Copy link
Reversal of Neuromuscular Blockade: Neostigmine
Last updated: 04/06/2023
Key Points
- Neostigmine works by inhibiting cholinesterase and increasing acetylcholine levels to compete with nondepolarizing neuromuscular blocking agents (NMBA) to bind nicotinic acetylcholine receptors (nAChR) at the neuromuscular junction.
- Neuromuscular monitoring, preferably quantitative, is necessary to determine the appropriate dosing and timing of administration of neostigmine.
- Neostigmine activity is subject to a ceiling effect and is unable to reverse deep levels of neuromuscular blockade.
- Paradoxical paralysis may occur if higher than necessary doses of neostigmine are administered.
- Muscarinic side effects with neostigmine administration are problematic and can be mitigated with the concurrent use of anticholinergic (antimuscarinic) agents.
Introduction
- The use of nondepolarizing NMBA places patients at risk of residual neuromuscular blockade (rNMB) and potential respiratory compromise if the effects of these agents are not resolved at the end of surgery and anesthesia.
- Return of adequate strength, defined by a train-of-four ratio (TOFR) ≥ 0.9, should be confirmed prior to tracheal extubation.
- Recovery from neuromuscular blockade can occur spontaneously over time (redistribution, metabolism, and excretion) or may be facilitated by the administration of an antagonist or “reversal agent.”
- Antagonism of NMBAs has historically been accomplished with anticholinesterase agents, with neostigmine being the most commonly used agent.
Mechanism of Action
- Neostigmine has a wide spectrum of activity and can antagonize both aminosteroidal and benzylisoquinolinium NMBAs.
- Neostigmine inhibits acetylcholinesterase, preventing the breakdown of acetylcholine and increasing its concentration at the neuromuscular junction.1
- Increased acetylcholine levels at the neuromuscular junction may displace and outcompete NMBAs for binding at nAChRs1 (Figure 1).
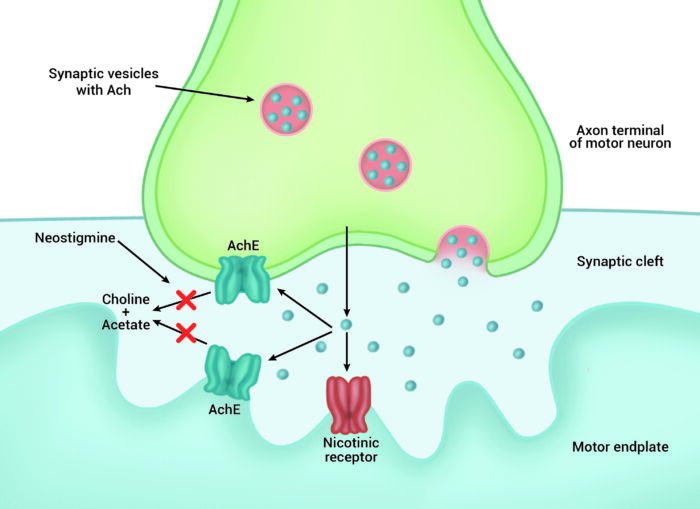
Figure 1. Mechanism of action of neostigmine. Inhibition of acetylcholinesterase (AChE) increases acetylcholine (ACh) levels at the neuromuscular junction. This facilitates the displacement of neuromuscular blocking agents and competitive binding of ACh at nicotinic acetylcholine receptors (nAChR), signaling muscular contraction.
Ceiling Effect
- Acetylcholinesterase inhibition with neostigmine reaches its peak effect approximately 10 minutes after administration, and adequate time must be given for neostigmine to exert its full effect.
- With maximum doses of neostigmine, full inhibition of acetylcholinesterase is achieved, and further increases in acetylcholine levels are not possible with additional doses of neostigmine.
- This “ceiling effect” results in the inability of neostigmine to antagonize deep levels of neuromuscular blockade (Table 1).
- Recovery from residual weakness following the peak effect of maximum neostigmine dosing will be dependent on the metabolism and elimination of the remaining NMBAs (i.e., spontaneous recovery).
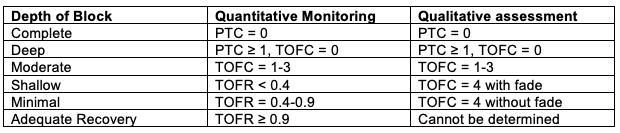
Table 1. Levels of neuromuscular blockade are shown as measured at the adductor pollicis muscle by quantitative monitoring or qualitative assessment with the use of a peripheral nerve stimulator. PTC=post-tetanic count; TOFC=train-of-four count; TOFR=train-of-four ratio. Adapted from Naquib M, et al. Anesth Analg 2018:127:71-80.2
Dosing and Timing of Administration
- The use of a peripheral nerve stimulator (PNS), or ideally quantitative monitoring is necessary to determine the proper dosing and timing of administration of neostigmine.
- Doses of neostigmine ranging from 0.015-0.07 mg/kg, up to 5 mg total, have been reported, though higher doses do not necessarily lead to more effective or efficient recovery, especially when administered at inappropriately deep levels of blockade.
- It is best to wait until the return of the 4th twitch (TOFC = 4) prior to the administration of neostigmine, though even this is not guaranteed to produce adequate reversal (TOFR ≥ 0.9).
- The odds of achieving adequate reversal with neostigmine are improved with a greater return of spontaneous strength at the time of its administration (Table 1).
- Neostigmine is most effective when spontaneous recovery to a minimal level of blockade has occurred.
- Moderate levels of blockade require larger doses and longer times for adequate recovery to occur.
- Neostigmine is unable to facilitate reversal from deep levels of blockade, and time to adequate reversal from this level will be determined by spontaneous recovery.
- Inadequate recovery, as determined by a TOFR <0.9 at 10 minutes, indicates either a relative underdosing of neostigmine has occurred or that the level of blockade is too deep for facilitated reversal alone to achieve a TOFR ≥ 0.9.
- Recommended dosing and timing of neostigmine administration for reversal of nondepolarizing neuromuscular blockade, depending on the availability of monitoring devices in one’s practice are shown in figure 2.3-5
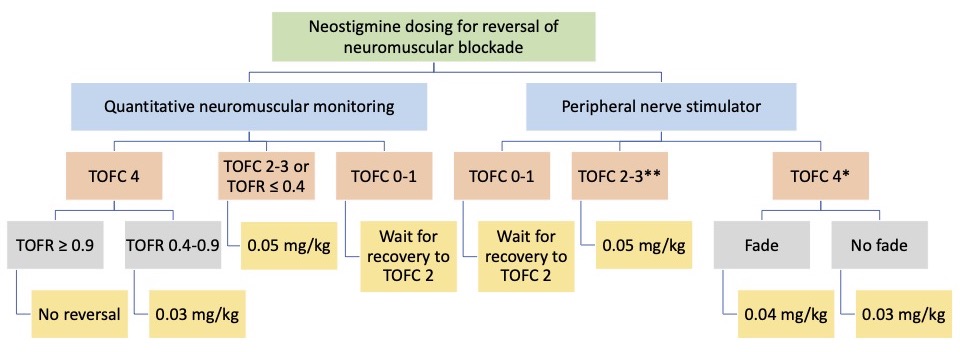
Figure 2. Neostigmine dosing recommendations depending on the depth of neuromuscular blockade measured with qualitative (peripheral nerve stimulator) or quantitative neuromuscular monitoring. TOFC=train-of-four count; TOFR=train-of-four ratio. + Wait at least 10 minutes for the peak effect of neostigmine; **Peak effect at 10 minutes may be inadequate to reverse neuromuscular blockade, and further return of strength will depend upon spontaneous recovery.
Paradoxical Paralysis
- Neostigmine doses beyond what is indicated by the patient’s depth of blockade may lead to paradoxical weakness.6
- Cholinesterase inhibition by neostigmine may increase acetylcholine levels by (1) preventing its breakdown and (2) increasing its release from presynaptic vesicles, leading to sustained depolarization, similar to that seen with succinylcholine.7
- Empiric or routine administration of maximum neostigmine doses is not recommended.
Muscarinic Side Effects
- Neostigmine increases the available acetylcholine to bind at nAChR of the neuromuscular junction, but also at parasympathetic, muscarinic, and acetylcholine receptors (AChR).
- Binding of muscarinic AChR produces undesirable side effects (Table 2).
- Concurrent administration of an anticholinergic (antimuscarinic) agent such as atropine or glycopyrrolate can mitigate the undesirable muscarinic effects, though they may still be seen.
- Glycopyrrolate is often administered with neostigmine as it has a similar time to onset.
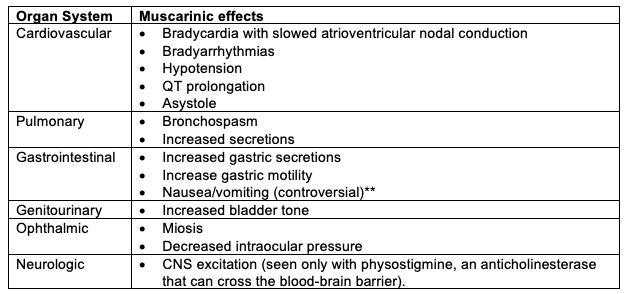
Table 2. Muscarinic side effects of neostigmine. ** Studies are inconclusive to support the increased risk and omission of neostigmine for prevention of postoperative nausea and vomiting.8
References
- Murphy G, De Boer HD, Eriksson LI, Miller RD. Reversal (antagonism) of neuromuscular blockade. In: Gropper MA, Miller RD, eds. Miller’s Anesthesia. 9th ed. Elsevier; 2020:832-64.
- Naguib M, Brull SJ, Kopman AF, et al. Consensus statement on perioperative use of neuromuscular monitoring. Anesth Analg. 2018;127(1):71-80. PubMed
- Kopman AF, Eikermann M. Antagonism of non-depolarising neuromuscular block: current practice. Anaesthesia. 2009;64 Suppl 1:22-30. PubMed
- Brull SJ, Kopman AF. Current status of neuromuscular reversal and monitoring: Challenges and opportunities. Anesthesiology. 2017;126(1):173-90. PubMed
- Weigel WA, Thilen SR. Neuromuscular blockade monitoring and reversal: A clinical and pharmacoeconomic update. Adv Anesth. 2021;39:169-88. PubMed
- Caldwell JE. Reversal of residual neuromuscular block with neostigmine at one to four hours after a single intubating dose of vecuronium. Anesth Analg. 1995;80(6):1168-74. PubMed
- Nair VP, Hunter JM. Anticholinesterases and anticholinergic drugs. Continuing Education in Anaesthesia Critical Care & Pain. 2004;4(5):164-8. Link
- Luo J, Chen S, Min S, et al. Reevaluation and update on efficacy and safety of neostigmine for reversal of neuromuscular blockade. Ther Clin Risk Manag. 2018;14:2397-2406. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.