Copy link
Cigarette Smoking and Anesthesia
Last updated: 05/10/2023
Key Points
- Smoking significantly increases perioperative morbidity and mortality due to the acute effects of diminished oxygen reserves and chronic effects of pulmonary inflammation and increased sympathetic tone.
- Nicotine’s action on the nicotinic cholinergic receptor is responsible for smoking addiction and alterations in the physiology of most organ systems.
- Preoperative smoking cessation reduces postoperative complications risk and improves long-term health.
Introduction
- According to the Centers for Disease Control and Prevention, cigarette smoking among adults in the United States has declined from 20.9% in 2005 to 12.5% in 2020. However, approximately 30.8 million adults currently smoke, and smokers comprise a significant proportion of surgical patients.1,2
- Cigarette smoking is a major modifiable risk factor for perioperative mortality and morbidity.
Nicotine Addiction
- Inhaled nicotine from cigarette smoking readily crosses the blood-brain barrier.
- The chemical structure of nicotine is similar to acetylcholine (Figure 1). Nicotine stimulates nicotinic cholinergic receptors and indirectly causes the release of neurotransmitters such as noradrenaline, adrenaline, vasopressin, serotonin, β-endorphin, and dopamine. Dopamine is released in the mesolimbic area, corpus striatum, and frontal cortex.3 Dopamine signals a pleasurable experience and plays a critical role in nicotine addiction.
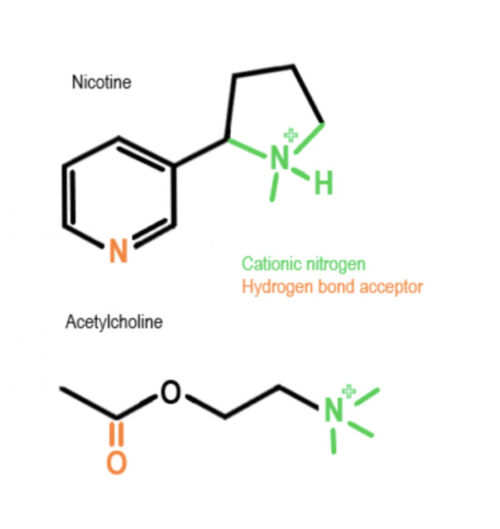
Figure 1. Nicotine and acetylcholine have similar chemical structures.
- Nicotine addiction may result from the stimulation of dopaminergic neurons in the midbrain and the nucleus accumbent, which are critical in drug-induced reward.3
- Repeated exposure to nicotine desensitizes nicotinic cholinergic receptors leading to tolerance and dependence. Withdrawal symptoms occur when desensitized receptors become aroused during periods of smoking abstinence.3
- Nicotine withdrawal increases extrahypothalamic corticotropin-releasing factors, activating the stress response in the brain felt as anxiety and stress during abstinence.3
- Ongoing genomic studies have identified gene loci and variants of nicotinic cholinergic receptors that may increase proclivity for nicotine addiction.3
Smoking and Perioperative Outcomes
- Smoking increases the risks of perioperative complications (Table 1).4
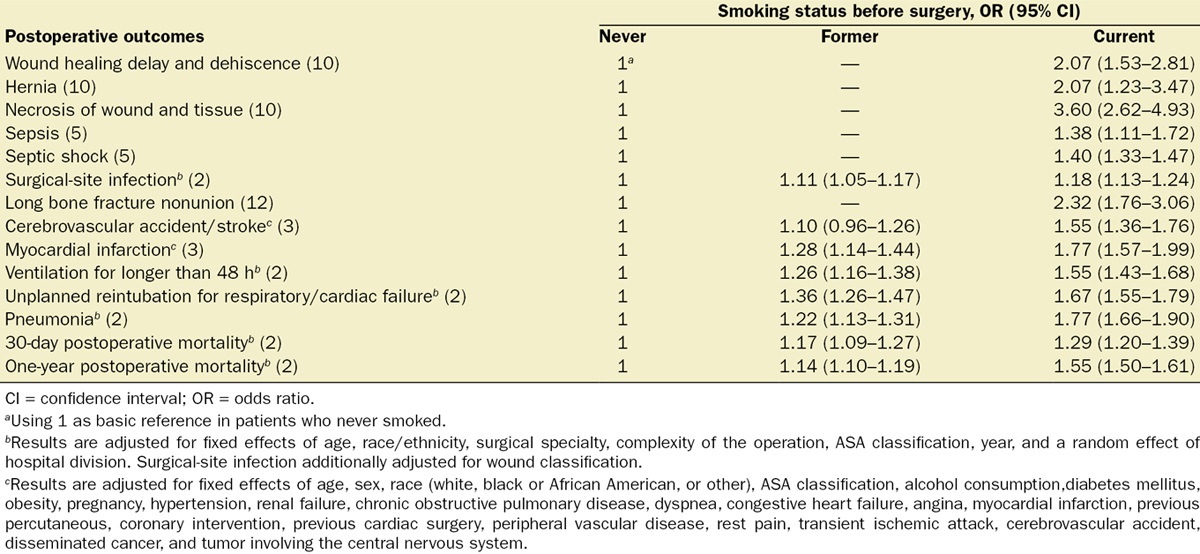
Table 1. Odd ratios of postoperative outcomes among current and former smokers compared with patients who never smoked. Used with permission from Yousefzadeh A, et al. Smoking cessation: The role of the anesthesiologist. Anesth Analg. 2016.4
Effects on Organ Systems
Cardiovascular System
- Nicotine’s effects on peripheral chemoreceptors include increased adrenaline secretion from the adrenal medulla, direct stimulation of the carotid and aortic bodies, and increased sympathetic tone from the autonomic ganglia.5
- In the short term, the increased sympathetic tone results in elevated blood pressure, heart rate, and peripheral vascular resistance.
- The increased myocardial contractility and oxygen demand, coupled with a decrease in coronary blood flow from an increase in coronary vascular resistance, leads to a decrease in the myocardial oxygen supply: demand ratio.5
- These cardiovascular effects lead to hemodynamic lability during anesthesia and surgery.
- Long-term smoking increases oxidative stress and inflammation.
- Endothelial cell damage accelerates vascular atherosclerosis.
- Platelet adhesion causes hypercoagulability and thrombosis. Smokers are at higher risks of perioperative myocardial infarction (odds ratio 1.77), and cerebral vascular accidents (odds ratio 1.55) (Table 1).4
Respiratory System
- Smoke inhalation decreases cilia movement in the airway and lungs, leading to ineffective clearing of debris and secretions and overall increased risks of postoperative pneumonia (odds ratio 1.77) and respiratory failure (odds ratio 1.67) (Table 1).
- Pulmonary epithelial inflammation acutely causes decreased surfactant production and small airway narrowing.6
- There is worsening ventilation/perfusion mismatch.
- Increased resistance [Q = πPr4/8ηl (Q=flow rate, P=pressure, r=radius, η= viscosity, l=length)] reduces airflow.
- Chronic pulmonary inflammation causes scarring and destruction of collagen and elastase. Noncompliant airways may require higher ventilatory inspiratory pressure, increasing the risks of barotrauma and acute respiratory distress syndrome.6
- Airway irritability and decreased compensatory pulmonary reserve increase the risks of adverse respiratory events such as laryngospasm, bronchospasm, cough, hypoventilation, hypoxemia, negative-pressure pulmonary edema, reintubation, and prolonged mechanical ventilation.6
- Some risks can be mitigated by maintaining deeper levels of anesthesia, avoidance of respiratory irritants, such as desflurane, and preoxygenation to increase oxygen (O2) reserves and decrease carbon monoxide (CO) levels.
Carbon Monoxide
- Smoking increases carboxyhemoglobin (COHgb) levels to 5-15% (normal 0.2 – 1.6%). CO has a 200-300 times affinity for hemoglobin (Hgb) relative to O2, decreasing O2 carrying capacity.6
- The binding of CO by Hgb decreases affinity for O2-binding (decreases P50), leading to a reduced release of O2 from Hgb to tissues (Figure 2).
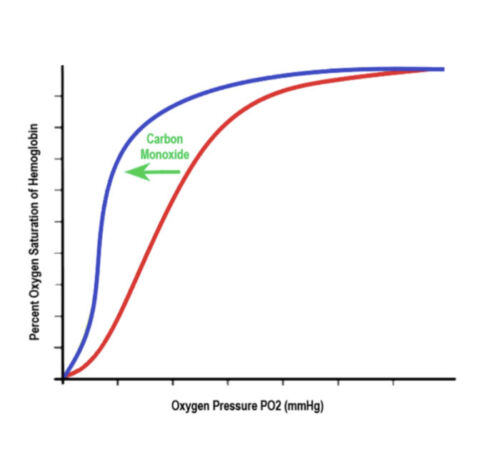
Figure 2. Oxygen Dissociation Curve. The binding of CO by Hgb decreases affinity for O2-binding (decreases P50), causing a leftward shift in the dissociation curve.
- CO binds to cytochrome oxidase and myoglobin, thereby inactivating cardiac mitochondrial enzymes, which decrease intracellular O2, thereby increasing hypoxia. CO hypoxia is not detected by pulse oximetry.5
- Tissue hypoxia causes decreased inotropy and increases in cardiac dysrhythmias (with COHb as little as 4-5%), necessitating close electrocardiographic monitoring.6
Hematopoietic System
- Chronic tissue hypoxia leads to a compensatory increase in red blood cell production and nonspecific myeloproliferation (white blood cells, platelets, and clotting factors), increasing plasma viscosity and a prothrombotic state.5,6
Wound and Bone Healing
- Reduced tissue perfusion and oxygenation increase the risks of delayed wound healing, dehiscence, and hernia (odds ratio 2.07), necrosis of wound and tissue (odds ratio 3.6), surgical site infection (odds ratio 1.18) (Table 1).4
- Bone healing is also impaired in smokers secondary to decreased neovascularization and osteoblast differentiation (odds ratio 2.32).4
Renal System
- Direct stimulation of the hypothalamo-neurohypophyseal axis causes increased antidiuretic hormone (ADH) levels, resulting in increased urine osmolality, decreased free water clearance, and dilutional hyponatremia, requiring avoidance of rapid correction when using intravenous fluids.6
Pharmacological Effects
- Polycyclic aromatic hydrocarbons from smoke inhalants induce cytochrome p450 and UDP-glucuronosyltransferase systems, thereby increasing the metabolism of opioids, benzodiazepines, propofol, most neuromuscular blockers, and volatile anesthetics.6
- These effects increase anesthetic requirements in smokers.
- Increased metabolism of volatile agents, along with the antiemetic properties of nicotine, may protect against postoperative nausea and vomiting.
Smoking Cessation
- An older prospective study showed increased pulmonary complication risk in patients with fewer than 8 weeks of smoking abstinence. However, recent systemic reviews and meta-analyses have not shown worse outcomes. With no strong evidence of harm related to short-term smoking abstinence, the Society for Perioperative Assessment and Quality Improvement (SPAQI) and the American Society of Anesthesiologists (ASA) Taskforce strongly recommend that patients be advised to quit smoking as soon as possible irrespective of surgery timing. A longer duration (more than 4-8 weeks) of smoking abstinence is optimal.7
- Smoking cessation reduces the risks of respiratory and wound-healing complications, and the benefits increase with longer periods of preoperative abstinence4,5,7 (Table 2).
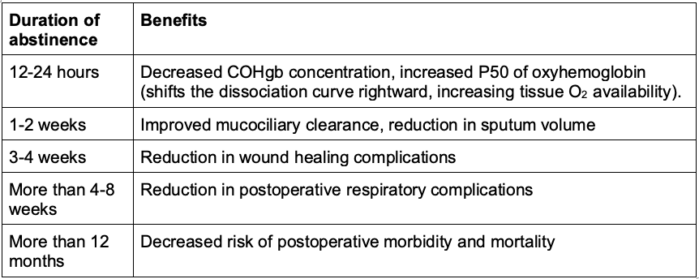
Table 2. Benefits of smoking cessation.
- Long-term smoking cessation reduces mortality rates with the greatest benefit in patients younger than 30 years of age. The risks of coronary artery disease and cerebrovascular disease approach the risk of never-smokers within 10-25 years.6
- The perioperative period is a “teachable moment” to encourage long-term smoking cessation, and the surgical encounter is associated with increased spontaneous smoking cessation compared with the rate in the general population.4
- Anesthesiologists should document preoperative cigarette smoking status, encourage smoking cessation, and, if time permits, refer patients to smoking cessation services to obtain counseling and pharmacologic interventions (Table 3).7 The ASA and SPAQI recommend the approach: Address, Advice, and Refer or Connect (AAR/AAC).4,7
- Smoking cessation counseling longer than 3 minutes is a billable service with associated Current Procedural Terminology (CPT®) codes.
- Counseling, behavioral therapy, and pharmacotherapy, in combination, are effective smoking cessation methods and increase the likelihood of long-term abstinence.4,7
- There are innovative and effective ways to educate and provide personalized counseling to aid smoking cessation: e-learning, web-based education, tobacco quitlines/text messaging systems, and in-person/virtual counseling.
- Current pharmacological interventions are listed in Table 4.
- Nicotine replacement therapies should be stopped 24 hours before surgery.
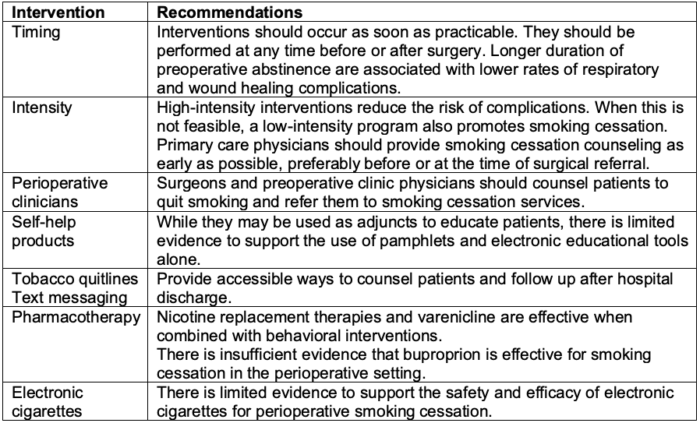
Table 3. Recommendations for perioperative smoking cessation interventions. Adapted from Wong J, et al. Society for Perioperative Assessment and Quality Improvement (SPAQI) consensus statement on perioperative smoking cessation. Anesth Analg. 2020.7
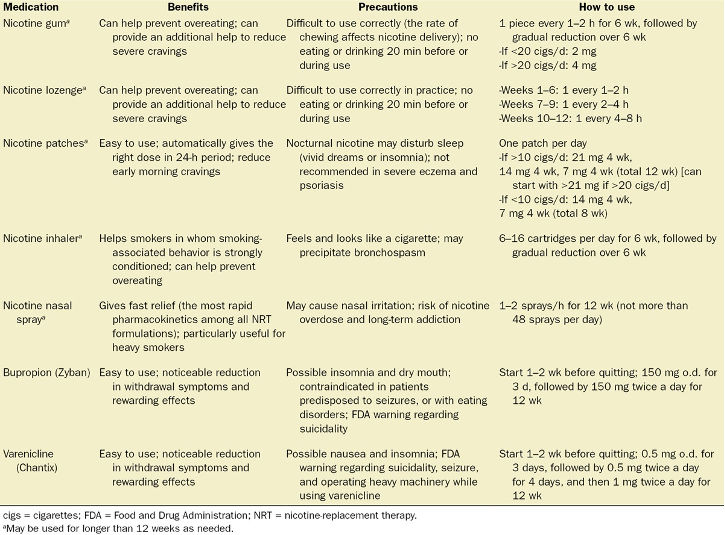
Table 4. Pharmacotherapies for smoking cessation. Used with permission from Yousefzadeh A, et al. Smoking cessation: The role of the anesthesiologist. Anesth Analg. 2016.4
References
- Centers for Disease Control and Prevention. Smoking and Tobacco Use. Accessed March 12th, 2023. Link
- United States Department of Health and Human Services. Smoking Cessation: A Report of the General Surgeon: Executive Summary. Atlanta, GA; United States Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2020. Link
- Benowitz NL. Nicotine addiction. N Engl J Med. 2010; 362(24): 2295-303. PubMed
- Yousefzadeh A, Chung F, Wong DT, et al. Smoking cessation: The role of the anesthesiologist. Anesth Analg. 2016;122 (5):1311-20. PubMed
- Rodrigo C. The effects of cigarette smoking on anesthesia. Anesth Prog. 2000;47(4):143-50. PubMed
- Carrick MA, Robson JM, Thomas C. Smoking and anaesthesia. BJA Educ. 2019;19 (1):1-6. PubMed
- Wong J, An D, Urman RD, et al. Society for Perioperative Assessment and Quality Improvement (SPAQI) consensus statement on perioperative smoking cessation. Anesth Analg. 2020;131(3): 955-68. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.