Copy link
Hypothyroidism
Last updated: 05/23/2025
Key Points
- Primary and secondary hypothyroidism are the two main forms of hypothyroidism, both characterized by dysregulation of thyroid hormone production.
- Hypothyroidism can be classified by severity, based on lab values and clinical presentation. Subclinical hypothyroidism rarely requires changes to anesthetic management, but overt hypothyroidism can range from mild to severe, with clinical significance.
- Clinically significant hypothyroidism can disrupt the proper function of many organ systems, especially the cardiac, pulmonary, and gastrointestinal systems.
- Management of hypothyroidism during anesthesia can include hormone replacement, changes in airway management, or vigilance for impacted cardiovascular or pulmonary physiology.
- Myxedema coma is a clinical state sometimes seen in severe hypothyroidism that can occur in the perioperative period and must be managed aggressively.
Introduction
- Hypothyroidism is an endocrine disorder marked by insufficient thyroid hormone production by the thyroid gland. This leads to reduced metabolic activity and, thus, downstream effects in organ systems that rely on normal thyroid hormone levels.
- Hypothyroidism is ten times more common in women compared to men.1
- Worldwide, the most common cause of hypothyroidism remains iodine deficiency,1 whereas in the United States, prior radioactive iodine treatment or prior thyroid surgery are the most common causes,2 followed by autoimmune thyroid disease (i.e., Hashimoto’s thyroiditis).1
- Clinical diagnosis of hypothyroidism can be difficult due to its slow and progressive manifestations in the body.
- Hypothyroidism can be classified as primary (decreased production of thyroid hormone in the thyroid gland) or secondary (decreased upstream stimulating hormone release by the pituitary gland), with both types exhibiting decreased thyroid hormone available to act on tissues. Much more rarely, decreased upstream hypothalamic hormone production can cause decreased thyroid hormone underproduction. This presents similarly to secondary hypothyroidism but would be labeled tertiary hypothyroidism.
Etiology
- In a normally functioning thyroid gland, thyroid hormone production is regulated in a classical negative feedback loop mechanism (Figure 1). Thyroid-stimulating hormone (TSH) is released from the anterior pituitary gland and is the primary regulator of thyroid hormone synthesis.
- TSH release from the pituitary is regulated by thyroid-releasing hormone (TRH), which is produced by the hypothalamus.
- Thyroxine (T4) and triiodothyronine (T3) are the circulating thyroid hormones that affect tissues and body systems. T4 is only produced in follicle cells of the thyroid gland; T3 is also produced in follicle cells (~20%) but is also created by extrathyroidal conversion of T4 to T3 (~80%). After conversion to iodide, dietary iodine is necessary to produce T4 and T3.
- Increased levels of circulating T4 and T3 act in a negative feedback manner to suppress hypothalamic TRH release, decreasing pituitary TSH release, and thus allowing fine control of plasma levels of T4 and T3.
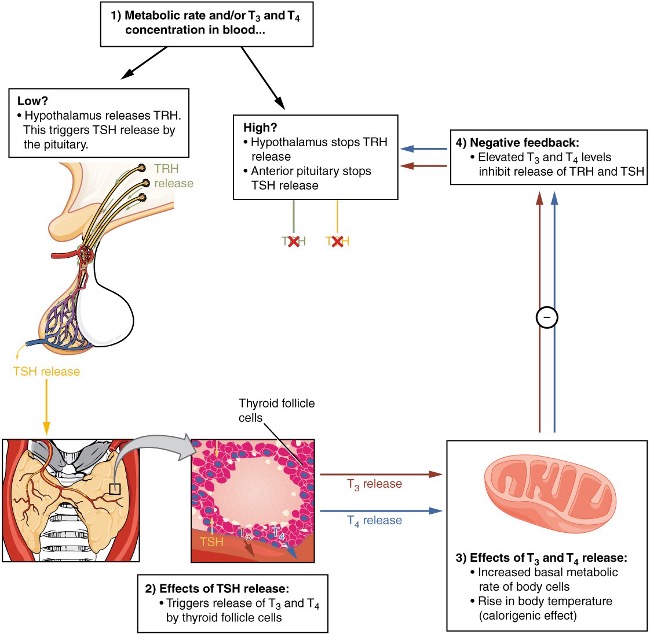
Figure 1. Negative feedback mechanism of thyroid hormone synthesis. Source: OpenStax College. Wikimedia Commons. 2013. Accessed 8 January 2025. Link
Primary Hypothyroidism
- Primary hypothyroidism is characterized by a decreased production of thyroid hormones T4 and T3 in the thyroid gland, with intact hypothalamic and pituitary feedback, leading to an increase in levels of TSH due to feedback3,4 (Table 1). Elevated TSH levels cannot correct the low circulating levels of T3 and T4 due to insufficient production.
- Primary hypothyroidism is the most common type of hypothyroidism, accounting for 95% of cases.4
Secondary Hypothyroidism
- Causes of decreased production of thyroid hormone include iodine deficiency (the most common cause worldwide), injury to the thyroid gland, prior radioactive iodine treatment or surgery on the thyroid (the most common causes in the United States), or autoimmune thyroid disease (Hashimoto’s thyroiditis). Other causes include drug effects, external radiation, and congenital defects in thyroid gland development.4,5
- Secondary hypothyroidism is characterized by decreased serum levels of T4 and T3, but also decreased levels of TSH, indicating a breakdown of typical negative feedback (Table 1). Secondary hypothyroidism often arises from a deficiency in the pituitary gland or hypothalamus, which can be caused by factors such as a pituitary tumor, empty sella syndrome, or infiltrative disorders.5 Diminished TRH or TSH levels lead to reduced stimulation of the thyroid gland, resulting in lower production of T3 and T4.1
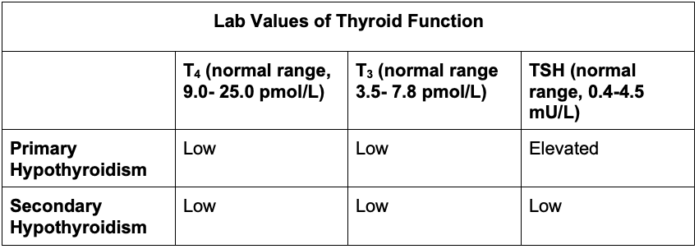
Table 1. Lab values of thyroid function. Adapted from references 1, 3, 4 and 5.
Medication Effects on Thyroid Hormone Synthesis
Various drugs can affect thyroid function through a variety of mechanisms and thus create clinical states that fall into the primary and secondary hypothyroidism classifications.5
- Medication-related inhibition of the peripheral conversion of T4 to T3 mimics primary hypothyroidism and can occur with amiodarone, phenobarbital, carbamazepine, propranolol, and glucocorticoids. Of note, propylthiouracil also inhibits peripheral conversion and is used to treat hyperthyroidism. Carbimazole and methimazole instead block the production of thyroid hormone, and are used to treat hyperthyroidism.1
- Medication-related suppression of TSH release can mimic secondary hypothyroidism, and can occur with lithium, dopamine, and glucocorticoids.5
Clinical Presentation
Signs and Symptoms
- Common symptoms of patients with hypothyroidism include weight gain, fatigue, sweating, brittle hair, cold intolerance, depression, and constipation. Physiological signs may include bradycardia, hypoventilation, hypertension, macroglossia, anemia, periorbital edema, etc. (Table 2).
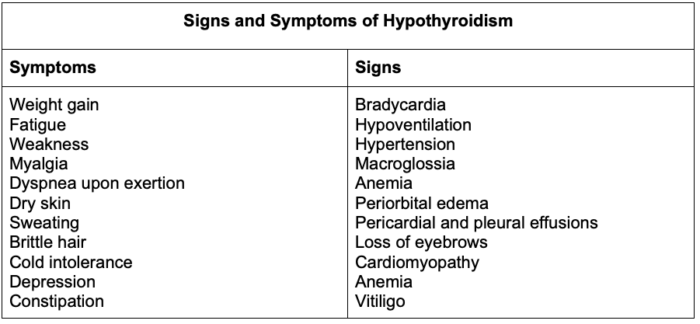
Table 2. Signs and symptoms of hypothyroidism. Adapted from references 1, 3 and 4.
Severity of Hypothyroidism
- Hypothyroid patients may present with varying levels of clinical severity. Typically, clinical manifestations are used to grade severity, regardless of mechanism (primary vs secondary hypothyroidism). However, since primary hypothyroidism is much more common (95%), the degree of TSH elevation is also used to grade severity.
Subclinical Hypothyroidism
- Although values can fluctuate, subclinical hypothyroidism can be associated with 5.0–10 milliunits/L of TSH and normal values of T4 and T3.3 Patients in the subclinical category may be asymptomatic or display minor symptoms such as fatigue or hair loss.6
Overt Hypothyroidism
- Patients with overt hypothyroidism display TSH lab values of > 20 mU/L, with reduced free T4 and T3 circulation.3 Often, obvious signs and symptoms (Table 2) of overt hypothyroidism will be displayed in the clinical presentation of the patient.6 Clinical severity can range from mild to moderate to severe, without specific differentiating criteria.
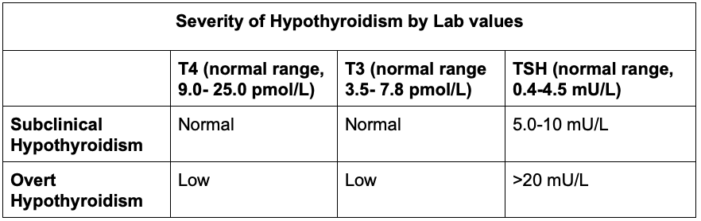
Table 3. Severity of hypothyroidism by lab values. Adapted from references 1, 3, 4 and 5.
Pathophysiology
- The clinical manifestations of hypothyroidism impact many different organ systems. In addition to the typical signs and symptoms helpful for clinical diagnosis, pathophysiologic changes relevant to anesthetic considerations include effects on drug clearance, electrolyte concentrations, and pulmonary, cardiovascular, and gastrointestinal effects.
Drug Clearance
- Drugs administered at typical dosages may elicit an increased effect due to a reduction in clearance efficiency in the hypothyroid patient. Drugs that are affected include but are not limited to anticoagulants, antiseizure agents, hypnotics, and opioid drugs.5 Drug toxicity can occur if the dosage of affected drugs is not considered carefully.
Metabolic Effects
- Electrolyte abnormalities can occur in patients with hypothyroidism. While rare, hyponatremia may arise due to a diminished ability to clear water effectively.5
- Lipid clearance can be decreased in patients with hypothyroidism, which leads to elevated free fatty acids, low-density lipoproteins, and total cholesterol. Significant hyperlipidemia attributable to thyroid disease can be seen in severe hypothyroidism, but is much more rare in subclinical hypothyroidism.5
Pulmonary Effects
- Patients with hypothyroidism may experience dyspnea on exertion or respiratory muscle weakness. Additionally, pleural effusion or intrinsically decreased lung volumes can lead to restrictive pulmonary physiology.5
- Sleep apnea may occur secondary to macroglossia.
- Hypoventilation may be caused by a reduction in central respiratory drive otherwise expected from hypoxia or hypercapnia.5
Cardiovascular Effects
- Bradycardia may be present due to decreased autonomic tone, and a prolonged QT interval may result from changes in K+ channel functions. These changes may cause ventricular arrhythmias or other arrhythmias.7
- Cardiac output may be reduced secondary to decreased heart rate and contractility. A decrease in heart contractility results from thyroid hormone gene regulation of myocardial enzymes involved in myocardial contractility and relaxation.
- Hypothyroidism can cause a decrease in responsiveness to alpha and beta-adrenergic agonists and downregulation of alpha and beta-adrenergic receptors.
- Hypothyroid patients may be predisposed to increased systemic vascular resistance. Additionally, patients may have diastolic pressure elevation that is out of proportion to systolic pressure, leading to narrowing of the pulse pressure. Diastolic dysfunction can also occur due to a reduction in diastolic compliance and filling. New congestive heart failure secondary purely to hypothyroidism is rare, but worsening of pre-existing congestive heart failure is common.5
Gastrointestinal Effects
- Expected changes in digestion may include slowed peristalsis, changes in bowel movements, constipation, and malabsorption, which can increase perioperative aspiration risks.5
Myxedema Coma
- Myxedema coma is a rare and life-threatening complication of severe hypothyroidism. Myxedema coma can come after a steady progression of severe hypothyroidism or can be precipitated by acute illness. Myxedema coma is differentiated from chronic severe hypothyroidism by increased severity of decreased mental status or coma, along with particularly severe hypothermia, bradycardia, and hypoventilation. Patients who have developed myxedema coma face mortality rates as high as 25-50%.5
- Myxedema coma is more commonly seen in older female patients. The clinical syndrome also includes decreased mental status, hypothermia, hypotension, bradycardia, hypoventilation, seizures due to concurrent hyponatremia, and swollen lips and eyes.1
- Swelling of the face and lips may also extend into the airway.
- The onset of myxedema coma in long-term hypothyroid patients can be precipitated by other acute events, such as trauma, usage of sedative medications, heart failure, infection, myocardial infarction, or a thrombolytic event.1
- Serum TSH, free T4, and cortisol lab values should be evaluated to confirm the clinical diagnosis.
Treatment of Myxedema Coma
- Due to the life-threatening nature of myxedema coma, the condition should be treated promptly and aggressively, with intravenous levothyroxine and glucocorticoids.
- Adrenal insufficiency is likely to coexist with the condition and should be treated with stress–dose intravenous steroids until laboratory data excludes adrenal dysfunction. Treatment includes 100mg of hydrocortisone IV, then 25 mg IV q6h4. Administration of levothyroxine prior to glucocorticoids in myxedema coma can provoke an adrenal crisis.5
- Levothyroxine treatment involves intravenous administration of 200–300 mcg over 5–10 min initially, and then 100 mcg IV every day.4 The intravenous route is preferred over oral, due to the possibility of impaired gastrointestinal absorption.5
- Hypothermia should be managed by covering the patient or gradual warming. High-intensity warming can risk rapid peripheral vasodilation and subsequent hypotension.
Anesthetic Management
Preoperative Evaluation
- Minimal or subclinical hypothyroidism typically does not impose risks on the perioperative period but should be considered in clinical management as a precaution.5
- In patients with overt hypothyroidism, elective surgery should be postponed until a euthyroid state is achieved to avoid complications of cardiac and respiratory decompensation, as well as myxedema coma.2
- For patients with controlled hypothyroidism on levothyroxine supplementation, thyroid hormone replacement should be continued perioperatively, including on the day of surgery.2,4
- In patients with overt hypothyroidism undergoing required surgery before correction to a euthyroid state, regional nerve blocks should be used whenever possible, especially if doing so can avoid general anesthesia, due to the risk of anesthetic complications and potential barriers to intubation.
- Patients with severe hypothyroidism who require emergency surgery should be given a loading dose of levothyroxine. For patients with suspected adrenal crisis, stress-dose glucocorticoids should be administered simultaneously.5
Intraoperative Care
- Most anesthetic agents can be used without difficulty in hypothyroid patients. Ketamine is sometimes chosen as an induction agent, given its sympathetic stimulation.4 There is little if any change in the minimum alveolar concentration of volatile agents. However, hypothyroid patients in general may show delayed emergence and prolonged postoperative sedation.2
- Patients with severe hypothyroidism may have airway complications from thyroid disease. Enlarged tongues, sleep apnea, delayed gastric emptying, decreased gastric motility, or vocal cord edema may impact airway management. Rapid sequence induction and vigilance for aspiration should be considered.2 In severe cases of vocal cord edema, awake fiberoptic intubation may be indicated.3
- Hypothyroid patients may present with goiter. Goiter is a thyroid gland swelling resulting from compensatory hypertrophy and hyperplasia of follicular epithelium secondary to a reduction in thyroid hormone output (Figure 2). A significant goiter may externally compress the airway after induction and neuromuscular blockade, leading to a difficult airway. Large substernal goiters can behave as anterior mediastinal masses and cause intrathoracic airway obstruction after induction of general anesthesia. Such goiters can also cause superior vena cava and/or cardiac compression. Imaging should be used to determine the depth of the goiter present and guide airway management.4

Figure 2. Presentation of goiter. Source: Doc James. Wikimedia Commons. 2023. Accessed 8 January 2025. Link
- Cardiovascular manifestations of severe hypothyroidism indicate need for closer monitoring, as bradycardia, slow rate atrial fibrillation, ventricular arrhythmias, and reduced cardiac output may occur.2
- Please see the OA summary on Anesthesia for Thyroidectomy for more details. Link
Postoperative Period
- Hypothyroid patients are more susceptible to obstructive sleep apnea and the prolonged effects of medications used intraoperatively.
- Body temperature should be monitored postoperatively, given the possibility of hypothyroid-related hypothermia.
- Fluid and electrolyte disturbances, especially hyponatremia, may occur in the postoperative period.
References
- Sharma MP, Cetera B. Thyroid disease and surgery. Anaesthesia & Intensive Care Medicine. 2020; 21(11): 558-71. Link
- Sweitzer BJ, Opera AJ, Gerlach RM. Anesthetic implications of concurrent diseases. In: Gropper, MA. Miller’s Anesthesia. Volume 1. Tenth edition. Philadelphia, PA; Elsevier; 2025: 873-929.
- Zuo L, Dillman D. Endocrine disease. In: Hines R, Jones S. Stoelting's Anesthesia and Co-Existing Disease. Eighth edition. Philadelphia, PA Elsevier; 2022: 439-64.
- Schwartz JJ, Akhtar S. Endocrine function. In: Cullen B, Stock C, et al. Barash, Cullen, and Stoelting’s Clinical Anesthesia. Ninth edition. Philadelphia, PA; Wolters Kluwer; 2024: 274-1303.
- Sipos J, Cance WG. Thyroid disorders. In: Civetta. Taylor & Kirby's Critical Care Medicine. Fifth edition. Philadelphia, PA; Wolters Kluwer; 2018: e376-e86.
- Murkin JM. Anesthesia and hypothyroidism: a review of thyroxine physiology, pharmacology, and anesthetic implications. Anesth Analg. 1982; 61(4): 371-83. PubMed
- Deegan R, Furman WR. Cardiovascular manifestations of endocrine dysfunction. J Cardiothorac Vascular Anesth. 2011; 25(4):705-20. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.