Copy link
Bronchial Blockers for One-Lung Ventilation
Last updated: 05/10/2023
Key Points
- Bronchial blockers (BB) achieve lung separation via balloon occlusion of a mainstem bronchus to allow lung collapse distal to the occlusion.1 Positioning a BB in a more distal airway can also be used to achieve selective lobar collapse.2
- Bronchial blockers achieve similar quality of lung collapse to double-lumen tubes but are more likely to dislodge during surgery and may require repositioning.
- Specific use cases of BB include:
1. A patient with a difficult airway who needs an awake orotracheal or nasotracheal intubation and one-lung ventilation (OLV).
2. A patient with an existing endotracheal tube or tracheostomy tube who requires OLV.
3. A patient who requires OLV during surgery and is anticipated to require postoperative mechanical ventilation. - The BBs require the use of flexible fiberoptic bronchoscopy to guide the blocker and achieve optimal position.
Description and Indications
BBs are used as a technique for lung separation and offer comparable quality of lung collapse compared to double-lumen tubes. Indications for lung separation include:
- To facilitate surgical exposure
- To prevent contamination of the contralateral lung in case of pulmonary hemorrhage
- To apply differential lung ventilation
A BB consists of a shaft with an inflatable balloon at the tip. BBs are designed to be introduced through the lumen a single-lumen endotracheal tube (ETT) or tracheostomy tube, or less commonly, passed extraluminally alongside an in situ endotracheal or tracheostomy tube. Positioning and inflating the balloon within a specific airway allows lung collapse distal to the occlusion to achieve lung or selective lobar blockade. In BBs designed for adult airways, the shaft includes a central channel through which suction, insufflation (e.g., with oxygen), or continuous positive airway pressure (CPAP) can be applied.
Techniques for Bronchial Blocker Placement and One Lung Ventilation
For ease of placement and bronchoscopic exam, it is recommended that the BB is introduced and initially positioned while the patient is in the supine position. Test inflation and deflation of the BB balloon should always be performed prior to use.
The overall technique for placing and positioning BBs consists of the following:
- Endotracheal intubation should established, taking care to select a tube size adequate to accommodate BB and bronchoscope (e.g., 7.5-8.0 mm internal diameter or larger in most adult cases). An in-situ endotracheal or tracheostomy tube of adequate size can also be used.
- The multiport adapter (included with the BB kit) should be attached to the single-lumen ETT and breathing circuit. The multiport adapter has dedicated ports for the bronchoscope and BB.
- A bronchoscopic exam should be performed to identify relevant tracheobronchial anatomy and to ensure there is adequate distance between the ETT tip and tracheal carina (3-4 cm)
- The BB should be introduced into the lumen of the ETT or tracheostomy tube and guided into position under bronchoscopic guidance. The BB balloon should be positioned approximately 5-10 mm below the carina for lung separation.
- Under bronchoscopic guidance, it should be ensured that the BB exits the distal opening of the ETT and not the Murphy eye.
- To facilitate left-sided BB placement, rotating the patient’s head toward the right can help displace the left mainstem bronchus towards the midline.
- BB positioning should be tested with balloon inflation to ensure that the BB does not dislodge from the selected bronchus. The BB balloon should be inflated with enough air to occlude the selected bronchus, approximately 5-8 mL for most adult sized BBs in a mainstem bronchus. The BB balloon should be deflated when lung separation is no longer needed.
- If patient repositioning is needed for surgery, the BB should be deflated until patient positioning is complete to avoid dislodgment of an inflated BB and resultant complete airway occlusion. When patient positioning is complete, BB position should be reconfirmed under bronchoscopic exam prior to BB inflation.
To achieve lung collapse and one-lung ventilation (OLV) after initial BB placement and patient positioning, the following steps are recommended:
- 100% oxygen should be administered.
- Appropriate BB position on bronchoscopic exam should be confirmed.
- Positive pressure ventilation should be stopped, the breathing circuit should be disconnected, and complete expiration should be allowed.
- BB balloon should be inflated under bronchoscopic visualization.
- Intermittent suction through the central channel should be initiated.
- Ventilation on the nonoperative side should be resumed.
Specific Bronchial Blocker Designs and Features
Variations on the basic BB design allow for improved manipulation and control. Commonly available BBs (Figure 1) include:
- Arndt® Wire-guided blocker (Cook Medical, Indiana, USA)
- Cohen® Tip Deflecting Endobronchial blocker (Cook Medical, Indiana, USA)
- Fuji Systems® Uniblocker (Ambu Inc, Maryland, USA)
- Rusch® EZ-Blocker® (Teleflex, North Carolina, USA)
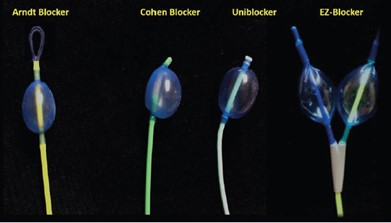
Figure 1. Commonly used BBs- Arndt blocker, Cohen blocker, Uniblocker, and EZ-Blocker. Used with permission from Campos JH.1
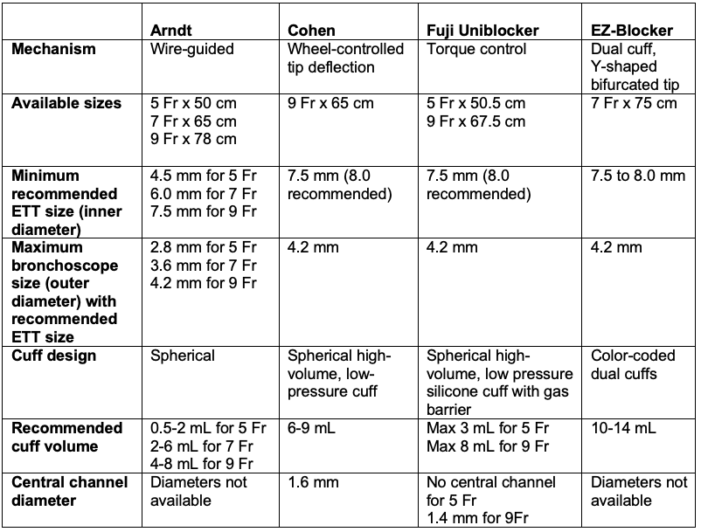
Table 1. Summary of the features of common BBs.
- The Arndt® blocker is a BB attached to a 7.0 or 9.0 Fr catheter. The Arndt® blocker has a high-volume, low-pressure cuff with a spherical shape balloon. These blockers contain a flexible nylon wire passing through the proximal end of the catheter extending to the distal end, which exists as a small flexible wire loop. This blocker comes with a multiport connector to accommodate the blocker and the fiberoptic bronchoscope. The wire loop of the Arndt® blocker is coupled with the fiberoptic bronchoscope and serves as a guide wire to introduce the blocker into the bronchus (Figure 2).
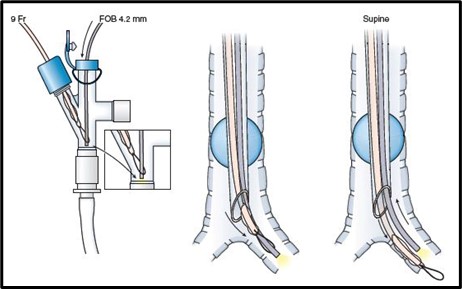
Figure 2. The placement of an Arndt® BB through a single-lumen endotracheal tube with the fiberoptic bronchoscope advanced through the guidewire loop into the left mainstem bronchus Used with permission from Campos JH.1
- For a 7 Fr Arndt blocker, a 7.5 mm internal diameter (ID) single-lumen ETT is used, and the larger 9 Fr Arndt blocker is best used with an 8.0 mm ID single-lumen ETT. After the optimal position of the Arndt blocker is accomplished, the wire-guide nylon loops must be removed. This blocker requires 4 to 8 mL of air in the cuff to achieve proper blockade. The optimal position for a right or left blocker is the one that allows one to see the outer balloon surface about 20 mm below the main bronchus (Figure 3).
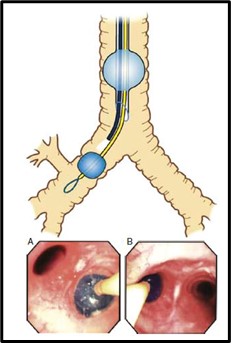
Figure 3. The optimal position of a BB in the right and left mainstem bronchus. The proximal edge of the fully inflated cuff is approximately 5 to 10 mm below the trachea carina. (a) A BB in the right mainstem bronchus, and (b) A BB in the left mainstem bronchus. Used with permission from Campos JH.3
- Cohen® Flexitip BB is available only in size 9.0 Fr. This device comes with a spherically shaped high-volume low-pressure balloon. The Cohen® blocker relies on a wheel-turning device located in the most proximal part of the unit allowing deflection of the flexible tip of the distal part of the blocker into the desired bronchus. Also, there is a torque grip located at the 55 cm mark to allow rotation of the blocker. The Cohen® blocker is advanced through an 8.0 mm ID single-lumen ETT; before insertion, the blocker balloon should be tested. This blocker, like all blockers, needs to be lubricated to facilitate insertion.
- The optimal position of this blocker when seen with the fiberoptic bronchoscope is the one that provides a view of the outer surface of the fully inflated balloon (4-8 mL of air) at least 10-20 mm below the tracheal carina into a mainstem bronchus (Figure 4).
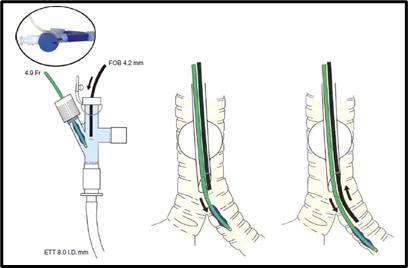
Figure 4. Displays the placement of a Cohen® Flexitip BB going into the left mainstem bronchus. Used with permission from Campos JH.3
- The Fuji Uniblocker® is a hockey stick-shaped tip BB and is available in 9.0 Fr size for adults. It has a high-volume balloon made of silicone with a maximal cuff inflation of 6 mL of air. The Fuji Uniblocker® is equipped with a swivel connector. The swivel connector allows easy insertion of the fiberoptic bronchoscope and continuous ventilation during blocker positioning. This blocker has a torque control with an incorporated shaft that allows guidance through the desired bronchus (Figure 5).
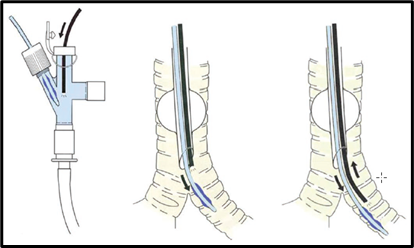
Figure 5. Placement of the Fuji Uniblocker.® Used with permission from Campos JH3
- The EZ Blocker is available in a 7.0 Fr size and is made of polyurethane material. The EZ blocker is designed with a y-shaped distal end. Both limbs of the distal end are fitted with an inflatable balloon and a central channel to allow suction. Also, each limb is color-coded (yellow or blue) for easy identification with the matching pilot balloon. The EZ blocker is inserted through a port of the enclosed multiport adapter that is attached to a single-lumen ETT. The optimal size of the single-lumen ETTT is 7.5- or 8.0-mm ID, so it allows the blocker and the fiberoptic bronchoscope to navigate together. The multiport adaptor of the EZ blocker is designed to be joined to the connector of the single-lumen ETT, and it contains two additional ports, one to allow advancement of the blocker and the other port for passing the flexible fiberoptic bronchoscope.
- The EZ blocker is tested and lubricated before passing into the lumen of the single-lumen ETT and the multiport connector. After advancing the blocker, the y-shaped end should be seated in the tracheal carina and each independent tip should be located in the entrance of the right and left bronchus. Only the balloon where lung isolation is desired should be inflated under direct fiberoptic bronchoscopy. The EZ blocker balloon sometimes requires up to 10-14 mL of air to achieve an adequate seal within the bronchus. The proper and optimal position is when the outer surface of the balloon is seen 5 to 10 mm below the entrance of the bronchus (Figure 6). The single-lumen ETT should be at least 4 cm above the carina for this BB to work.
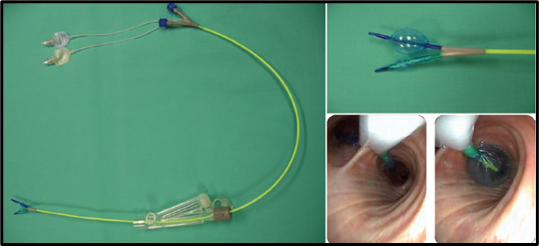
Figure 6. Displays the optimal position of the EZ-Blocker. (A) The EZ-Blocker and multiport adapter, (B) displays the Y-shaped distal end with one balloon fully inflated and the other deflated, (C) shows Y-shaped distal end sitting on the tracheal carina and to the right the balloon fully inflated. Used with permission from Campos JH.1
- The optimal position for a BB with the bronchoscope should be confirmed when the patient is in lateral decubitus position or wherever a malposition occurs.
Advantages and Disadvantages of the Bronchial Blocker4
Advantages of BBs
- There is easy recognition of anatomy if the tip of the single-lumen ETT is above the tracheal carina (4 cm).
- BB is the best device for patients with difficult airways.
- Cuff damage during intubation is rare.
- There is no need to replace an ETT if postoperative mechanical ventilation is needed.
- BBs can be used for early stage or long-term tracheostomized patients during OLV.5
Disadvantages of BBs
- They have a small channel for suctioning.
- Conversion from 1 to 2; then to 1 lung ventilation is problematic and more complex.
- BBs are high maintenance devices (frequent dislodgement or loss of seal during surgery).
- They require a learning curve to master the technique.
Complications with the Use of Bronchial Blockers
Although serious complications have been reported with the use of current BBs, these complications appear to be more benign than those involving double-lumen endotracheal tubes.
- Complications with the Arndt® blocker include a report of a sheared balloon that occurred when the blocker was removed through the multiport blocker site. It is recommended that when the Arndt® blocker is not in use, it needs to be removed with the multiport connector in place to prevent this complication (sheared material).
- Another complication of the Arndt® blocker involved inadvertent resection of the guide wire adapter of the tip of the BB during stapler resection.
- There is a recent report involving the Fuji Uniblocker® where the balloon of this blocker failed to deflate in three cases; therefore, the already inflated balloon had to be removed along with the single-lumen ETT during extubation. It is recommended to test the pilot and balloon prior to use to ensure that the air that is injected is aspirated and the balloon completely deflates.
- There are also case reports with the Fuji Uniblocker® and another involving the EZ blocker, where the tip of the blocker perforated the bronchial wall.
References
- Campos JH. Separation of the lung: Double-lumen endotracheal tubes and endobronchial blocker. In: Cohen E (ed). Cohen's Comprehensive Thoracic Anesthesia. 1st edition. Philadelphia, PA. Elsevier. 2022: 213-39.
- Campos JH. Lung isolation in patients with a difficult airway in thoracic anesthesia. In: Cohen E (ed). Cohen's Comprehensive Thoracic Anesthesia. 1st edition. Philadelphia, PA. Elsevier. 2022: 240-8.
- Campos J. Lung isolation. In: Slinger P (ed). Principles and Practice of Anesthesia for Thoracic Surgery. 2nd edition. Switzerland. Springer Nature. 2019: 283-309.
- Campos JH. Which device should be considered the best for lung isolation: Double-lumen endotracheal tube versus bronchial blockers. Curr Opin Anaesthesiol. 2007; 20:27-31. PubMed
- Campos JH, Musselman ED, Hanada S, Ueda K. Lung isolation techniques in patients with early stage or long-term tracheostomy: A case series report of 70 cases and recommendations. J Cardiothorac Vasc Anesth. 2019; 33: 433-9. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.