Copy link
Fibromyalgia
Last updated: 03/22/2023
Key Points
- Fibromyalgia is a chronic pain condition characterized by widespread pain and tenderness and is often associated with fatigue, sleep disturbance, mood and memory issues.
- Differential diagnosis includes hypothyroidism, polymyalgia rheumatica, rheumatoid arthritis, systemic lupus erythematosus and Sjogren’s syndrome
- Diagnostic criteria that is widely utilized includes widespread pain index, symptom severity score, presence of pain in at least 4 out of 5 regions of the body, and symptoms for at least 3 months.
Introduction
- Fibromyalgia is a relatively new term established in the mid 1970s by Smythe and Moldofsky to reflect a pain condition characterized by chronic widespread pain without evidence of inflammation of the connective tissues.1
- Fibromyalgia is characterized by2
- widespread pain and tenderness;
- fatigue;
- sleep disturbance; and
- mood and memory issues.
- The characteristics of pain found in fibromyalgia include
- diffuse or multifocal;
- difficult to localize;
- often waxes and wanes; and
- frequently migratory in nature.
- Fibromyalgia affects about 4 million US adults, about 2% of the adult population.2
- Risk factors for fibromyalgia include2
- sex: women are twice as likely to be diagnosed as men;
- stressful or traumatic events (car accidents, posttraumatic stress disorder);
- other painful conditions-osteoarthritis, rheumatoid arthritis, etc.;
- repetitive injuries;
- viral infections such as Epstein-Barr virus, viral hepatitis, etc.);
- family history of chronic pain; and
- obesity.
Diagnosis
- Previously, the diagnosis of fibromyalgia emphasized the number of tender points and widespread pain. In 2010, the American College of Rheumatology (ACR) developed provisional criteria, and in 2016, updated their diagnostic criteria. They abandoned the tender point count and instead, placed greater emphasis on the patient’s symptoms.1,3
- A thorough musculoskeletal examination and history remains the most important method of diagnosis for fibromyalgia. No diagnostic tests has been as reliable and does not account for the symptoms.
ACR Criteria for Fibromyalgia Diagnosis1
A patient satisfies modified 2016 fibromyalgia criteria if the following conditions are met.1
- Widespread pain index (WPI) is > 7 and symptom severity scale (SSS) score > 5 OR
WPI of 4–6 and SSS score > 9. - Generalized pain, defined as pain in at least 4 of 5 regions, must be present. Jaw, chest, and abdominal pain are not included in generalized pain definition.
- Symptoms have been present at a similar level for at least 3 months.
- A diagnosis of fibromyalgia is valid irrespective of other diagnoses. A diagnosis of fibromyalgia does not exclude the presence of other clinically important illnesses.
Widespread Pain Index
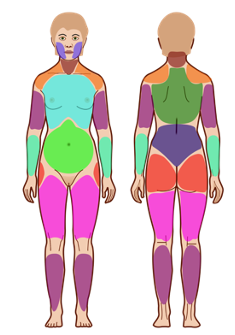
Figure 1. Widespread pain index: The patient is asked to note the number of areas in which the patient has had pain over the last week. Score will be between 0 and 19. Source: Wikimedia. Jmarchn, CC BY SA 3.0. Link. Accessed 12/05/22.
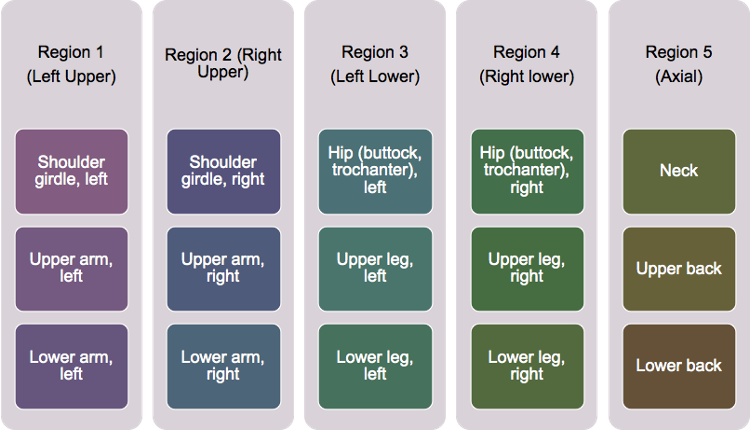
Figure 2. Regions of the body for WPI
Symptom Severity Scale (SSS) Score
- Fatigue
- Waking unrefreshed
- Cognitive symptoms
For each of the 3 symptoms above, indicate the level of severity over the past week
using the following scale:
0 = No problem
1 = Slight or mild problems, generally mild or intermittent
2 = Moderate, considerable problems, often present and/or at a moderate level
3 = Severe: pervasive, continuous, life-disturbing problems
The symptom severity scale (SSS) score is between 0 and 12 and is the sum of the severity scores of the 3 symptoms (fatigue, waking unrefreshed, and cognitive symptoms) (0–9) plus the sum (0–3) of the number of the following symptoms the patient has been bothered by that occurred during the previous 6 months:
- headaches (0–1);
- pain or cramps in lower abdomen (0–1); and
- depression (0–1).
The fibromyalgia severity scale is the sum of the WPI and SSS.
Differential Diagnosis
- Symptoms of fibromyalgia are similar to symptoms in the following conditions:
- Common
- Hypothyroidism
- Polymyalgia rheumatic
- Early in course of autoimmune disorders such as rheumatoid arthritis or systemic lupus erythematosus.
- Less common
- Hepatitis C
- Sleep apnea
- Chiari malformation
- Celiac sprue
- Drug-induced myalgias (e.g., lipid-lowering drugs)
- Laboratory tests are not useful for diagnosis of fibromyalgia except for the purpose of differential diagnosis and exclusion.
- Generally, the length of time can serve as a tool to assess for whether work up would be helpful as acute or subacute symptoms would require other conditions to be ruled out whereas symptoms that have persisted for many years are more likely to be due to fibromyalgia.
Treatment
Management of fibromyalgia follows a functional, multidisciplinary approach that is advocated for chronic pain management, with a focus on:
- improving function;
- improving quality of life; and
- managing symptoms.
Achieving these goals requires a personalized and multimodal plan that encompasses all aspects of a patient’s life (Figure 3). Diagnosis and treatment can be delivered in a primary care setting with referral to a specialty pain clinic reserved for: 1) those with uncertain diagnosis; 2) patients refractory to therapy and/or; 3) with significant comorbid psychiatric issues.4
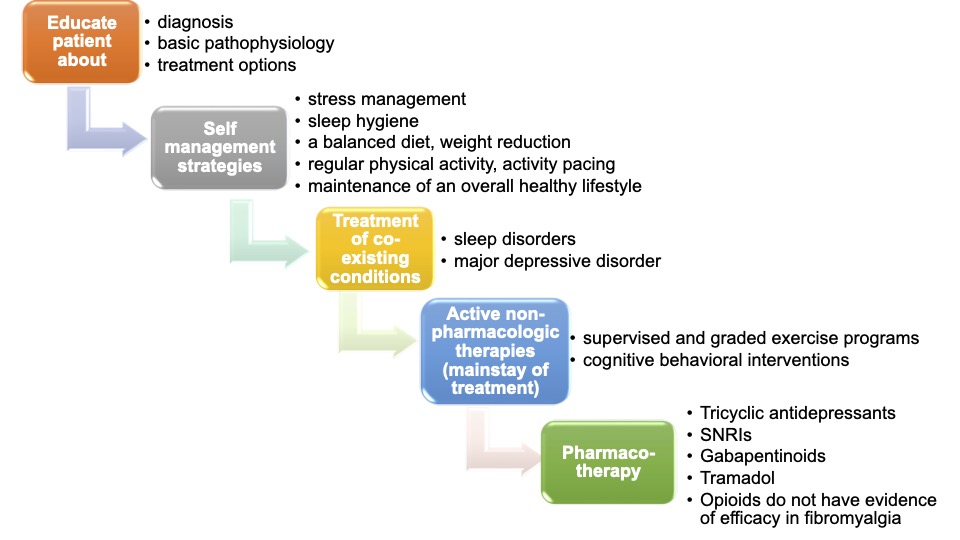
Figure 3. Management of fibromyalgia.5 (SNRI = serotonin and norepinephrine reuptake inhibitors).
References
- Wolfe F, Clauw DJ, Fitzcharles MA, et al. 2016 revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016;46(3): 319-29. PubMed
- Centers for Disease Control and Prevention (CDC). Fibromyalgia. Link. January 6, 2020. Accessed November 30, 2022.
- Clauw DJ, Brummett C. Fibromyalgia. In: Fishman S, Ballantyne J, Rathmell J. Bonica’s Management of Pain. 5th edition. Philadelphia, PA. Lippincott Williams & Wilkins. 2019; 535-43.
- Clauw DJ. Fibromyalgia: a clinical review. JAMA. 2014;311(15): 1547-55. PubMed
- Bair MJ, Krebs EE. Fibromyalgia. Ann Intern Med. 2020;172(5): ITC33-48. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.