Copy link
Botulinum Toxin: Mechanism of Action and Clinical Use
Last updated: 03/14/2023
Key Points
- Botulinum toxins (BoNT) bind irreversibly to presynaptic cholinergic nerve terminals and inhibit the release of acetylcholine, thereby inducing muscle weakness.
- BoNT is used clinically for various conditions to reduce muscle spasticity.
- BoNT is the mainstay of the treatment for chronic migraine headaches. They can also be considered for other headaches and painful conditions.
Introduction
- BoNT is a neurotoxin produced by Clostridium botulinum bacteria. There are 7 serotypes (labeled as types A, B, C [C1, C2], D, E, F, and G), all of which block the release of acetylcholine from nerve endings, thereby inducing muscle weakness.1
- BoNTs are the most potent neurotoxins known to humans.1
- In the United States, four botulinum toxin types are FDA-approved for clinical use: three type A toxins and one type B toxin.2 Botox® is the brand name for onabotulinumtoxinA (OBTA).
Mechanism of Action
- BoNTs bind irreversibly to the presynaptic surface of cholinergic nerve terminals, which results in the inhibition of acetylcholine release, thereby inducing muscle weakness.2 The toxins enter the neuron by endocytosis and then interact with the soluble N-ethylmaleimide-sensitive factor attachment protein receptor (SNARE) apparatus to disrupt acetylcholine release2 (Figure 1).
- The seven serotypes of BoNT specifically interact with different components of the SNARE complex: synaptobrevin, SNAP-25, and syntaxin.2 The net effect is to prevent the exocytosis of acetylcholine-containing vesicles into the nerve terminal cleft and create effective chemical denervation.2
- BoNT types A, C, and E cleave SNAP-25.
- BoNT types B, D, F, and G cleave synaptobrevin.
- BoNT type C also cleaves syntaxin.
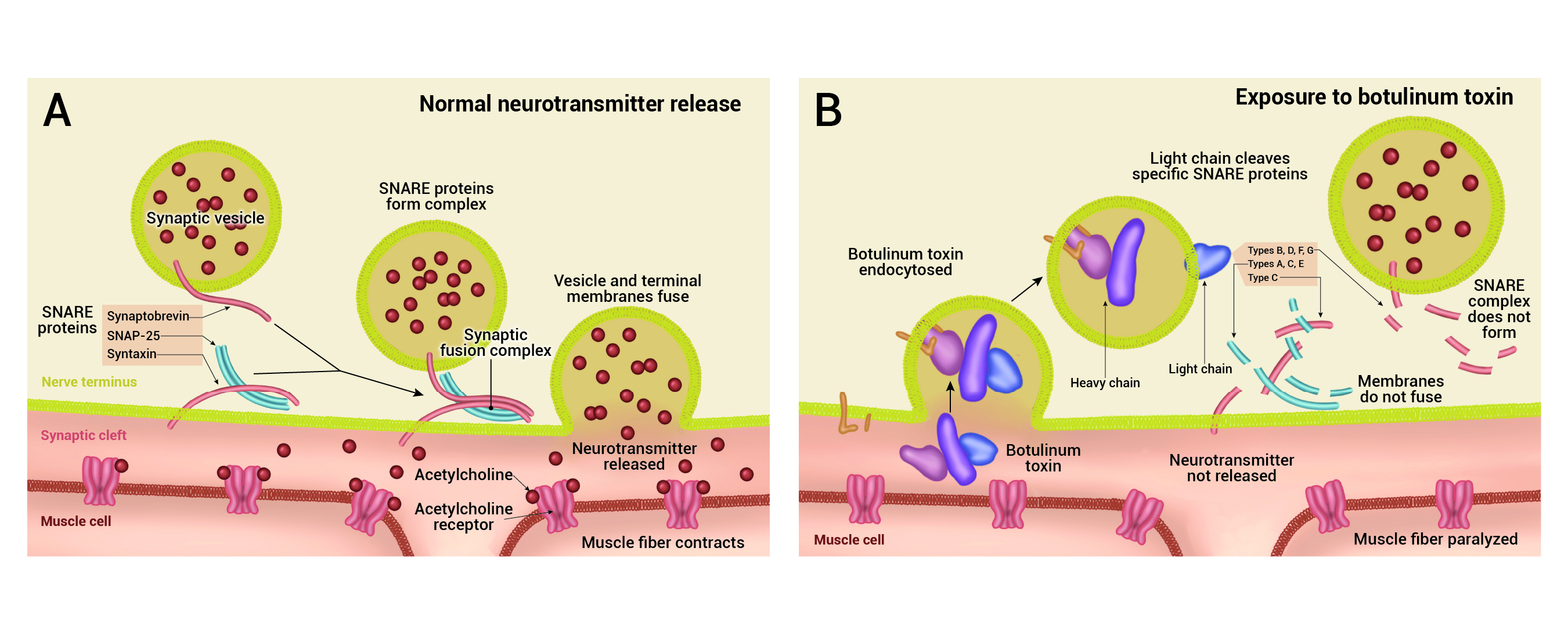
Figure 1. Mechanism of action of BoNT. Left panel: Acetylcholine release at the neuromuscular junction is mediated by the assembly of the SNARE fusion complex, allowing the membrane of the synaptic vesicles containing acetylcholine to fuse with the neuronal cell membrane. Right panel: Upon exposure to BoNT, it binds to the cell membrane, and enters the neuron by endocytosis. The light chain of BoNT cleaves specific sites on the SNARE protein preventing the complete assembly of the synaptic fusion complex, thereby blocking acetylcholine release. Adapted from Arnon SS, et al. Botulinum toxin as a biological weapon: medical and public health management. JAMA. 2021;285(8): 1059-70. PubMed
- Given as an intramuscular injection, the onset of action takes 24 to 72 hours. The peak effect lasts for about 4 to 6 weeks, with effects lasting up to 2 to 6 months.2 Days after exposure to the toxin, the axon fibrils begin to sprout and form junction plates on new areas of the muscle cell walls, rendering weakness reversible over a period of 3 months.2
- Some patients lose the beneficial response to BoNT, and it is thought to be due to the formation of antibodies to BoNT.1 Antibody formation is not associated with all toxins and may be decreased by maintaining at least 3-month intervals between injections and keeping doses as low as possible.2
- The botulinum toxin serotypes are thought to be immunologically distinct, and thus, there is some rationale for alternative serotypes to be tried if clinical resistance develops.3
- In animal models, the botulinum injection also inhibits nociceptive input by blocking substance P release. Thus, in addition to being an antispastic agent, the BoNT may have analgesic properties as well.1
Clinical Use
BoNT is used to treat various clinical conditions, including spasticity, cervical dystonia, strabismus, blepharospasm, overactive bladder, and several other cosmetic indications. This summary will focus on BoNT for chronic migraines and other painful conditions.
Chronic Migraines
- OBTA injections are a mainstay of the treatment for chronic migraine, which are characterized by headaches at least 15 days a month, and eight of these headache days must be migraine headaches or relieved by a triptan or ergot derivative.4
- Pooled analyses of data from two large multicenter, double-blind, randomized controlled trials showed that compared to placebo, OBTA injections resulted in significant improvements in multiple headache symptom measures, including the frequency of headache days.5
- However, some patients report a “wear-off” period days to weeks before the next OBTA injections are due with increased headache frequency.
- The mechanism of action of OBTA for chronic migraine involves the BoNT binding to receptors on the C-fiber nerve terminals and blocking the release of calcitonin gene-related peptide from peripheral c-fiber nerve endings. Muscle relaxation is not the primary mechanism of action of analgesia.
Other Headaches
- OBTA injections have also been used successfully for other headache patterns such as cluster headaches, trigeminal autonomic cephalalgias, chronic tension-type headaches, etc.4
Trigeminal Neuralgia
- BoNT is a treatment option for patients with trigeminal neuralgia who have failed conservative therapy or if surgery is not an option or is unsuccessful.4
Temporomandibular Disorder
- BoNT lessens pain levels in patients with temporomandibular disorder and bruxism. It can be used as a treatment option once conservative measures are ineffective.4
Side Effects
- BoNT acts at the neuromuscular junction but can affect other cholinergic sites, including the pre- and postganglionic sites of the autonomic nervous system.2 This can lead to side effects, including dry mouth and reduced sweating.2 Other side effects include pain, erythema, unintended paralysis of nearby muscles, flu-like symptoms, and nerve trauma.
References
- Barnes M. Botulinum toxin-mechanism of action and clinical use in spasticity. J Rehabil Med. 2003;(41 Suppl): 56-9. PubMed
- Burstein R, Blumenfeld AM, Silberstein SD, Manack Adams A, Brin MF. Mechanism of action of onabotulinumtoxinA in chronic migraine: a narrative review. Headache: The Journal of Head and Face Pain. 2020 Jul;60(7):1259-72. PubMed
- Čapek P, Dickerson T. Sensing the deadliest toxin: Technologies for Botulinum Neurotoxin Detection. Toxins (Basel). 2010;2(1):24-53. PubMed
- Becker WJ. Botulinum toxin the treatment of headache. Toxins (Basel). 2020;12(12): 803. PubMed
- Dodick DW, Turkel CC, DeGryse RE, et al. OnabotulinumtoxinA for treatment of chronic migraine: pooled results from the double-blind, randomized, placebo-controlled phases of the PREEMPT clinical program. Headache. 2010;50(6): 921. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.