Copy link
Ketogenic Dietary Therapy
Last updated: 01/12/2023
Key Points
- Ketogenic diets are high-fat, low carbohydrate diets that induce and maintain ketosis and are well-established treatment modalities for patients with drug-resistant epilepsy.
- Maintenance of ketosis throughout the perioperative period is critical.
- Major anesthetic considerations include a comprehensive preoperative evaluation, avoiding medications and intravenous fluids with high carbohydrate content, and monitoring the patient’s glucose and electrolytes throughout the perioperative period.
- Ketogenic dietary therapy (KDT) is an effective treatment modality for patients with drug-resistant epilepsy (after 2 anticonvulsant drugs have failed) and status epilepticus.
- KDT is also a treatment for certain metabolic and neurologic disorders such as glucose transporter 1 deficiency syndrome, pyruvate dehydrogenase deficiency, autism-spectrum disorder, etc.1 Other indications and contraindications of KDTs are listed in reference.1
- Anesthesiologists now frequently care for these patients with the recent resurgence in interest in KDT.2
- The basic principle of KDTs involves using high-fat, low carbohydrate diets to induce and maintain ketosis through the production of ketone bodies. KDTs trigger the body to use fat instead of carbohydrates to produce energy.1,2
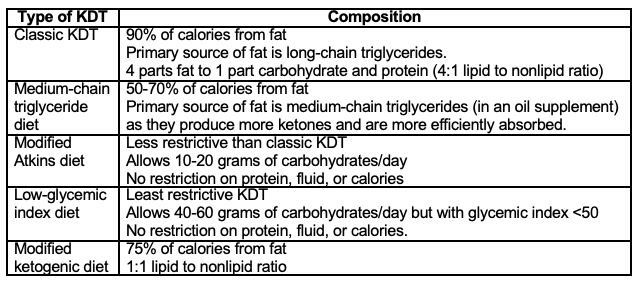
Table 1. Main types of ketogenic dietary therapy.1
- While the production of ketone bodies (acetoacetate, acetone, beta-hydroxybutyrate) is a hallmark feature of KDT, the exact anticonvulsant mechanism of KDT remains unknown. Proposed mechanisms include elevated plasma-free polyunsaturated fatty acids, reduced glucose fluctuations, increased activation of ATP-sensitive potassium channels, caloric restriction, and elevated brain amino acids.3
- Presence of the ketotic state is measured through serum ketone bodies and urine ketones. After ketosis is achieved, it may take up to 72 hours to see ketones in the urine.
Anesthetic Considerations
Preoperative Planning and Evaluation2
- Elective procedures should be scheduled as early in the day as possible to minimize the duration of fasting and decrease the likelihood of case delays. Prolonged fasting increases the risk of hypoglycemia in these patients.
- Consider consulting with the patient’s neurologist regarding the patient’s nutritional status, efficacy of KDT, concurrent anticonvulsant medications, and side effects from KDT.
- Preoperative administration of carbohydrate-containing electrolyte solutions and intravenous fluids should be avoided.
- Preoperative sedation with oral midazolam secondary to high carbohydrate content should be avoided. Alternatives for preoperative sedation include intranasal midazolam or dexmedetomidine.
- Preoperative administration of oral acetaminophen secondary to high carbohydrate content should be avoided (see Table below).
- Measuring the patient’s glucose levels preoperatively should be considered. Signs and symptoms of hypoglycemia include sweating, clammy, vomiting, increased sleepiness, confusion, tachycardia, rapid respirations, etc.
Intraoperative Management2
- Carbohydrate-containing medications and intravenous fluids should be avoided (see Table below).
- Current, preoperative doses of any intravenous anesthetics used in the treatment of status epilepticus should be maintained. These are titrated carefully to the electroencephalogram and should not be decreased. Common drugs that are used are propofol, midazolam, ketamine, alprazolam and rarely barbiturates.
- Clinicians should be mindful of patients who have been on propofol infusions for the treatment of status epilepticus. Increasing the dose of propofol should be avoided as this may put the patient at risk of propofol-infusion syndrome.
- Isotonic crystalloid solutions (normal saline or lactate Ringer’s solution) for volume replacement should be used. Using large volumes of normal saline secondary to the risks of hyperchloremic metabolic acidosis should be avoided.
- For major surgical procedures or those lasting greater than 3 hours, serum pH, glucose, electrolytes, and bicarbonate levels should be monitored every hour.
- Hypoglycemia should not be overcorrected. Clinicians should administer 1-2 mg/kg of dextrose if glucose < 40 mg/dL). Patients will have an attenuated response to glucagon. Dextrose should be used to correct severe hypoglycemia.
Postoperative Management2
- Carbohydrate containing medications and fluids should be avoided (see Table 2 below)
- The decision for inpatient monitoring versus same day discharge depends on the surgery/procedure and the patient’s comorbidities.
- Clinicians should advance diet as surgically appropriate, to resume KDT. Measuring serum or urine ketone levels should be considered.
- Intensive care unit (ICU) patients should return to the ICU on the same intravenous infusions, at the same dosage and rate that they were receiving preoperatively.
Carbohydrate Content of Anesthetic Drugs2
- If carbohydrates are administered to a patient on KDT, the body favors its uses over fat and ketosis is lost. Therefore, carbohydrate containing medications and fluids must be avoided.2
- Based on the carbohydrate ingredients identified in the drug package insert, medications are color-coded as green, yellow, and orange. Green-colored medications can be used per routine as no carbohydrates are listed in the package insert. Yellow-colored medications must be used with caution due to the unknown clinical significance of carbohydrates listed in the package insert. Orange-colored medications contain carbohydrates and should be avoided as much as possible. Table adapted from reference 2.
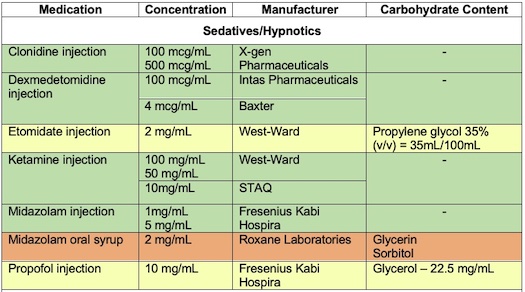
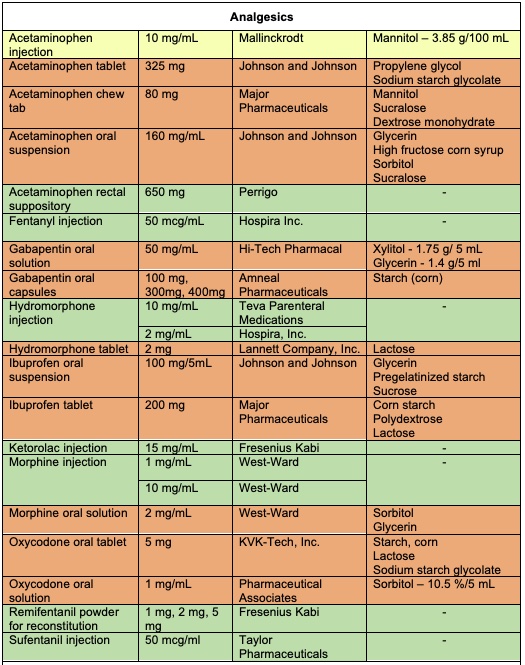
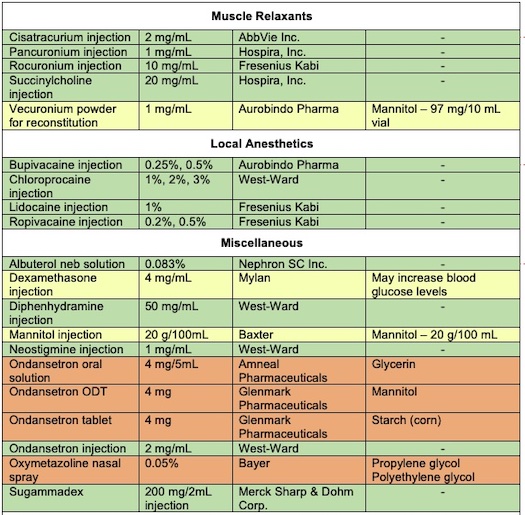
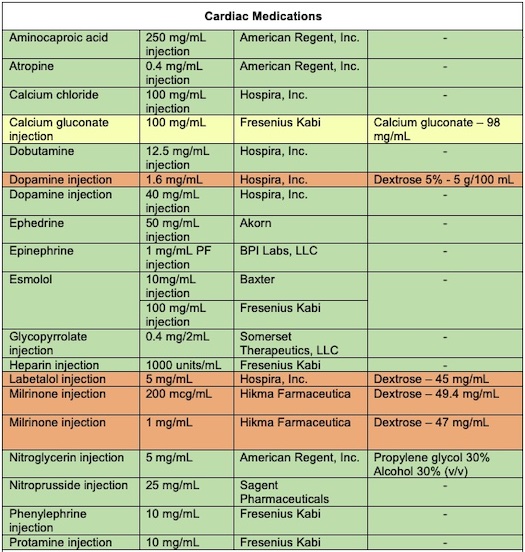
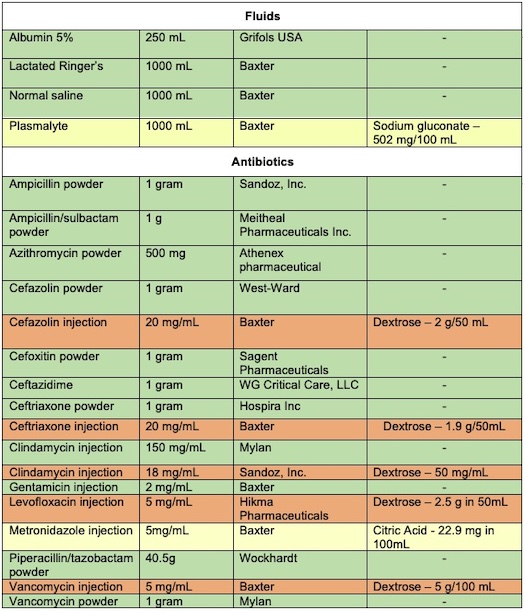
Table 2. Commonly Used Perioperative Medications That Usually Do Not Contain any Carbohydrates and Can be Used per Routine in Children on Ketogenic Dietary Therapies. Adapted from Conover ZR, et al. Perioperative management of children on ketogenic dietary therapies.2
References
- Kossoff EH, Zupec-Kania BA, Auvin S, et al. Optimal clinical management of children receiving dietary therapies for epilepsy: updated recommendations of the International Ketogenic Diet Study Group. Epilepsia Open. 2018; 3:175-92. PubMed
- Conover ZR, Talai A, Klockau KS, et al. Perioperative management of children on ketogenic dietary therapies. Anesth Analg. 2020;131(6): 1872-82. PubMed
- Bough KJ, Rho JM. Anticonvulsant mechanisms of the ketogenic diet. Epilepsia. 2007;48(1): 43. PubMed
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.