Copy link
Cervical Spine Injuries
Last updated: 08/09/2023
Key Points
- Among cervical spine injuries (CSI), ligamentous injury is more likely to be associated with spinal instability than bony fracture injuries.
- Cervical spine clearance can be radiological or clinical. Up to one-third of patients with delayed diagnosis of CSI may develop neurological deficits.
- There is no single best airway management technique in patients with CSI. The goal is to minimize neck movement and the risk of potential spinal cord injury during intubation.
- Anesthetic considerations include achieving neuroprotection through proper positioning and neurophysiological monitoring, management of autonomic instabilities, maintaining adequate spinal cord perfusion, and appropriate postoperative care in the intensive care unit (ICU).
Introduction
- The incidence of CSI is about 2% of patients with blunt trauma. This incidence is increased if the Glasgow Coma Scale (GCS) score is less than 8 or if there is a focal neurologic deficit.1
- Immobilization of the cervical spine with suspected injury is the standard of care and may pose challenges to airway management.2
Cervical Spine Anatomy
- The cervical spine is composed of seven vertebrae. The first (atlas) and second (axis) cervical vertebrae support the weight of the occiput and form the atlanto-occipital and atlanto-axial joints.
- The ligaments of the cervical spine are commonly divided into two columns (Figure 1).3
- Posterior column includes the supraspinous ligament, interspinous ligament, and ligamentum flavum. They provide stability during flexion.
- Anterior column includes the anterior and posterior longitudinal ligaments, and three ligaments that secure the dens (odontoid process) of C2 to the anterior arch of C1. The posterior column provides stability during extension.
- When the first cervical spine is viewed in the sagittal plane, note that anterior one-third of the space is occupied by the dens, the middle third is the spinal cord, and the posterior third is the buffer to allow encroachment of the spinal lumen without cord compression. (Figure 1C). The spinal cord occupies a greater proportion of the space in the subaxial spine. At C6, approximately 75% of the space is occupied by the cord.
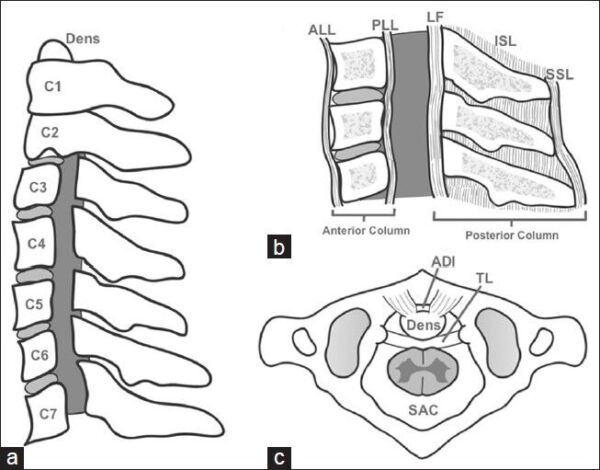
Figure 1. Cervical spine anatomy: a. lateral view of the cervical spine; b. ligaments forming the anterior and posterior columns; c. superior view of first on second cervical vertebrae. The transverse ligament (TL) limits translation and the normal atlas-dens interval (ADI) of 3 mm. ALL = anterior longitudinal ligament; PLL = posterior longitudinal ligament; LF = ligamentum flavum; ISL= interspinous ligament; SSL = supraspinous ligament. Source: Austin N, et al. Int J Crit Illn Inj Sci. 2014;4(1):50-6. CC BY NC SA 3.0. PubMed.
Injury Classification
- Fracture injuries are generally considered to be clinically insignificant unless also associated with ligamentous injury that results in instability or with displaced fracture elements causing neurovascular injury and compromise.1
- Ligamentous injury is less likely to occur with pure flexion injuries, which typically do not result in spinal instability.1
- In general, hyperflexion injuries involve distraction or overstretching of the posterior column, and hyperextension injuries involve distraction of the anterior column3 (Figure 2).
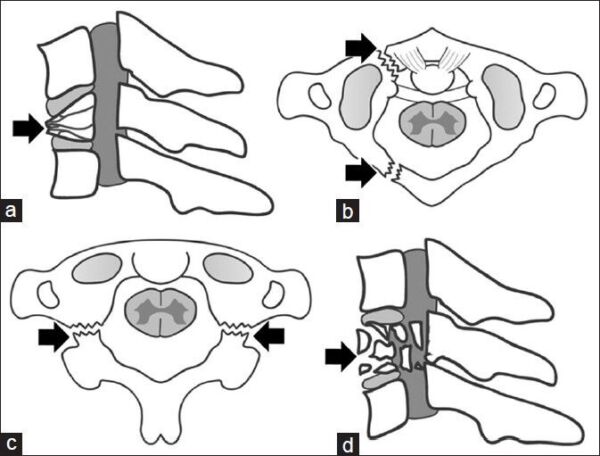
Figure 2. Types of CSI: a. hyperflexion leading to a vertebral body wedge fracture, b. hyperflexion leading to a “Jefferson” fracture of C1 anterior and posterior arches, c. hyperflexion leading to a Hangman’s fracture of C2 pedicles, and d. compression injuries leading to a verterbral body burst fractures. Source: Austin N, et al. Int J Crit Illn Inj Sci. 2014;4(1):50-6. CC BY NC SA 3.0. PubMed.
- High CSI (occiput to C2) are typically classified by the anatomical level.4
- Occiput: occipito-atlantal dissociation
- This type of injury is typically fatal.
- C1: Jefferson burst fracture due to axial compression
- Dens: Odontoid fractures4 (Figure 3)
- Type I: Mostly considered stable and involves the apex of the dens
- Type II: Considered unstable – fracture of the dens through the base
- Type III: Considered unstable – fracture into the C2 vertebral body
- C2: Hangman’s fracture – disruption of the anterior longitudinal ligament as well as a fracture through the C2 pars interarticularis. This combination results in the anterolisthesis of the vertebral body.4
- Lower CSI (C3 and below) are typically classified by the mechanism of injury.4
- Distractive flexion results in posterior ligament tear, unilateral or bilateral facet dislocation.
- Compressive flexion results in anterior vertebral body fracture, wedge compression fracture.
- Distractive extension results in anterior ligament tear, hyperextension sprain or dislocation.
- Compressive extension results in posterior element fractures such as unilateral or bilateral laminar fractures, lateral mass fractures, or spinous process fractures.
- Axial compression: results in vertebral body burst fracture.
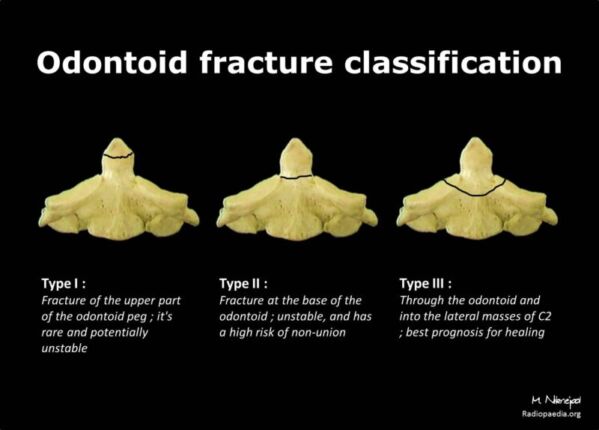
Figure 3. Odontoid fracture classification. Case courtesy of Mohammadtaghi Niknejad. Radiopaedia.org, rID:21310. Link.
Cervical Spine Injury Assessment and Management
- The initial evaluation is geared towards determining the presence of potentially unstable CSI, which is usually based on a radiographic evaluation.
- The National Emergency X-radiography Utilization Study (NEXUS) criteria must be met for clinical cervical spine clearance without radiographic assessment.5
- Patient is alert, oriented, and has a GCS of 15
- Absence of distracting injuries
- No evidence of interference of mental status, such as usage of intoxicants or illicit substances
- No pain or tenderness of the cervical spine
- Full range of active motion without symptoms
- No neurological deficits related to the cervical spine
- To clear a cervical collar (C-collar) in obtunded patients, the Eastern Association for the Surgery of Trauma (EAST) guidelines can be used for removal of the C-collar after a high-quality negative computed tomography (CT) of the cervical spine.6
- For radiographic clearance, CT is the preferred initial screening tool with magnetic resonance imaging (MRI) as the diagnostic tool for ligamentous injuries. Plain radiographs may be helpful in ruling in CSI but may miss up to 15% of injuries, Therefore, it cannot be relied upon to rule out CSI.1
- Up to one-third of patients with delayed diagnosis of injury may develop long-term neurological deficits.1
- Without clearance of the cervical spine, or when there is evidence of an unstable injury, immobilization of the neck is standard practice until treatment can be determined.2
- Initial immobilization typically involves the use of sandbags and headstraps while the patient is supine on bedrest and/or using a hard C-collar (Figure 4).
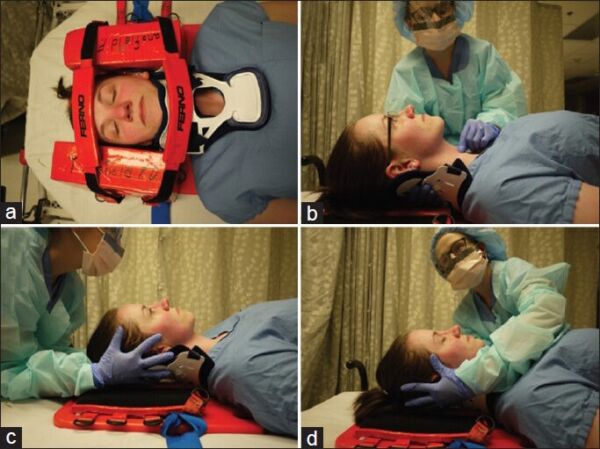
Figure 4. Neck stabilization for CSI. (a) neck stabilization using sandbag collar-tape on hardboard for prehospital care, (b) cricoid pressure with the anterior half of hard cervical collar (C-collar) removed and other hand behind posterior C-collar, (c) manual in-line immobilization (MILI) from head of the bed, with anterior C-collar removed and hands cradling the occiput and mastoid process, and (d) MILI from side of the bed to facilitated airway management. Source: Austin N, et al. Int J Crit Illn Inj Sci. 2014;4(1):50-6. CC BY NC SA 3.0. PubMed.
Airway Management
Emergent Airway Management Considerations
- Trauma patients are often considered to be full stomach, and a rapid sequence induction (RSI) should be considered to minimize the risk of aspiration.
- CSI may occur concurrently with laryngeal penetration injuries that cause aspiration even prior to intubation.7
- Direct laryngoscopy may be performed more efficiently but may also result in more movement of the spine than indirect visualization techniques.
- Indirect visualization techniques such as video laryngoscopy, fiberoptic visualization, blind nasal intubation or use of an intubating laryngeal mask airway may better allow the neck to remain in a neutral position in comparison to direct laryngoscopy.
- Video laryngoscopy is an excellent alternative to direct visualizations techniques, especially for patients who are anticipated to have less an optimal airway view.
- Awake fiberoptic intubation allows for neurological exam before and after intubation to ensure minimal damage to spinal cord. However, patient selection is key and requires high level of patient cooperation, provider experience, and availability of local anesthetics (lidocaine jelly, lidocaine spray, etc.)
- Patients may have other concurrent injuries that pose challenges to securing the airway. For example, nasal intubations are relatively contraindicated in the presence of concurrent skull-base injuries.7
- Supraglottic airways are an essential piece of equipment to have readily available during emergency airway situations as it is part of the typical difficult airway algorithm. However, they have been shown to cause posterior displacement at upper cervical levels.3
- There is no singular “best” method for tracheal intubation. Selection of the optimal technique and outcome depends on the pattern of injury, resource availability, and provider experience.
Nonemergent Airway Management Considerations
- If the surgical intervention is not urgent or emergent, the benefit of waiting for the patient to be appropriately nil per os (NPO) should be considered.
- This allows further time to carefully examine the patient’s airway and plan for the most appropriate method of intubation and gathering of the appropriate supplies and equipment for intubation.
- Manual in-line immobilization (MILI) should be used to stabilize the cervical spine during intubation (Figure 4).
- MILI has less impact on obscuring the view for direct laryngoscopy when compared to other stabilization techniques such as axial-traction or C-collar.1
- As nonemergent airways likely do not require RSI and will allow for mask ventilation, anesthesia providers must keep in mind that even masking or jaw thrusting can further exacerbate spine instability. The required immobility may cause mask ventilation to be harder than usual.
Anesthetic Considerations
Preoperative Evaluation
- History: Due to the nature of CSI, it may not be possible to interview the patient or to ascertain the time span from injury and NPO time. A collateral history can be obtained from the emergency medical technicians or the patient‘s family.
- Airway considerations:
- In patients with injury at the C3-5 level or above, respiratory insufficiency may require preoperative intubation and ventilatory support8
- CSI can often disrupt diaphragmatic and other accessory respiratory muscular function, predisposing these patients to atelectasis and retention of secretions.
- Hemodynamic considerations:
- Mean arterial pressure (MAP) should be maintained above 85-90 mmHg to optimize spinal cord perfusion.9
- Spinal shock is typically not diagnosed in the immediate postinjury timeline and it usually occurs about 24-48 hours after the initial injury.
- Neuroprotection:
- Immobilization is commonly used to help stabilize the cervical spine and prevent further injury secondary to airway management, positioning, etc.
- Steroids: Although previously a standard to give methylprednisolone within 8 hours of injury, the more recent guidelines10 did not include recommendations for steroid usage. If surgeon requests the administration of high dose of steroids, consider potential adverse effects such as hyperglycemia, immunosuppression, and gastrointestinal bleeding.
- Hypothermia: Mild to low hypothermia can be beneficial for neuroprotection without the complications of deep hypothermia such as coagulopathy, hemodynamic instability, and immunosuppression.9
Intraoperative Considerations and Monitoring
- Induction: It is critical to optimize spinal cord perfusion pressure and avoid systemic hypotension or increases in intracranial pressure. Hence, large doses of propofol or ketamine should be avoided.
- Depolarizing muscle relaxants: starting a few days following injury, depolarizing agents such as succinylcholine should be avoided to prevent hyperkalemia.
- The intense stimulation while inserting an airway device may cause severe bradycardia from autonomic instability secondary to spinal cord injury, leading to hemodynamic instability and even cardiac arrest.
- Intraoperative neurophysiological monitoring (IONM):
- Several intraoperative factors may worsen patient injury, such as positioning, surgical-related factors, hypotension, hypothermia. IONM can help guide clinicians to minimize further damage to the spinal cord.
- Somatosensory evoked potentials are commonly used and total intravenous anesthesia (TIVA) or a combination of intravenous anesthesia with less than 1 minimum anesthetic concentration of volatile agents are preferred for this type of monitoring. Muscle relaxants can be used.
- Motor evoked potentials: TIVA without muscle relaxants are preferred to aid monitoring.
- Maintenance of anesthesia:
- Ventilation: Normocapnia should be maintained and hyperventilation should be avoided as it reduces spinal cord perfusion.8
- Hyperglycemia is associated with poor neurologic outcomes and should be avoided. Blood glucose level should be checked frequently and levels above 200 mg/dl must be treated aggressively.8
- Hemodynamics: Placement of an arterial line should be considered since many patients experience hemodynamic instability secondary to the autonomic imbalance.
- Bradycardia can be induced by activities that increase vagal tone, such as suctioning or intubation. Therefore, atropine should be readily available.
- Hypotension may occur secondary to hemorrhagic and neurogenic shock, depending on the patient’s pattern and severity of injury.
- MAP should be maintained within 85-90 mmHg with systolic blood pressures above 90 mmHg during the first 7 days postinjury to optimize spinal cord perfusion.8
- Resuscitation: excessive crystalloid fluid may result in heart failure, electrolyte abnormalities, coagulopathy, and edema. Goal-directed fluid resuscitation is recommended. Hemodynamic goals should be maintained with vasopressors and a balanced ratio of blood products should be used to avoid dilutional coagulopathy.
- Postoperative care
- These patients should be managed in the ICU to allow close neurological, hemodynamic, and respiratory monitoring.
- Extubation considerations:
- Several factors such as the extent of injury, patient comorbidities, length and extent of surgery, amount of resuscitation, respiratory status and ease of initial intubation should be considered.
- Additionally, respiratory failure may recur the first 7-10 days of injury.10
- Thromboembolic prophylaxis: this patient population is at high risk for thromboembolic events.
- Prophylaxis is recommended for 3 months. A combination of chemical prophylaxis (low-molecular weight heparin) and mechanical prophylaxis (compression stockings) should be considered.8
References
- Crosby ET. Airway management in adults after cervical spine trauma. Anesthesiology. 2006;104(6):1293–318. PubMed
- Gupta AK, Gelb AW. Airway management and cervical spine disease. In: Essentials of neuroanesthesia and neurointensive care. Philadelphia, PA: Saunders Elsevier.160–5.
- Austin N, Krishnamoorthy V, Dagal A. Airway management in cervical spine injury. Int J Crit Illn Inj Sci. 2014;4(1):50-6. PubMed
- Cervical Spine Radiology. In: Schwartz DT. eds. Emergency Radiology: Case Studies. McGraw Hill; 2008.
- Hoffman JR, Wolfson AB, Todd K, et al. Selective cervical spine radiography in blunt trauma: Methodology of the national emergency X-radiography utilization study (nexus). Ann Emerg Med. 1998;32(4):461–9. PubMed
- Patel MB, Humble SS, Cullinane DC, et al. Cervical spine collar clearance in the obtunded adult blunt trauma patient. J Trauma Acute Care Surg. 2015; 78(2):430–41. PubMed
- Bao FP, Zhang HG, Zhu SM. Anesthetic considerations for patients with acute cervical spinal cord injury. Neural Regen Res. 2017;12(3):499-504. PubMed
- Hadley MN, Walters BC. Introduction to the guidelines for the management of acute cervical spine and spinal cord injuries. Neurosurgery. 2013;72 Suppl 2:5-16. PubMed
- Ryken TC, Hurlbert RJ, Hadley MN, et al. The acute cardiopulmonary management of patients with cervical spinal cord injuries. Neurosurgery. 2013;72.Suppl 2:84-92. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.