thyroid hormone creates hyperthyroidism, and iodine administration can also induce hyperthyroidism, classically via iodinated contrast or amiodarone administration.4 Thyroid carcinoma can also present with hyperthyroidism.7
Pathophysiology
- Excess thyroid hormones affect nearly every tissue, increasing basal metabolic rate and thermogenesis through the upregulation of beta-adrenergic receptors.7 The degree of hormone elevation roughly correlates with the severity of symptoms, leading to the spectrum of clinical presentation ranging from subclinical to mild to severe.4,8
- Common presenting symptoms include palpitations, weight loss, and anxiety, among others (Table 1). In more severe presentations, the pathophysiologic changes most relevant to anesthetic considerations include effects on the cardiovascular and pulmonary systems, including any airway compression from a large goiter.1
Cardiovascular
- Palpitations or tachycardia, including arrhythmias such as atrial fibrillation and associated embolic risks
- Increased heart rate and contractility, leading to elevated cardiac output.6 In severe cases, it may present with high-output heart failure.1
- Systolic hypertension but decreased systemic vascular resistance;1 may present with widened pulse pressure.7
Pulmonary
- Dyspnea on exertion may be a presenting symptom.4
- Cardiogenic pulmonary edema may be present secondary to heart failure.5
- Musculoskeletal effects of thyrotoxicosis may cause decreases in respiratory muscle strength.4
- Significant goiter may cause compressive symptoms with stridor, dyspnea, or dysphagia.1
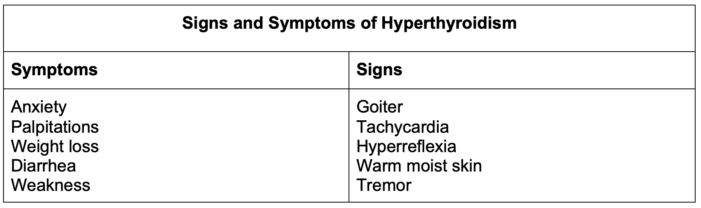
Table 1. Signs and symptoms of hyperthyroidism. Adapted from references 1, 4 and 6.
Anesthetic Management
- Effective perioperative management of hyperthyroidism involves achieving a euthyroid state, controlling hyperadrenergic symptoms, securing the airway, and monitoring for postoperative complications.
Preoperative
- Subclinical or well-controlled hyperthyroidism rarely increases perioperative risks significantly, though patients are still at increased risk for perioperative arrhythmias such as atrial fibrillation.1
- Symptomatic hyperthyroidism or thyrotoxicosis includes patients who are newly diagnosed or are not yet optimized on therapy, and such patients should ideally have their thyroid disease optimized prior to surgery.2,7 Medical management of thyrotoxicosis includes decreasing hormone synthesis and controlling symptoms.6
- Decreasing thyroid hormone synthesis: Antithyroid drugs such as methimazole or propylthiouracil inhibit thyroid hormone synthesis.7 Inorganic iodine administration also inhibits thyroid hormone synthesis and release.6 Of note, antithyroid drugs should be started before iodide treatment, to avoid worsening thyrotoxicosis.7
- Controlling symptoms: Beta-adrenergic antagonists help control the hyperadrenergic symptoms.6,7 Propranolol is typically used, as it also inhibits the peripheral conversion of thyroid hormone.1
Intraoperative
- Anesthetic depth is typically aimed at preventing exaggerated sympathetic responses to surgery.7 All inhalational anesthetics are generally acceptable.1 Medications that stimulate the sympathetic nervous system, such as ketamine and ephedrine, are typically avoided.6
- Goiters may compress the airway, and external goiter size is not perfectly predictive of the risk of difficult intubation or tracheal compression.7 Although substernal goiters can theoretically cause intrathoracic compression after induction of general anesthesia, classically thyroid goiters more commonly cause lateral deviation of the trachea without full collapse.1,7 Preoperative imaging and airway examination can help guide difficult airway planning.7
- Given the hyperthyroidism cardiovascular manifestations of arrhythmias, decreased systemic vascular resistance, potential high-output heart failure, and increased sensitivity to catecholamines, close vigilance to cardiac monitoring is necessary, and there should be a low threshold to use invasive blood pressure monitoring in uncontrolled thyrotoxicosis.1,6
- Intraoperative beta-adrenergic antagonists or calcium channel antagonists can be used to control refractory tachycardia or hypertension.2
Postoperative
- Hyperthyroid patients undergoing surgery are at increased risk for perioperative arrhythmia, which can present postoperatively.4
- Surgical stimulation in patients with significant uncontrolled hyperthyroidism can precipitate qthyroid storm, an exaggerated clinical thyrotoxicosis.5
- Surgery on the thyroid gland itself has several potential airway complications. Recurrent laryngeal nerve injury can lead to hoarseness or airway obstruction, especially with bilateral injury.1 Postoperative hematoma can cause direct tracheal compression.7 Hypocalcemia secondary to parathyroid injury can lead to laryngeal stridor.7
- Please see the OA summary on Anesthesia for Thyroidectomy for more details. Link
Thyroid Storm
- Thyroid storm is a life-threatening exacerbation of hyperthyroidism with exaggerated clinical manifestations, typically after acute illness, trauma, or surgery.1 Mortality rates of patients with thyroid storm are approximately 20%.6
- Clinically, thyroid storm presents as acute multiorgan decompensation after an insult, rather than the slow worsening of untreated severe hyperthyroidism.4 The main features of thyroid storm include tachycardia, fever, central nervous system disturbances, and gastrointestinal symptoms.4 Of note, there is significant overlap between thyroid storm and malignant hyperthermia, and distinguishing between the two can be difficult, especially in an intraoperative environment.6
Thyroid Storm Management
- Reduce thyroid hormone synthesis with antithyroid medications such as methimazole or propylthiouracil (which are not available in intravenous formulations).6
- Treat dehydration with intravenous fluids to correct dehydration and maintain hemodynamic stability.4
- Reduce hyperthermia with cooling blankets and antipyretics such as acetaminophen.7
- Mitigate increased adrenergic tone with beta-adrenergic antagonists.1
- Consider steroid administration for empiric adrenal insufficiency treatment, and also to reduce thyroid hormone secretion and conversion.4
- Similar to less acute hyperthyroidism management, after initiation of antithyroid medications, iodine is typically used.4
- Avoid any elective or nonemergent surgery until stabilized.1 If urgent surgery is needed, use invasive hemodynamic monitoring.7
References
- Sweitzer B, Opera A, Gerlach R. Anesthetic Implications of Concurrent Diseases. In: Gropper M, ed. Miller’s Anesthesia. Volume 1. Tenth edition. Elsevier; 2025:873-929.
- Sharma MP, Cetera B. Thyroid disease and surgery. Anaesth Intensive Care Med. 2020;21(11):558-571. Link
- Terefe M, Belay Bizuneh Y, Addisu Nigatu Y, Yaregal Melesse D. Perioperative management of the thyrotoxic patients: A systematic review. Ann Med Surg. 2022; 81:104487. PubMed
- Sipos J, Cance W. Thyroid Disorders. In: Civetta J, ed. Taylor & Kirby’s Critical Care Medicine. Fifth edition. Wolters Kluwer; 2018: e376-e386.
- de Mul N, Damstra J, Nieveen van Dijkum EJM, et al. Risk of perioperative thyroid storm in hyperthyroid patients: a systematic review. Br J Anaesth. 2021;127(6):879-889. PubMed
- Zuo L, Dillman D. Endocrine Disease. In: Hines R, Jones S, eds. Stoelting’s Anesthesia and Co-Existing Disease. Eighth edition. Elsevier; 2022:439-464.
- Schwartz J, Akhtar S. Endocrine Function. In: Cullen B, Stock C, eds. Barash, Cullen, and Stoelting’s Clinical Anesthesia. Ninth edition. Wolters Kluwer; 2024:274-1303.
- Chaker L, Cooper DS, Walsh JP, Peeters RP. Hyperthyroidism. Lancet. 2024;403(10428):768-80. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.