Copy link
Total Knee Arthroplasty: Regional Anesthesia Techniques
Last updated: 01/12/2024
Key Points
- Total knee arthroplasty (TKA) is a commonly performed procedure, with its demand expected to increase to over 1 million procedures by the year 2030. Over the last decade, TKAs have shifted toward outpatient surgery. Postoperative pain control among TKA patients continues to be an area for improvement.
- In the last decade, there has been a steady shift toward outpatient surgery. In 2018, the United States Center for Medicare & Medicaid Services finalized the 2018 Medicare Outpatient Payment System rule that removed TKA from the Medicare inpatient-only list of procedures.
- In the last decade, there has been a steady shift toward outpatient surgery. In 2018, the United States Center for Medicare & Medicaid Services finalized the 2018 Medicare Outpatient Payment System rule that removed TKA from the Medicare inpatient-only list of procedures.
- In addition to optimizing pain control, the other important consideration is providing analgesia while preserving motor function to facilitate immediate postoperative participation in physical therapy.
Background
- TKA is commonly performed to treat end-stage osteoarthritis and other disabling knee conditions, and its demand is expected to increase to over 1 million procedures in the United States by the year 2030.
- In the last decade, there has been a steady shift toward outpatient surgery. In 2018, the United States Center for Medicare & Medicaid Services finalized the 2018 Medicare Outpatient Payment System rule that removed TKA from the Medicare inpatient-only list of procedures.
- Altogether, the safety and general feasibility of cost-effective strategies across different TKA patient populations constitutes an area of increased interest and value. One of the facets that continues to require improvement is the high incidence of postoperative severe pain, ranging from 10 to 36%, which produces dissatisfaction and increased hospital utilization.1
- In addition to optimizing pain control, the other important consideration is providing analgesia while preserving motor function to facilitate immediate postoperative participation in physical therapy.
General vs. Neuraxial Anesthesia
- A large 2019 meta-analysis named the International Consensus on Anesthesia-Related Outcomes after Surgery group (ICAROS) analyzed 94 studies comparing neuraxial anesthesia (NA) vs general anesthesia (GA) in hip and knee arthroplasty.2
- NA was associated with improved outcomes compared to GA alone with respect to complications such as pulmonary complications, gastrointestinal complications, acute renal failure, deep vein thrombosis, pulmonary embolism, all-cause infections, superficial wound infections, blood transfusions, critical care admissions, and readmissions.2
Motor Sparing Blocks
Adductor Canal Block3,4
- Goals: local anesthetic spread around the femoral nerve in the femoral triangle or saphenous nerve in the adductor canal
- Innervation: Targets 2 terminal branches of the femoral nerve that innervate the anteromedial knee: nerve to vastus medialis and saphenous nerve. Although an adductor canal block is predominantly a sensory block, a large volume of local anesthetic in the subsartorial space may lead to proximal extravasation of local anesthetic into the femoral triangle, leading to potential quadricep weakness.
- Landmark and positioning: Ultrasound probe is placed in the middle-third of the medial thigh. Patient is supine with thigh abducted and externally rotated (Figure 1).
- Equipment and drugs: A linear transducer (8-14MHz) or curved transducer is used for larger patients. Typically, an 8cm 22–25-gauge needle is used and 10mL of 0.25% bupivacaine or 0.2% ropivacaine is injected.
- Anatomy
- Femoral triangle
- Roof – sartorius muscle
- Apex is the intersection between the medial borders of the sartorius and adductor longus muscle. The apex defines the proximal end of the adductor canal.
- Adductor canal / Subsartorius canal
- Contains the saphenous nerve and femoral artery
- Roof – sartorius muscle
- Anterolateral border – vastus medialis muscle
- Posteromedial border – adductor longus and adductor magnus muscles
- Contains the saphenous nerve and femoral artery
- Femoral triangle
- Femoral triangle injection provides better analgesia to the knee. An adductor canal injection blocks primarily the saphenous nerve.
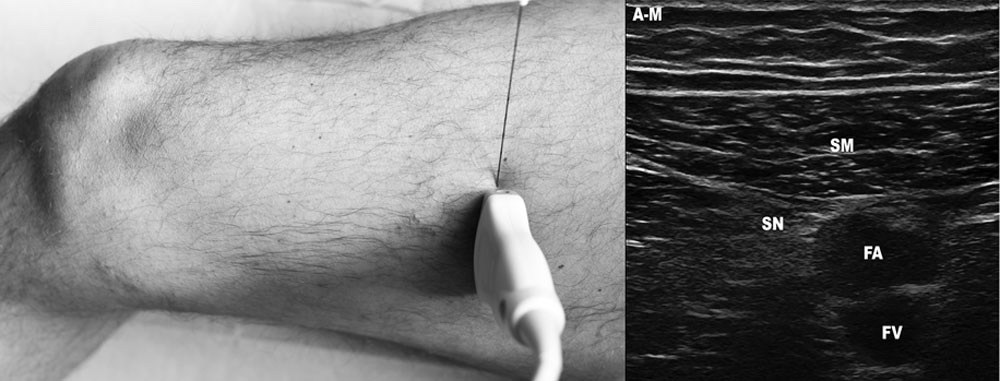
Figure 1. Patient and transducer position with needle insertion for ultrasound-guided adductor canal block.
Abbreviations: A-M = antero-medial; SM = sartorius muscle; SN = saphenous nerve; FA = femoral artery; FV = femoral vein.
Used with permission from Gautier PE, et al. Anesth Analg. 2016; 122(1): 279-82.
- Technique: The transducer is placed on the middle-third of the medial thigh (roughly midpoint from patella and iliac crest) and the dark, hyperechoic femur is identified. Once identified, the next step is to scan medially over the thigh to identify the femoral vessels deep to the sartorius muscle where its medial border meets the medial border of the adductor longus muscle. This point is known as the apex of the femoral triangle or the superior limit of the adductor canal. Needle insertion is made in-plane through the sartorius muscle to reach the adductor canal lateral to the femoral artery.
- Video: Gadsden J. Adductor canal block: What nerves are we after? Duke Regional Anesthesiology and Acute Pain Medicine. Link
IPACK Block (Infiltration [between] Popliteal Artery and Capsule of the Knee)
- Goals and indications: Local anesthetic infiltration over the posterior aspect of the femur between the popliteal artery and capsule of the knee for pain control after TKA, anterior cruciate ligament (ACL) repair, and procedures involving the posterior knee
- Innervation: Small articular branches of the popliteal plexus and obturator nerve resulting in analgesia to the posterior knee capsule with some distribution to the anterolateral knee capsule (articular branches of the sciatic nerve)
- Landmark and positioning: Epicondyles of the femur and the popliteal artery within the popliteal fossa. The patient can either be positioned supine with knee flexed, lateral decubitus, or prone. The needle may be inserted from lateral to medial or medial to lateral.
- Equipment and drugs: A linear transducer (or curved transducer for larger patients) is used. Typically, an 8 cm 22-gauge needle is used and 20mL of 0.25% bupivacaine or 0.2% ropivacaine is injected. This is considered a field block, hence the higher volume.
- Technique: In the supine position, the patient is asked to bend their knee by 45 degrees while internally rotating the hip. With the transducer in the popliteal crease, the popliteal artery and the 2 condyles of the femur (which look like hyperechoic humps) are identified. The next step is to scan slightly proximally until the epicondyles (humps) transition to a flatter metaphysis of the femur. While visualizing the popliteal vessels in relation to the femur, the needle is advanced in-plane from medial (or lateral) between the popliteal artery and the femur, and local anesthetic is injected along the posterior capsule of the knee.
- Video: Gadsden J. iPACK block. Duke Regional Anesthesiology and Acute Pain Medicine. Link
Genicular Nerve (GN) Blocks
- Goal and indications: Classically used for treating chronic knee pain via local anesthetic infiltration or radiofrequency ablation. Used as an adjunct with IPACK and adductor canal block. These blocks are simple and quick to perform.
- Innervation: Superomedial (SMGN), superolateral (SLGN), inferomedial (IMGN), and nerve to vastus intermedius
- Landmark and positioning: Bony surface of distal femoral condyle, proximal tibial condyle, and patellar borders. The patient is supine with the leg in a neutral position.
- Equipment: A linear transducer and a 5cm, 22-gauge needle is used. Typically, 5 mL of 0.25% bupivacaine or 0.2% ropivacaine is used per injection site, for a total of 20 mL local anesthetic. This is considered a field block. Historically, the block was performed by palpation and anatomic landmarks without ultrasound-guidance.
- Technique: The transducer is placed on the bony surface of the distal femur and in a sagittal orientation, the transducer is advanced towards the joint until a slight sloping of the epicondyle is seen. For SMGN and SLGN, the centerline of the probe will align with the superior aspect of the patella (medial and lateral, respectively). The needle is inserted in out-of-plane or in-plane view until bony contact is made. For the IMGN, transducer is maintained in the sagittal orientation with the centerline of the probe aligning 1-2cm distal to the joint line described as a “shallow bowl.” Lastly, this block may include the nerve to vastus intermedius. The transducer is placed approximately 3 cm superior to the patella with the femur visualized in short axis. The needle is advanced out-of-plane in similar fashion as above until bony contact is made. Inferolateral GN is avoided due to the risk of peroneal nerve blockade resulting in a foot drop.
- Video: Gadsden J. Ultrasound-guided genicular nerve blocks. Duke Regional Anesthesiology and Acute Pain Medicine. Link
Nonmotor Sparing Blocks
Femoral Nerve Block5
- Goals and indications: Local anesthetic spread around the femoral nerve for TKA, Fulkerson osteotomy, ACL repair
- Innervation: Anterior and medial thigh, including the hip, knee, and ankle joints with variable coverage to the medial leg down to the midfoot (saphenous nerve branch)
- Landmark and positioning: Femoral crease over the pulse of the femoral artery. The patient is supine with the leg extended and slightly externally rotated.
- Equipment and drugs: A linear or curved transducer if larger patient; 5cm-10cm, 22-gauge needle; 0.25% bupivacaine or 0.2%-0.3% ropivacaine, total volume 10-15mL
- Technique: The transducer is placed in an axial-oblique orientation parallel to the inguinal crease. The femoral nerve (lateral) and femoral artery (medial) are identified. Then, the fascia lata (superficial) and fascia iliaca (deep) that overlies the femoral nerve are identified. Injection of local anesthetic underneath the wrong fascia may result in block failure. The needle is inserted in a plane from lateral to medial and advanced towards the femoral nerve. The needle should be deep to fascia iliaca but superficial to the iliopsoas muscle. Hydrodissection is performed with either local anesthetic or normal saline until the solution is seen trickling over or under the femoral nerve.
- Video: Gadsden J. Femoral and lateral femoral cutaneous nerve blocks. Duke Regional Anesthesiology and Acute Pain Medicine. Link
Proximal Sciatic Nerve Block
- Goals and indications: Local anesthetic spread within the sciatic nerve sheath for procedures on and below the knee involving the posterior aspect of the knee and for above-knee amputation.
- Innervation: Sensory and motor block of the posterior aspect of the thigh and leg below the knee. Motor block involves all the posterior compartment muscles (biceps femoris, semimembranosus, and semitendinosus) and part of the adductor magnus muscles. Sensory block involves the posterior capsules of the hip and knee. Below the knee, the block results in complete anesthesia except for the saphenous nerve distribution in the medial leg (branch of femoral nerve), ankle, and foot.
- Landmark and positioning: Gluteal crease or sciatic nerve at the popliteal fossa with proximal scanning towards the subgluteal fold. The patient’s position can be prone, lateral decubitus, or supine with the procedure hip and knee in flexion.
- Equipment: A curvilinear or linear transducer probe if sub-gluteal/infragluteal approach is used. Typically, a 22-gauge, 8-10cm needle is used and 15-20 mL of 0.25% bupivacaine or 0.2% ropivacaine is used.
- Technique
- Subgluteal (infragluteal): The transducer is placed over the gluteal crease and the fascial planes between the gluteus maximus and quadratus femoris muscles are identified. The next step is to scan distally and adjust the tilt of the transducer to distinguish the sciatic nerve between those two muscles. The needle is advanced in-plane from lateral to medial toward the lateral edge of the sciatic nerve within the identified fascial plane, and local anesthetic is injected.
- Video: Gadsden J. Subgluteal sciatic nerve block. Duke Regional Anesthesiology and Acute Pain Medicine. Link
- Anterior: The transducer is placed in a transverse orientation over the anteromedial aspect of the proximal thigh. The femoral artery and nerve superficial and medial with the lesser trochanter in the lateral position is identified. The sciatic nerve is noted deep between the adductor magnus and semimembranosus/semitendinosus. If the patient can dorsi/plantar flex ankle, the nerve will be noted moving within the muscular plane, facilitating identification of the nerve. The needle is inserted in- or out-of-plane and advanced towards the fascial plane where the sciatic nerve is located. If the nerve is difficult to visualize, nerve stimulation is very helpful in identifying the sciatic nerve.
- Video: Gadsden J. Anterior sciatic nerve block. Duke Regional Anesthesiology and Acute Pain Medicine. Link
- Popliteal (Distal): The transducer is placed in a transverse position in the popliteal crease, and the pulsatile popliteal artery is identified. The tibial nerve typically lies superolaterally to the popliteal vein and can be seen as a hyperechoic, round structure with a honeycomb pattern. The next step is to scan more proximally until the peroneal nerve converging with the posterior tibial nerve is visualized. At this juncture, the needle is advanced in-plane from lateral to medial within the sciatic sheath. This block can also be performed while the patient is prone using an out-of-plane technique.
- Video: Gadsden J. Popliteal sciatic nerve block. Duke Regional Anesthesiology and Acute Pain Medicine. Link
References
- Rodriguez-Patarroyo FA, Cuello N, Molloy R, et al. A guide to regional analgesia for Total Knee Arthroplasty. EFORT Open Rev. 2021;6(12):1181-92. PubMed PubMed
- Memtsoudis SG, Cozowicz C, Bekeris J, et al. Peripheral nerve block anesthesia/analgesia for patients undergoing primary hip and knee arthroplasty: recommendations from the International Consensus on Anesthesia-Related Outcomes after Surgery (ICAROS) group based on a systematic review and meta-analysis of current literature. Reg Anesth Pain Med. 2021;46(11):971-85. PubMed
- Hadzic A, Minkowitz HS, Melson TI, et al. Liposome bupivacaine femoral nerve block for postsurgical analgesia after total knee arthroplasty. Anesthesiology 2016; 124:1372–83. PubMed
- Bendsten TF, Lopez AM, Clark TB. Ultrasound-guided saphenous (subsartorius/adductor canal) nerve block. In: Hadzic's Textbook of Regional Anesthesia and Acute Pain Management. New York, NY: McGraw-Hill Education; 2017:615-9.
- Hadzic A. Saphenous nerve block. In: NYSORA Nerve Block Manual. New York, NY: NYSORA, Inc; 2022:134-9.
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.