Copy link
Fetal Heart Rate Tracing Interpretation
Last updated: 10/18/2023
Key Points
- Fetal heart rate (FHR) monitoring is a widely used intrapartum tool that allows providers to assess fetal well-being.
- The characterization of FHR tracing morphology has been standardized to allow for clear communication of interpretation of fetal status and to support intrapartum decision-making.
- Despite widespread use, limitations of FHR monitoring include high rates of inter- and intraobserver discrepancy and questionable efficacy mitigating poor fetal outcomes.
Introduction
- FHR monitoring has become a cornerstone in the assessment of intrapartum fetal wellbeing, with the technology being utilized in more than 85% of laboring patients in the United States.
- FHR is impacted by a constant balance of sympathetic and parasympathetic activation, which is controlled by the fetal brain.
- FHR patterns are interpreted to give a moment-to-moment assessment of fetal acid-base status as a proxy for fetal well-being.
- Despite widespread use, FHR monitoring has yet to clearly demonstrate benefit in mitigating poor fetal outcomes.1
Electronic Fetal Heart Rate Tracing (EFHRT) Mechanics
- FHR can be assessed with external or internal monitoring.
- External monitoring is conducted using ultrasound Doppler technology, where the Doppler device transmits its signal to a computer which interprets the input as FHR.
- Internal monitoring is achieved using a fetal electrode, which is a spiral wire affixed to the fetal scalp (or presenting part) and directly monitoring FHR.
- This method allows for increased accuracy in the assessment of FHR and is less affected by movement artifacts but is more invasive than external monitoring.
- Internal monitoring is frequently used when external monitoring is limited by patient acoustic properties or when maternal heart rate is similar to the FHR.
- A large retrospective cohort study demonstrated an association of fetal scalp injury and cephalohematoma, which occurred in 1.2% and 1.0% of cases respectively when a fetal scalp electrode was used for internal EFHRT.2
Categories of FHR Tracings
- In 2008, the American College of Obstetricians and Gynecologists, the Society for Maternal-Fetal Medicine, and the National Institute of Child Health and Human Development convened a workshop to create clearer standards for FHR interpretation and proposed a three-tier categorization of FHR tracings.3
- EFHRT are characterized by several features, including the baseline FHR, beat-to-beat variability, and the presence of accelerations and decelerations, which are further classified as early, variable, or late based on the morphology.
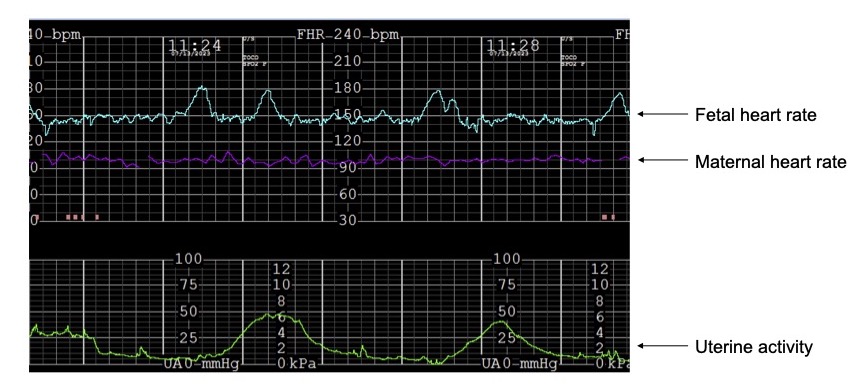
Figure 1. Baseline fetal heart rate tracing
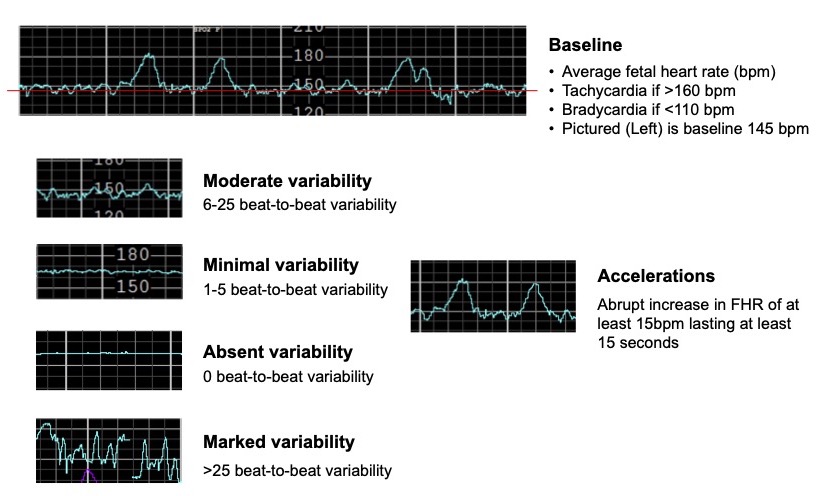
Figure 2. Fetal heart rate accelerations and beat-to-beat variability
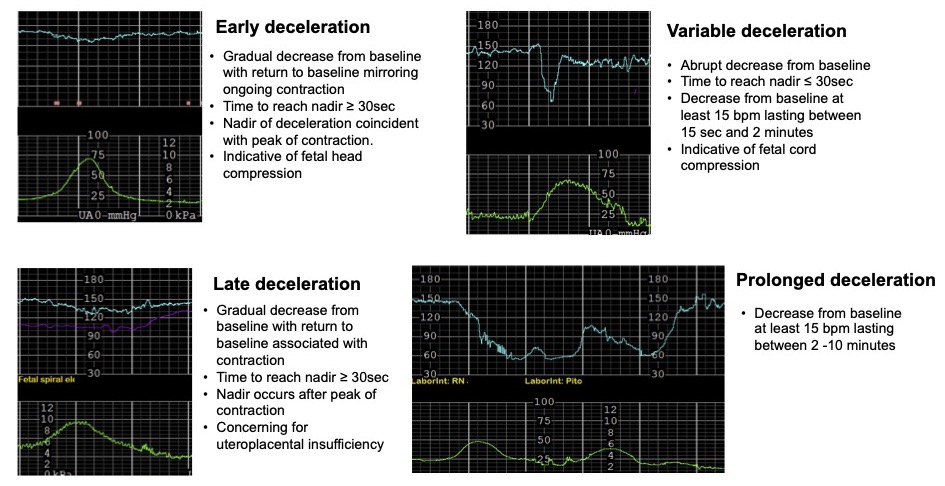
Figure 3. Types of fetal heart rate decelerations
- FHR tracings can be classified as categories I, II, and III (Table 1).4
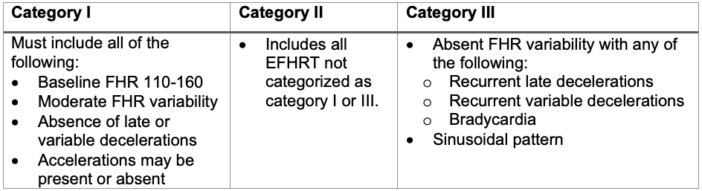
Table 1. Classification of FHR tracing4
Abbreviations: FHR, fetal heart rate; EFHRT, electronic fetal heart rate tracing
- Category I tracings are overall reassuring and indicate fetal well-being.
- Category II tracings are indeterminate and may indicate concern for fetal status.
- Recent work has identified that recurrent variable and late decelerations, and prolonged decelerations are features of Category II EFHRT concerning enough to lead obstetricians to cesarean delivery for nonreassuring fetal status.
- Category III tracings are indicative of significant fetal stress and concern for acidemia.
Clinical Interpretation and Anesthetic Management
- Clinical FHR monitoring pearls are listed in Table 2.
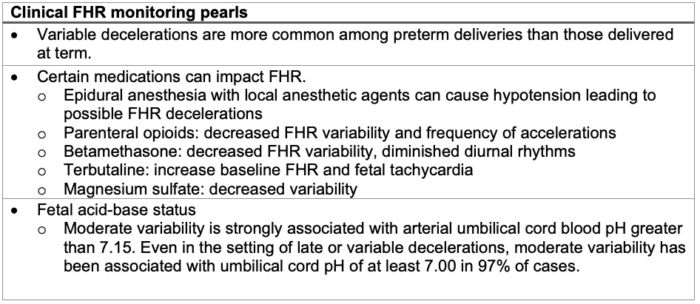
Table 2. Clinical fetal heart rate monitoring pearls
Abbreviation: FHR, fetal heart rate
- FHR changes, specifically decelerations, can be improved by an obstetric anesthesia team’s involvement in patient care (Tables 3 and 4).
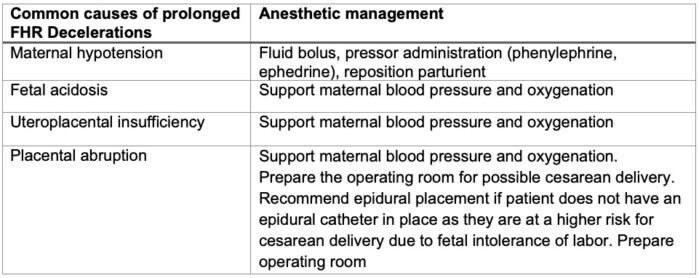
Table 3. Anesthetic management of prolonged fetal heart rate decelerations
Abbreviation: FHR, fetal heart rate
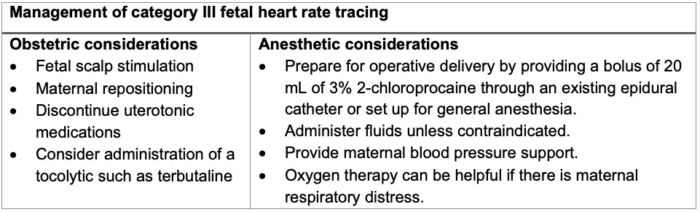
Table 4: Management of category III fetal heart rate tracing
Outcomes of EFHRT
- Meta-analyses have assessed the efficacy of EFHRT use during labor primarily to evaluate the rate of complications as well as the impact on rates of cesarean and operative vaginal deliveries (i.e., forceps and vacuum-assisted vaginal deliveries).5
- EFHRT is associated with a significant increase in the rate of cesarean and operative vaginal deliveries.
- The use of EFHRT was not associated with reduced rates of perinatal mortality or cerebral palsy but was associated with reduced risk of neonatal seizures.
- EFHTR may allow for intervention before harm occurs, as recent work has identified that infants delivered via cesarean section for non-reassuring fetal status were more likely to be acidemic at birth based on cord blood gases.6
References
- ACOG Practice Bulletin No. 106: Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstet Gynecol. 2009;114(1):192-202. PubMed
- Kawakita T, Reddy UM, Landy HJ, et al. Neonatal complications associated with use of fetal scalp electrode: a retrospective study. BJOG. 2016;123(11):1797-803. PubMed
- Macones GA, Hankins GD, Spong CY, et al. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines. Obstet Gynecol 2008;112:661–6 (Level III) PubMed
- Intrapartum Assessment. In: Cunningham F, Leveno KJ, Bloom SL, Dashe JS, Hoffman BL, Casey BM, Spong CY. eds. Williams Obstetrics, 25e. McGraw Hill; 2018, 457-81.
- Vintzileos AM, Nochimson DJ, Guzman ER, et al. Intrapartum electronic fetal heart rate monitoring versus intermittent auscultation: a meta-analysis. Obstet Gynecol. 1995;85(1):149-55. PubMed
- Rimsza RR, Frolova AI, Kelly JC, et al. Intrapartum electronic fetal monitoring features associated with a clinical diagnosis of nonreassuring fetal status. Am J Obstet Gynecol MFM. 2023;5(9):101068. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.