Copy link
Noninvasive Blood Pressure Monitoring
Last updated: 01/26/2024
Key Points
- Serial blood pressure monitoring is indicated in every patient receiving anesthesia. Invasive and noninvasive measurements each have intrinsic benefits and risks that should be weighed on a case-by-case basis.
- Several noninvasive methods of blood pressure measurement can be used to determine the patient’s systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial pressure (MAP). However, every method has shortcomings that should be carefully considered when being used to assess a patient.
- Auscultation of Korotkoff sounds continues to be the gold standard for accurately measuring SBP and DBP. This method only estimates MAP and may be difficult to accurately assess in hypotensive patients or noisy environments.
- Automated blood pressure cuff readings will measure lower values when the arm is raised above the level of the heart and higher values when the arm is lowered below the level of the heart.
Blood Pressure Measurement: Invasive vs. Noninvasive
- Noninvasive blood pressure monitoring:
- Indications: Per the American Society of Anesthesiologists guidelines, “Every patient receiving anesthesia shall have arterial blood pressure…determined and evaluated at least every five minutes”.1
- Contraindications: conditions in which repeated mechanical compression may cause traumatic injury (local bone fracture), open wounds to areas the cuff is intended to cover, presence of arteriovenous dialysis fistula, and indwelling peripherally inserted central lines.2 Automated blood pressure cuffs require pulsatile blood flow, making them inaccurate in cases requiring cardiopulmonary bypass and in patients with ventricular assist devices (VAD).3
- Complications: pain, petechiae and ecchymoses, limb edema, venous stasis and thrombophlebitis, peripheral neuropathy, and compartment syndrome
- Patients who have undergone axillary lymph node dissection were thought to be at an increased risk of lymphedema if blood pressure was repeatedly measured on the ipsilateral arm. However, these reports have been mostly anecdotal, and a large prospective cohort study showed no increase in lymphedema associated with blood pressure cuff usage.4,5
- Invasive blood pressure monitoring:
- Indications: anticipated rapid changes or extremes of blood pressure, patient inability to tolerate brief hemodynamic instability, and need for frequent blood sampling to assess respiratory function, oxygenation, ventilation, or metabolic derangements
- Contraindications: ongoing limb ischemia, local infection, or compromised collateral arterial supply (e.g., Raynaud phenomenon, thromboangiitis obliterans)3
- Complications: limb ischemia, hemorrhage, thrombosis, embolism, aneurysm or fistula formation, skin necrosis, and infection2
Noninvasive BP: Measurement Techniques
- Palpation
- SBP can be determined by palpating a peripheral pulse, inflating a blood pressure cuff proximal to the location until the flow is occluded, releasing cuff pressure slowly (2-3 mmHg per heartbeat), and finally measuring the cuff pressure at which the pulse is first felt again.
- Limitations of this method include no DBP or MAP measured and underestimation of SBP.
- Doppler
- A Doppler probe transmits an ultrasonic high-frequency sound across the lumen of an artery and may be substituted for the physician’s finger in the prior method to measure blood pressure.
- A shift in sound frequency (the Doppler effect) is produced by the movement of blood as pressure is released from an inflated blood pressure cuff.
- The inflation pressure at which flow is detected can reliably determine the SBP.
- Limitations of this method include no diastolic pressure or MAP measured.
- Auscultation
- Korotkoff sounds are frequencies created by turbulent flow within an artery caused by partial vessel compression by a blood pressure cuff. These sounds can be heard with the aid of a stethoscope over an artery as pressure is released from an inflated cuff.
- The pressure at which the first Korotkoff sounds are heard corresponds with the SBP.
- The pressure at which the muffling or loss of sound can be recorded as the DBP.
- This method is best used to measure the SBP and DBP but is unable to measure the MAP directly.
- Measurement of the SBP and DBP can then be used to estimate the MAP with the equation:
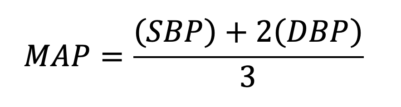
- Oscillometry:
- An automated blood pressure cuff is inflated until a pressure is reached, which occludes arterial flow to the limb. Pressure is then slowly released, and small fluctuations in cuff pressure are closely monitored by the machine.
- At first, the machine will only detect the pulseless decrease in pressure. However, as pressure is decreased below SBP, arterial flow resumes, which produces a detectable vibration of the arterial wall. This vibration produces oscillating changes in cuff pressure, which are measured by the computer.6
- As the cuff pressure is decreased to SBP and then further decreased to DBP, the frequency of oscillations increases and then decreases as flow through the vessel eventually becomes smooth, producing no oscillations in cuff pressure. These changes in oscillatory frequency roughly correlate with Korotkoff sounds heard with manual auscultation (see Figure 1).
- From these measurements, the point of maximal oscillation is measured as the MAP.
- SBP and DBP are estimated using proprietary algorithms that vary by manufacturer.7,8
- As SBP and DBP are not directly measured, they are therefore deemed to be less reliable than the MAP.3
- A comparison of oscillometric and direct arterial blood pressure measurements have shown that oscillometric blood pressure cuffs will often underestimate SBP and overestimate DBP. They also tend to underestimate values during periods of hypertension and overestimate during periods of hypotension.9
- This discrepancy in measurement may lead to a significant underestimation of pulse pressure.3
- DBP is the least accurate value measured by oscillometry, as this value is estimated using the minimum cuff pressure at which pressure fluctuations can be perceived. This value is difficult to measure as oscillations can still be present, even when the cuff is below the actual DBP.2
- Adequate blood pressure cuff sizing is important for accurate measurement.
- Blood pressure cuffs should have a bladder that extends to 40% of the arm circumference and 80% (or 2/3) of the distance between the elbow and shoulder.3
- Blood pressure measurements may be inaccurate in patients with any motion (shivering, tremors, seizure, etc.), severe hypotension, arrhythmias (e.g., atrial fibrillation), or mechanical disruption of the cuff or tubing.10
- In addition to the previously noted automated (oscillometric) measurement techniques, palpation and auscultation also require pulsatile blood flow to measure the components of blood pressure. Therefore, these methods are inaccurate in the measurement of blood pressure for patients on cardiopulmonary bypass (CPB) and those primarily dependent on VADs, which produce nonpulsatile flow.3
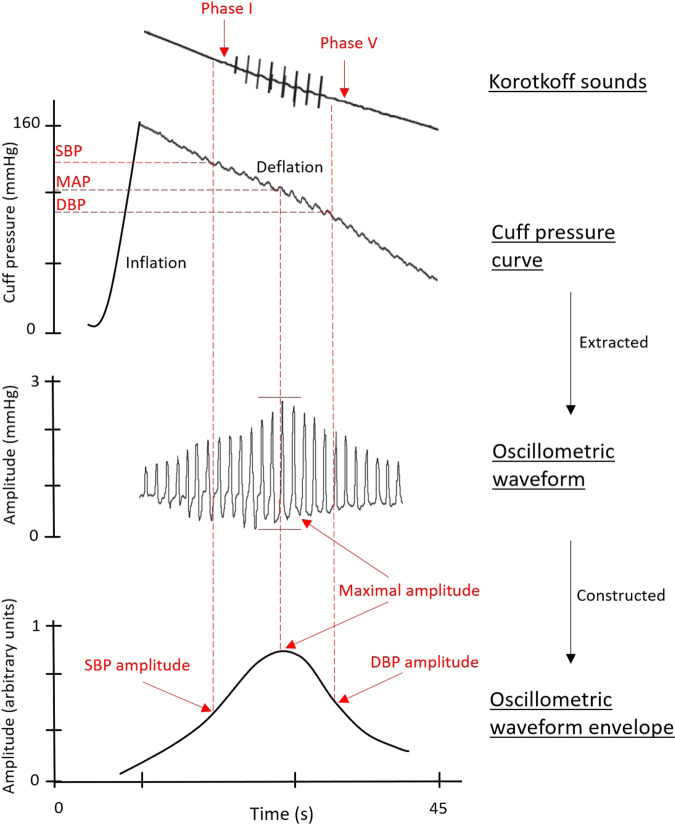
Figure 1. Overview of the oscillometric method to estimate blood pressure with superimposed examples of Korotkoff sounds phases I through V. Source: Sharman JE, et al. Automated ‘oscillometric’ blood pressure measuring devices: How they work and what they measure. J Hum Hypertens. 2022;37(2):93-100.
** Measured parameter is listed in parentheses.
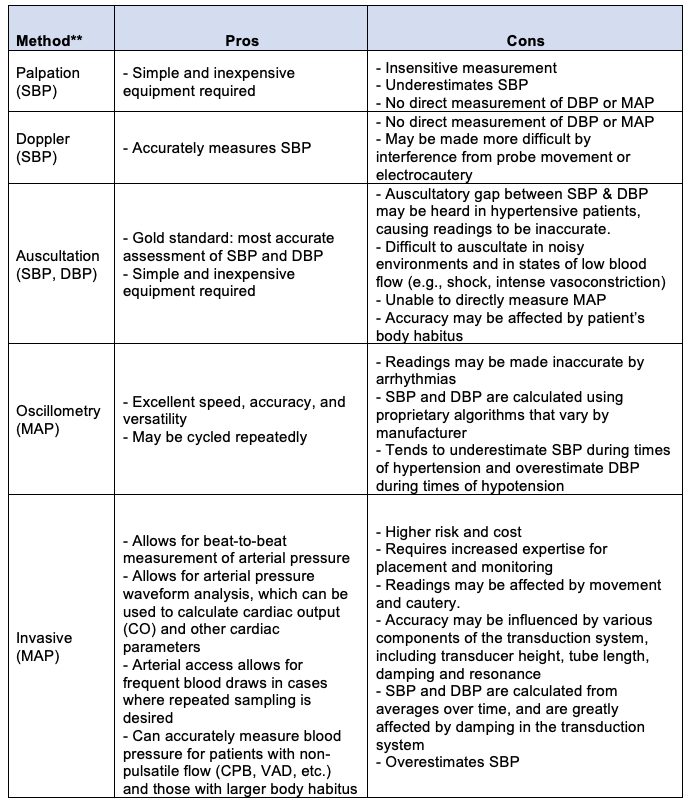
Table 1. Summary of the various methods of blood pressure measurement, directly measured hemodynamic parameters for each method, and pros/cons of each method.
Noninvasive Blood Pressure (NIBP): Positioning Effects
- Automated blood pressure cuff readings change depending on the relative position of the cuff to the patient’s heart.
- Elevation of the arm above the level of the heart results in lower blood pressure readings while lowering the arm below the heart causes the readings to be higher11 (Figure 2).
- The difference in blood pressure can be calculated by using the conversion 1 cm = 0.74 mm Hg or 10 cm in height = 7.4 mm Hg. Occasionally, it is easier to simplify the value as 20 cm = 15 (14.7) mmHg.
- Example: If a patient with a blood pressure of 120/80 has the cuff elevated 20 cm above the level of the heart, there will be a 14.7 mmHg difference in measured blood pressure values. Therefore, the automated cuff value will read closer to 105/63.
- This phenomenon may result in significant clinical implications, as an erroneously low blood pressure reading may lead to incorrect treatment of perceived hypotension.
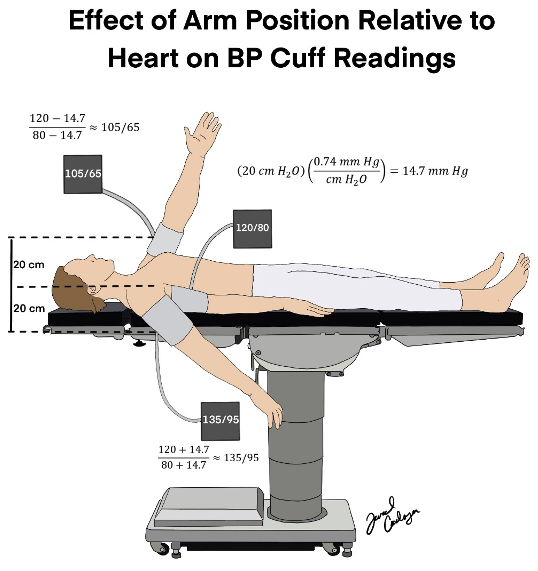
Figure 2. The difference in blood pressure (measured in mmHg) at three different heights: at the level of the heart, 20 cm above the heart, and 20 cm below the heart. The difference in blood pressure is calculated by multiplying the height difference (cm) by 0.74.
References
- American Society of Anesthesiologists. Standards for Basic Anesthetic Monitoring. Published October 20, 2010. Accessed April 25, 2023. Link
- Connor CW, Conley CM. Commonly used monitoring techniques. In: Clinical Anesthesia. 8th edition. Philadelphia, PA. Wolters Kluwer; 2017:715-6.
- Miller RD, Schroeder B, Barbeito A, et al. Cardiovascular monitoring. In: Miller's Anesthesia. 8th ed. Philadelphia, PA: Elsevier Saunders; 2015:1569-1629.
- Ferguson CM, Swaroop MN, Horick N, et al. Impact of ipsilateral blood draws, injections, blood pressure measurements, and air travel on the risk of lymphedema for patients treated for breast cancer. J Clin Oncol. 2016;34(7):691-8. PubMed
- Bryant JR, Hajjar RT, Lumley C, et al. Clinical Inquiry in women who have undergone breast cancer surgery, including lymph node removal, do blood pressure measurements taken in the ipsilateral arm increase the risk of lymphedema? J Okla State Med Assoc. 2016;109(12):589-91. PubMed
- Lewis PS. Oscillometric measurement of blood pressure: A simplified explanation. A technical note on behalf of the British and Irish Hypertension Society. J Hum Hypertens. 2019;33(5):349-51. PubMed
- Sharman JE, Tan I, Stergiou GS, et al. Automated ‘oscillometric’ blood pressure measuring devices: How they work and what they measure. J Hum Hypertens. 2022;37(2):93-100. PubMed
- Kaufmann MA, Pargger H, Drop LJ. Oscillometric blood pressure measurements by different devices are not interchangeable. Anesth Analg. 1996;82(2):377-81. PubMed
- Wax DB, Lin H-M, Leibowitz AB. Invasive and concomitant noninvasive intraoperative blood pressure monitoring. Anesthesiology. 2011;115(5):973-8. PubMed
- Kallioinen N, Hill A, Horswill MS, et al. Sources of inaccuracy in the measurement of adult patients’ resting blood pressure in clinical settings. J Hypertens. 2017;35(3):421-41. PubMed
- Mitchell PL, Parlin RW, Blackburn H. Effect of vertical displacement of the arm on indirect blood-pressure measurement. N Engl J Med.1964;271(2):72-4. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.