Copy link
Liver Chemistry and Function Tests
Last updated: 09/08/2025
Key Points
- The liver plays a central role in detoxifying various metabolites, synthesizing both proteins and digestive enzymes, regulating red blood cell turnover, and managing glucose synthesis and storage.
- Liver function tests (LFTs) commonly include measurements of serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), total bilirubin (including conjugated and unconjugated fractions), and albumin.
- Other tests include measuring the prothrombin time (PT) and calculating the international normalized ratio (INR).
- The liver's synthetic capacity can be evaluated by its production of albumin and vitamin K-dependent clotting factors (II, VII, IX, and X).
- Patterns of enzyme elevation can be used to identify the source of hepatic injury and guide differential diagnosis.
Introduction
- Liver function tests (LFTs) are used to evaluate the presence, severity, and progression of liver injury or dysfunction. They help identify underlying causes – alcohol-use disorder, metabolic-dysfunction associated steatohepatitis (MASH), viral hepatitis, cholestasis, or acute liver failure – and monitor subsequent disease progression.1
- In patients with cirrhosis or chronic liver disease, LFTs serve as useful indicators to guide diagnostic workup, risk stratification, and disease management. Some elements are also used in scoring tools to predict outcomes and determine the specific timing for interventions such as transjugular intrahepatic portosystemic shunt or liver transplantation.2
- The common laboratory tests used to assess liver function include:
- Transaminases (ALT and AST)
- ALP
- Gamma-glutamyl transferase (GGT)
- Serum albumin
- PT INR
- Serum bilirubin (total and direct/conjugated)
- Platelet count
Markers of Hepatocellular Injury and Cholestasis
- The “transaminases” are enzymes located within hepatocytes, the release of which indicates hepatocellular injury. ALT is found predominantly in the liver, while AST is also found in other tissues such as cardiac and skeletal muscle, kidney, and brain1 (Table 1).
- ALP exists as multiple isoforms across many different tissues. Liver ALP (LALP) is routinely measured as part of the evaluation of liver disease. Elevated levels are a sensitive marker of cholestatic liver injury, whether extrahepatic, such as bile duct obstruction, or intrahepatic, such as viral hepatitis, primary sclerosing cholangitis, and primary biliary sclerosis.
- GGT is another enzyme widely distributed across organ systems, but with a high concentration in the liver. Liver injury, especially that associated with alcoholic liver disease and cirrhosis, can cause an elevation in serum GGT levels, although a variety of nonhepatic conditions may have a similar effect.3
- Bilirubin is typically measured as total bilirubin and further divided into direct (conjugated) and indirect (unconjugated) fractions. Direct bilirubin has undergone conjugation in the liver, which makes it water-soluble and allows it to be excreted in bile. In contrast, indirect bilirubin arises from the breakdown of red blood cells, is lipid-soluble, and circulates in the bloodstream bound tightly to albumin.
- Elevated conjugated bilirubin levels indicate hepatocellular dysfunction or cholestasis (issues occurring after conjugation), whereas increased unconjugated bilirubin suggests excessive production, decreased hepatic uptake, or defective conjugation (problems occurring before conjugation).
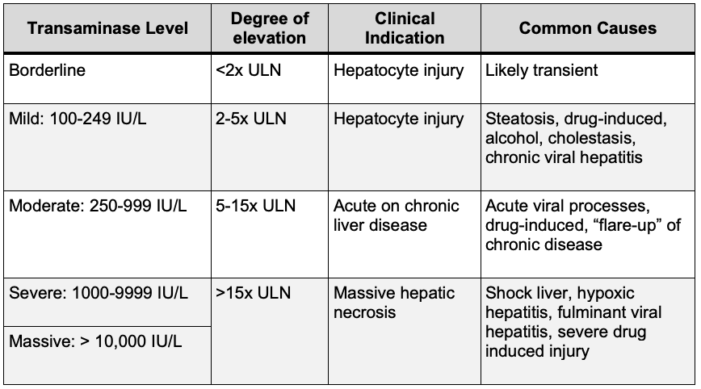
Table 1. Transaminase elevation patterns associated with potential causes.
Abbreviations: IU, international units; ULN, upper limit of normal
Markers of Synthetic Function
- The liver plays a central role in synthesizing plasma proteins and clotting factors.
- It produces the majority of coagulation factors, including fibrinogen (I), prothrombin (II), factors V, VII, IX, X, XI, and XII, along with the anticoagulation proteins C, S, and antithrombin. As a result, PT/INR serve as sensitive indicators of acute changes in liver function.1
- Prolongation of PT and an elevated INR indicate a decline in synthetic function because of the short circulatory half-lives of the key clotting factors (prothrombin II, factors VII and X).
- Albumin is a plasma protein synthesized exclusively in the liver. It has a long half-life in the circulation (~ 21 days), but levels can also vary with poor nutritional status, acute phase reactivity, and chronic health conditions (Table 2).
- Other plasma proteins, such as prealbumin and factor V, may have their levels assessed in specialized clinical contexts.
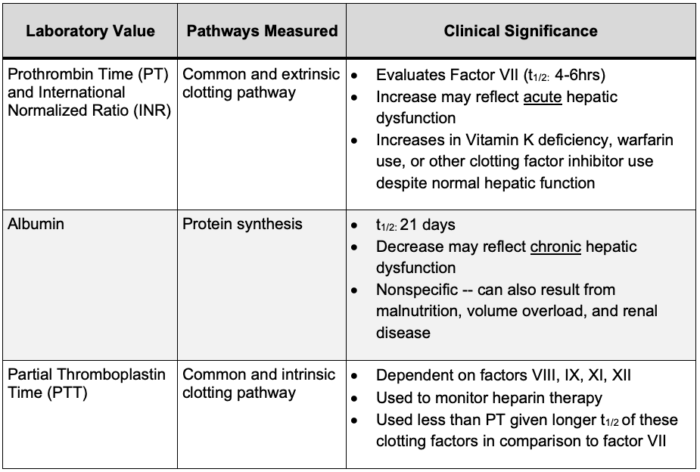
Table 2. Clinical significance of markers of hepatic synthetic function.
Abbreviations: t1/2, half-life
Scoring Systems
- Common scoring systems to assess liver disease include Child-Pugh, Model for End-Stage Liver Disease, FIB-4 Index, NAFLD fibrosis score, and albumin-bilirubin grade (ALBI).4
- Most systems use a combination of laboratory parameters, including but not limited to AST, ALT, platelet count, albumin, bilirubin, and PT/INR (Table 3).
- These noninvasive scoring systems are validated risk stratification tools for liver function, fibrosis state, and overall prognosis.5
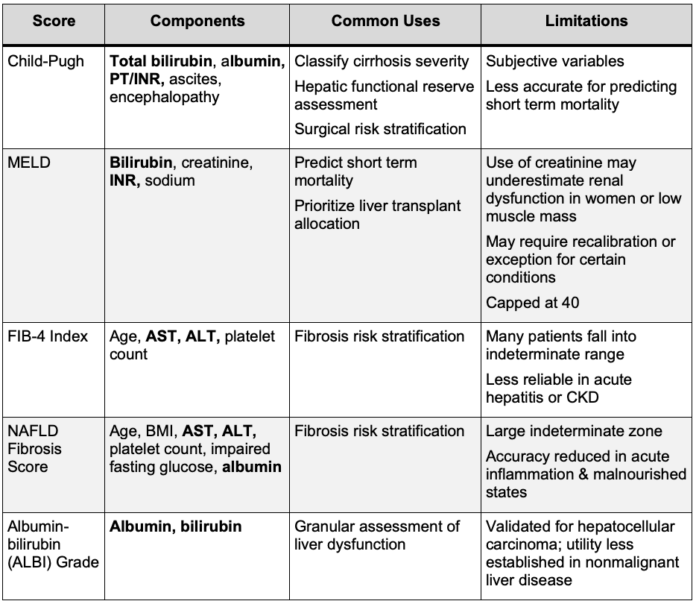
Table 3. Use of liver chemistry variables in liver disease-related scoring systems.
Abbreviations: PT, prothrombin time; INR, international normalized ratio; MELD, model for end-stage liver disease; FIB-4, fibrosis-4 index for liver fibrosis; AST, aspartate aminotransferase; ALT, alanine aminotransferase; CKD, chronic kidney disease; NAFLD, nonalcoholic fatty liver disease.
References
- Kwo PY, Cohen SM, Lim JK. ACG clinical guideline: Evaluation of abnormal liver chemistries. Am J Gastroenterol. 2017;112(1):18-35. PubMed
- Iluz-Freundlich D, Zhang M, Uhanova J, Minuk GY. The relative expression of hepatocellular and cholestatic liver enzymes in adult patients with liver disease. Ann Hepatol. 2020; 19(2):204-8. PubMed
- Irie M, Suzuki N, Sohda T, Anan A, et al. Hepatic expression of gamma-glutamyltranspeptidase in the human liver of patients with alcoholic liver disease. Hepatol Res. 2007;37(11):966-73. PubMed
- Moore O, Ma WS, Read S, et al. The unwell patient with advanced chronic liver disease: when to use each score? BMC Med. 2025;23(1):413. PubMed
- Sterling RK, Patel K, Duarte-Rojo A, et al. AASLD practice guideline on blood-based noninvasive liver disease assessment of hepatic fibrosis and steatosis. Hepatology. 2025;81(1):321-57. PubMed
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.