Copy link
Delayed Emergence After Anesthesia
Last updated: 03/22/2023
Key Points
- Delayed emergence can be broken down into three potential causes: drug effects, metabolic abnormalities, and neurologic causes.
- Recognition and differential diagnosis utilizing clinical, laboratory, and radiographic assessments are key to patient safety.
- Appropriate management includes reversal of underlying cause(s), supportive management with continued mechanical ventilation, and appropriate postoperative care.
Identification and Evaluation
- Emergence from anesthesia should occur within 60-90 minutes, even after a long anesthetic. If the patient lacks an appropriate response to a stimulus within this time frame, this would be deemed delayed emergence from anesthesia.
- The major causes of delayed emergence from anesthesia are due to drug, metabolic or neurologic effects. Drug effects are the most common cause of delayed emergence. Supportive care and continued mechanical ventilation until full recovery is required.1
- Initial recognition and intraoperative work-up and evaluation will be discussed in further detail below but should include the following in a step-based manner:
- Vital signs including temperature, neurological exam (including pupillary response, gag and cough reflexes, motor/neuromuscular train-of-four (TOF) monitor, processed electroencephalogram (EEG) monitor, etc. should be evaluated.
- Clinicians should ensure that drugs are turned off and “reversed” when needed. This includes turning off anesthetic vapors. Infusions like propofol, ketamine, or dexmedetomidine should be stopped at an appropriate time at the end of case. appropriate reversal of Neuromuscular blockade should be appropriately reversed and ; the reversal of opiates and benzodiazepines should be considered.
- “Outside drugs” that patients may have been consuming and may influence their mental status like alcohol, recreational drugs, or prescription medications should be considered.
- Clinicians should evaluate labs including glucose, arterial blood gas (ABG) to evaluate for acid-base status, and electrolytes (sodium, calcium, magnesium, etc.). Once the drug and metabolic causes of delayed emergence are ruled out and reversed, extended workup and treatment to evaluate for neurologic causes includes:
- supportive care, including mechanical ventilation without sedation;
- appropriate placement of the patient in the intensive care unit (ICU) or postanesthesia care unit with repeated short interval neurological evaluations, repeat labs to monitor abnormalities and to guide corrections; and
- neurology consultation and “Stroke Alert,” likely stat head computed tomography (CT) scan with contrast, and repeated CT scan in 6-8hrs.2
Drug Effects
- Residual anesthetics
- Volatile anesthetics: Clinicians should ensure that the agent is turned off and that end-tidal concentrations are zero.
- Intravenous (IV) anesthetics
- Clinicians should ensure all IV infusions have been stopped.
- See Table 1 for context-sensitive half-lives and reversal of common anesthetics.
- Propofol: Delayed emergence is relatively common after prolonged administration. Extremely rare hepatic enzyme mutations have been reported in in cases of delayed emergence.3
- Reversal agents
- Naloxone is used for reversal of opiates. Intravenous boluses of 40 mcg should be administered every 2 minutes. After 400mcg, other reasons for delayed emergence should be considered. Readministration of naloxone may be needed as its effect is shorter than most long-acting opiates.
- Flumazenil is used for the reversal of benzodiazepines and barbiturates. 0.2mg IV boluses should be administered every 1 minute up to a maximum of 1mg. It may need readministration but do not exceed a total dose of 3mg/hr.
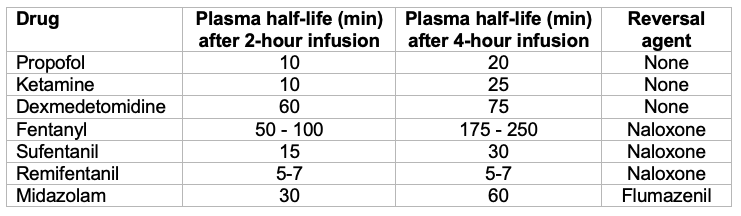
Table 1. Context-sensitive half-lives and reversal of common anesthetics
- Anticholinergics
- Although less likely, it is possible to have delayed emergence from cerebral anticholinergic syndrome, which can be potentiated by many drugs used in anesthesia, including opiates, benzodiazepines, phenothiazines, butyrophenones, ketamine, etomidate, propofol, nitrous oxide, halogenated inhalation anesthetics, scopolamine, and H2-blocking agents like cimetidine.4,5
- Physostigmine is used for reversal by administering 1.25-2 mg IV boluses and it may need readministration.4 Physostigmine is a lipophilic cholinesterase inhibitor, enabling it to penetrate the blood-brain barrier.
- Neuromuscular blockade
- Neuromuscular blocking agents at higher doses or after incomplete reversal may contribute to or mimic delayed emergence due to skeletal muscle weakness interfering with spontaneous breathing and movement.
- Sugammadex may be used if the patient received rocuronium or vecuronium for rapid reversal of neuromuscular blockade. For other nondepolarizing neuromuscular blockade agents, appropriate reversal with either edrophonium and atropine or neostigmine and glycopyrrolate should be administered.
- Finally, if the patient received a short-acting depolarizing agent (succinylcholine) and has not recovered, pseudocholinesterase deficiency should be considered.
- Drug-Drug interactions
- Multimodal anesthesia and pain management may lead to more sedation than anticipated.
- Gabapentin has been implicated in drug-drug interactions with ketamine leading to delayed emergence and possibly other anesthestics.5
- Home medications and recreational drugs
- The possible use of “outside drugs” consumed by the patient should be considered.
- Alcohol, recreational drugs, and other home medications can have sedative or neurologic effects.
Metabolic Causes
- Hypothermia/hyperthermia
- Clinicians should use core temperature monitoring to identify hypothermia or hyperthermia and correct it with active warming or cooling techniques to achieve normothermia.
- Acidosis, hypercarbia, hypoxemia
- Clinicians should use ABG to monitor acid-base status (pH, paCO2, paO2) and correct if derangements from normal ranges are present.
- “CO2 narcosis,” or somnolence from hypercapnia, can be seen when PaCO2 exceeds 60-70 mmHg. Hypercarbia can result from reduced elimination (e.g., respiratory failure, bronchospasm, opioid intoxication, etc.) and increased production (e.g., hypermetabolic states, malignant hyperthermia, etc.).
- Hyperglycemia or hypoglycemia
- Point-of-care finger stick glucose testing or ABG may be used to evaluate glucose levels and corrected with insulin for hyperglycemia or given glucagon or 50% dextrose for hypoglycemia as indicated.
- Electrolyte abnormalities (hyponatremia, hypercalcemia, hypermagnesemia)
- Electrolyte abnormalities with ABG or electrolyte panel should be identified as the above abnormalities can negatively impact arousal. Electrolyte disturbances should be corrected as indicated.
- Serotonin syndrome
- Rare cause of delayed emergence5
- Clinical diagnosis but mild symptoms may be difficult to differentiate from common postoperative symptoms such as tachycardia, restlessness, anxiety, dilated pupils, myoclonus. Severe cases have symptoms that closely resemble malignant hyperthermia with muscle rigidity, hyperthermia, tachycardia, and multiorgan failure.
- Many herbal medicines can cause increased serotonin levels.
- Underlying disease states (liver disease, thyroid disease, renal failure, etc.)
- Patients with pre-existing liver or thyroid disease in extreme states may have difficulty with the metabolism of medications given in the perioperative period. Supportive management is indicated until further lab testing is performed. Liver function tests (LFT), thyroid function tests (TFT), calculation of glomerular filtration rate, etc. should be considered.
Neurologic Causes
- Once drug and metabolic events are ruled out, the following neurologic events should be considered as they can cause a change in mental status and present as delayed emergence.
- New ischemic, thrombotic, embolic, or hemorrhagic event
- Seizures and postictal state
- Increased intracranial pressure (ICP)
- Rare causes: psychiatric disorders including conversion disorder and sleep disorders including narcolepsy and sleep paralysis5
- Neurology and possibly neurosurgery should be consulted. A stroke alert may be called and head imaging such as CT scan or CT angiogram with a follow-up scan as appropriate in 4-6 hours may be ordered.
- Patients after neurosurgical procedures are especially at risk for intracranial hemorrhage, ischemia, seizures, and increased ICP. These patients should undergo a STAT CT head prior to a neurology consult.
- It is important to keep in mind that the patient may need to return to the operating room (OR) if an acute neurosurgical problem is identified.
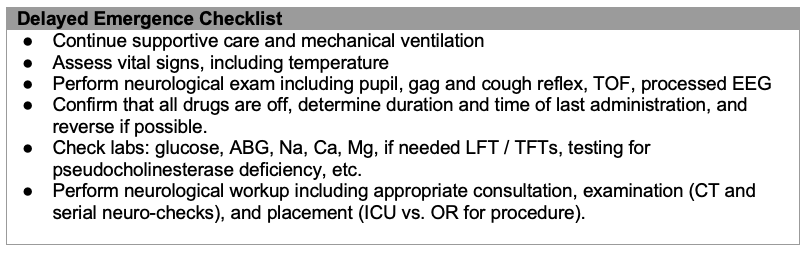
Table 2. Delayed emergence checklist.
References
- Berg SM, Braehler MR. The Postanesthesia Care Unit. In: Gropper MA, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Cohen NH, Leslie K, ed. Miller’s Anesthesia; Ninth Edition; Philadelphia, PA. Elsevier; 2020: 2586-2613.
- Stanford Ether. Delayed Emergence from Anesthesia. Link. Published 2022. Accessed 08/01/2022.
- Yonekura H, Murayama N, Yamazaki H, et al. A case of delayed emergence after propofol anesthesia: Genetic analysis. AA Case Rep. 2016; 7 (11):243-6. PubMed
- Schneck HJ, Rupreht J. Central anticholinergic syndrome (CAS) in anesthesia and intensive care. Acta Anaesthesiol Belg. 1989; 40(3): 219-28. PubMed
- Tzabbazis A, Miller C, Dobrow MF, et al. Delayed emergence after anesthesia. J Clin Anesth. 2015;27(4):353-60. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.