Copy link
Coagulation Changes in Pregnancy
Last updated: 09/18/2024
Key Points
- Pregnancy is a hypercoagulable state.
- Amounts of clotting factors change throughout pregnancy, with the largest difference at full term.
- Laboratory tests should be interpreted in the context of the expected normal range for pregnancy.
- In patients with thrombocytopenia, the risk of spinal epidural hematoma is low for a platelet count of ≥70,000/µL in patients with negative bleeding histories.
Introduction
- The coagulation system undergoes many changes during pregnancy, which can lead to a hypercoagulable state, especially at term. Pregnancy is characterized by:
- four to 5 times increased risk for venous thromboembolism in pregnancy compared to nonpregnant; and1
- sixty times increased risk for venous thromboembolism in the first 3 months postpartum.
- Risk factors for venous thromboembolism in pregnancy include thrombophilia, fluid shifts, obesity, age older than 35 years, lupus, heart disease, sickle cell disease, postpartum infection, and transfusion.1
- Theoretically, this state is an evolutionary protection against hemorrhage in childbirth. However, this makes pregnancy a risk factor for thrombosis, and thromboembolism is an important cause of maternal morbidity.
Review of Coagulation Changes in Pregnancy
Platelets
- Platelet count decreases the most in the 3rd trimester. This is due to hemodilution and increased destruction (consumption).
- Gestational thrombocytopenia is diagnosed when the platelet count decreases to less than 150,000/µL.
- The incidence of the different causes of thrombocytopenia in pregnancy is as follows.2
- Gestational thrombocytopenia: 5-11.6%
- 75% of all cases of thrombocytopenia in pregnancy.
- Preeclampsia: 5-8%
- Immune thrombocytopenic purpura: Less than 1%
- HELLP Syndrome: Less than 1%
- Gestational thrombocytopenia: 5-11.6%
Clotting Factors
- Increase: fibrinogen, Factors VII, VIII, IX, X, XII, and vWF.
- Decrease: Factor XIII, protein S
Fibrinolysis
- Decreased due to decreased tissue plasminogen activator (t-PA) activity3
- Plasminogen activator inhibitor-1 (PAI-) from the endothelium and PAI-2 from the placenta increase throughout pregnancy.
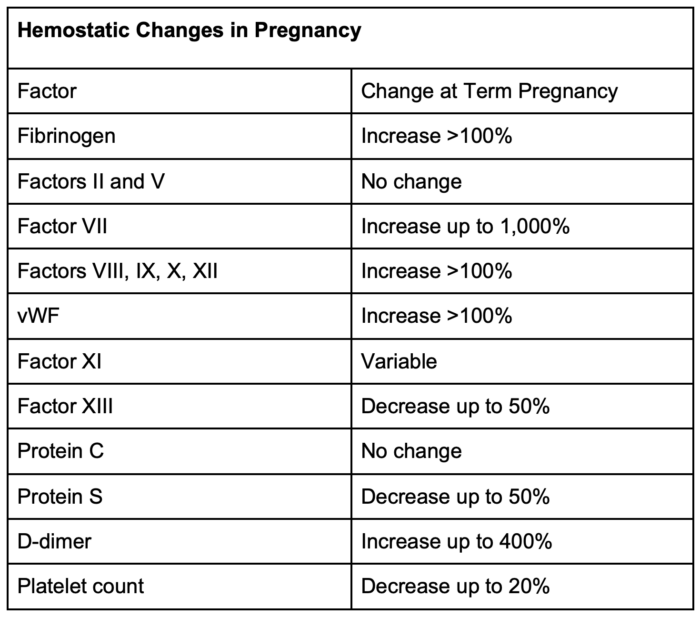
Table 1. Hemostatic changes in pregnancy
Approaches to Assessing Coagulation in Pregnancy
Patient History
- A thorough history can help assess the severity of bleeding or clotting disorders. It is important to elucidate whether events took place before or during pregnancy.
- The components of bleeding history that should be elucidated include:4
- Heavy menstrual bleeding
- Problem with hemostasis
- Surgical bleeding
- Bleeding related to dental work
- Postpartum hemorrhage
- Nontraumatic major bleed not related to anatomical defect
- Intracranial bleed
- Gastrointestinal bleed
- Musculoskeletal bleed
- Symptoms:
- Epistaxis
- Easy bruising
- Bleeding after minor injury
- Family history of bleeding problems or bleeding disorder
Traditional Laboratory Assessments
Platelet Count
- The average platelet count is lower in pregnant women (approximately 213,000/µL)
- The prevalence of thrombocytopenia in parturients is ~5-10%3
- Platelet count assesses platelet number, not function.
Platelet Function Analyzer
- Analyzes platelet function in vitro
- PFA-100 is one type of analyzer. It gives a value of closure time (CT), which is the time needed for platelets from a whole blood sample to form a plug that occludes a membrane.
- Does not correlate with platelet count or TEG maximum amplitude in parturients
- CT is prolonged in patients with severe preeclampsia, though not in mild preeclampsia.5
- It may be less accurate in patients with severe thrombocytopenia.6
- No studies have assessed using this test to determine if one can safely place an epidural.
- PFA-100 is one type of analyzer. It gives a value of closure time (CT), which is the time needed for platelets from a whole blood sample to form a plug that occludes a membrane.
Coagulation Tests
- Coagulation tests focus on clotting factors, not the efficacy of clot formation.6
- Prothrombin time (PT) and activated partial thromboplastin time (aPTT) are shortened in normal pregnancy.
- PT or aPTT prolongation greater than or equal to 1.5 times normal are recommended values to trigger transfusion. Still, this prolongation varies in massive hemorrhage situations, and the PT may be more reliable.7
- Bleeding time is no longer routinely used due to low reliability and reproducibility.
Viscoelastic Testing
- Viscoelastic tests are real-time measures of clot formation, strength, and lysis.
- Two forms of viscoelastic tests are thromboelastography (TEG) and rotational thromboelastometry (ROTEM).
- At term and even more so in labor, clot formation is quicker with a larger maximum amplitude.8
- Numerical “normal” values in the pregnant state are different from nonpregnant and vary widely by study and institution as well as stage of pregnancy9 (Table 2).
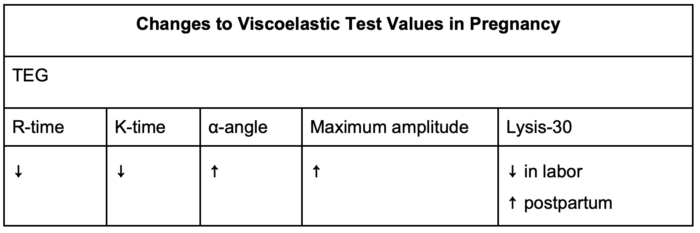
Table 2: Changes to viscoelastic test values in pregnancy
SOAP Consensus Guidelines
- The Society for Obstetric Anesthesia and Perinatology (SOAP) published a consensus statement on the anesthetic management of pregnant and postpartum women receiving thromboprophylaxis or higher-dose anticoagulants.10
- In patients who are on anticoagulation, there is no standardized test to assess the risk of spinal epidural hematoma.
- To date, no data correlate aPTT, anti-Xa, TEG, or ROTEM with the risk of spinal epidural hematoma.
- SOAP’s interdisciplinary consensus statement on neuraxial procedures in obstetric patients discusses the safety of neuraxial blocks in patients with thrombocytopenia4 (Figure 1).
- Known etiology
- Platelet count ≥70,000/µL: likely safe to proceed
- Platelet count 50-70,000/µL: weigh risks and benefits
- If consistent with HELLP: consider verifying platelet count within 6 hours of the procedure.
- Unknown etiology
- Platelet count ≥70,000/µL: likely safe to proceed
- Platelet count <70,000/µL: additional workup may be beneficial
- For all patients
- Platelet count <50,000/µL: reasonable to avoid neuraxial
- If there is a concerning bleeding history, it is reasonable to avoid neuraxial or consult hematology beforehand.
- It is reasonable to avoid neuraxial in patients with current symptoms of disseminated intravascular coagulation or coagulopathy (bleeding from IVs, mucocutaneous bleeding, etc.)
- If there are no inherited or acquired coagulation defects, PT and aPTT are not useful in predicting bleeding risk in parturients with thrombocytopenia.
- There is not enough evidence to recommend the routine use of lab tests, including PT, aPTT, PFA-CT, TEG, and ROTEM, in parturients with thrombocytopenia to determine whether it is safe to place neuraxial blocks.
- Known etiology
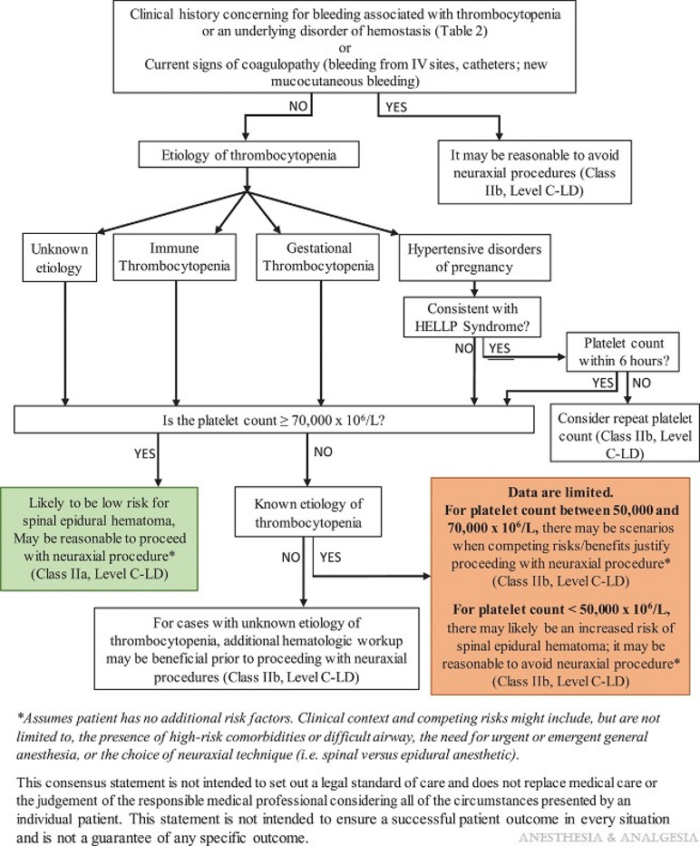
Figure 1. Decision aid for when to proceed with neuraxial procedures in obstetric patients with thrombocytopenia. LD = limited data. Used with permission from Bauer ME et al. The Society for Obstetric Anesthesia and Perinatology interdisciplinary consensus statement on neuraxial procedures in obstetric patients with thrombocytopenia. Anesth Analg. 2021;132(6):1531-44.4
References
- James AH, Jamison MG, Brancazio LR, et al. Venous thromboembolism during pregnancy and the postpartum period: incidence, risk factors, and mortality. Am J Obstet Gynecol. 2006;194(5):1311-5. PubMed
- Cines DB, Levine LD. Thrombocytopenia in pregnancy. Blood. 2017; 130 (21): 2271–7. PubMed
- Thornton P, Douglas J. Coagulation in pregnancy. Best Pract Res Clin Obstet Gynaecol. 2010;24(3):339-52. PubMed
- Bauer ME, Arendt K, Beilin Y, et al. The Society for Obstetric Anesthesia and Perinatology interdisciplinary consensus statement on neuraxial procedures in obstetric patients with thrombocytopenia. Anesth Analg. 2021;132(6):1531-44. PubMed
- Davies JR, Fernando R, Hallworth SP. Hemostatic function in healthy pregnant and preeclamptic women: an assessment using the platelet function analyzer (PFA-100) and thromboelastograph. Anesth Analg. 2007;104(2):416-20. PubMed
- Katz D, Bellin Y. Disorders of coagulation in pregnancy. Br J Anaesth. 2015;115:ii75-88. PubMed
- Yuan S, Ferrell C, Chandler WL. Comparing the prothrombin time INR versus the APTT to evaluate the coagulopathy of acute trauma. Thromb Res. 2007;120(1):29-37. PubMed
- Shreeve NE, Barry JA, Deutsch LR, Gomez K, Kadir RA. Changes in thromboelastography parameters in pregnancy, labor, and the immediate postpartum period. Int J Gynaecol Obstet. 2016;134(3):290-3. PubMed
- Katz D, Farber M, Getrajdman C, et al. The role of viscoelastic hemostatic assays for postpartum hemorrhage management and bedside intrapartum care. Am J Obstet Gynecol. 2024;230(3S): S1089-S1106. PubMed
- Leffert L, Butwick A, Carvalho B, et al. The Society for Obstetric Anesthesia and Perinatology consensus statement on the anesthetic management of pregnant and postpartum women receiving thromboprophylaxis or higher dose anticoagulants. Anesth Analg. 2018;126(3):928-44. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.