Copy link
Hydrocephalus and Chronic Intracranial Hypertension
Last updated: 01/12/2023
Key Points
- Hydrocephalus is the pathological accumulation of cerebrospinal fluid (CSF) in the cerebral ventricles and is the most common cause of chronic intracranial hypertension (ICH).
- Hydrocephalus is classified as communicating, noncommunicating, hypersecretory, and normal pressure hydrocephalus.
- Pseudotumor cerebri is also known as idiopathic intracranial hypertension.
Cerebral Spinal Fluid Physiology
- CSF is produced by the ependymal cells in the choroid plexus of the lateral, third and fourth ventricles. In adults, about 400 – 600 mL of CSF is produced every day, and there is about 150cc of CSF at any given time (1.5-2cc/kg)(Figure 1).1
- CSF covers the brain and the spinal cord in the subarachnoid space.
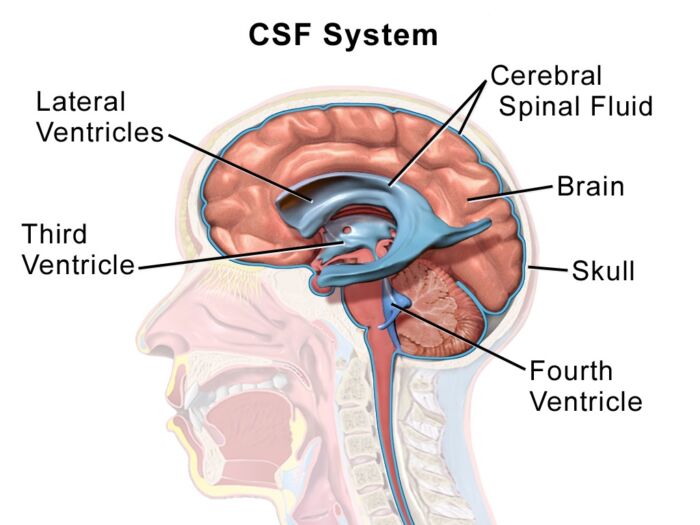
Figure 1. CSF in the cerebral ventricles and subarachnoid space. Source: Wikipedia. Medical Gallery of Blausen Medical 2014. CC BY 3.0.
- Circulation of CSF: lateral ventricles ➔ interventricular foramina ➔ 3rd ventricle ➔ cerebral aqueduct ➔ 4th ventricle ➔ subarachnoid space via 4 openings in 4th ventricle (central canal, median aperture, lateral aperture, lateral aperture)(Figure 2).1
- CSF is re-absorbed by the arachnoid granulations and drained into the dural venous sinuses. Arachnoid granulations are outpouchings of arachnoid mater into the sinuses with one-way valves.1
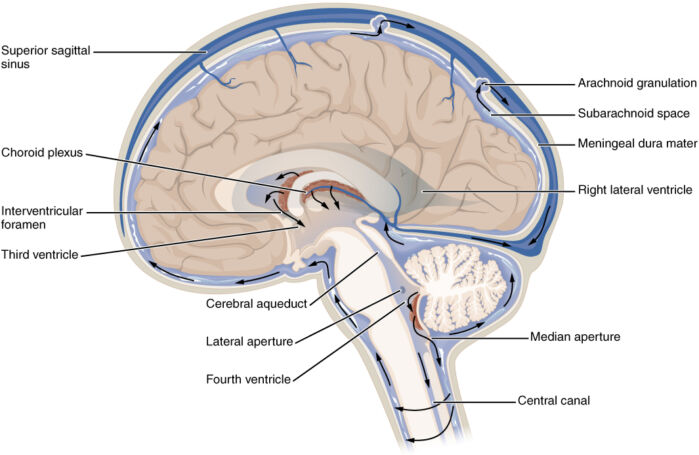
Figure 2. Circulation of CSF. Source: OpenStax. Wikipedia. CC BY 4.0
Hydrocephalus Classification
- Hydrocephalus refers to the pathological accumulation of CSF in the cerebral ventricles. In adults, the 4 types of hydrocephalus are communicating, noncommunicating, hypersecretory, and normal-pressure hydrocephalus.3 Congenital hydrocephalus presents in young children with increased head size, bulging fontanelles, setting-sun sign (pupils closed to the lower eyelid), poor feeding, etc.2
- Communicating hydrocephalus2
- It is caused by impaired absorption of CSF.
- There is still communication or flow between the CSF within and between the ventricles.
- Most common causes are subarachnoid hemorrhage and meningitis.
- Noncommunicating hydrocephalus2
- CSF flow is blocked along one of the passages connecting or within the ventricles.
- There is no CSF communication or flow between the ventricles.
- Commonly caused by tumors such as ependymomas, astrocytomas, craniopharyngiomas, posterior fossa tumors, etc.
- Hypersecretory hydrocephalus:2
- It is caused by an overproduction of CSF, most commonly due to plexus papillomas.
- It is more common in children.
- Normal pressure hydrocephalus (see below)
Normal Pressure Hydrocephalus
- Normal pressure hydrocephalus (NPH) is a type of communicating hydrocephalus characterized by increased ventricular size with normal opening pressures on lumbar puncture (LP).3
- NPH primarily affects people older than 50 years, with a gradual onset.
- The enlargement of the ventricles compresses the brain parenchyma causing the classic triad of cognitive impairment, gait disturbances, and urinary incontinence/urgency.3
- MRI is superior to computed tomography to diagnose NPH. Signs on MRI include ventriculomegaly without sulcal enlargement or obstruction at the 3rd or 4th ventricle, loss of signal in aqueduct of Sylvius.3
- Diagnosis of NPH can be confirmed in two ways:
- a high-volume LP, where 30-50 mL of CSF is removed, and the patient is monitored for gait and symptomatic improvement;3
- a lumbar drain trial, where a lumbar drain is placed to continuously drain CSF, and the patient is monitored for gait and symptomatic improvement.3
- NPH is commonly treated by placing a ventricular shunt, frequently from the lateral ventricle to the abdominal peritoneal space. In certain cases, the neurosurgeon can also treat NPH with an endoscopic third ventriculostomy or choroid plexus coagulation.3
Pseudotumor Cerebri
- Also known as idiopathic intracranial hypertension.
- Primarily affects overweight females of child-bearing age group.
- Pseudotumor cerebri is a diagnosis of exclusion characterized by clinical signs and symptoms of increased intracranial pressure, normal CSF composition, and no other causes of ICH on neuroimaging.4
- Clinical symptoms include headache, transient visual symptoms, pulsatile tinnitus, back pain, and retrobulbar pain.4
- Physical exam findings include papilledema, visual field deficits, and sixth nerve palsy.4
- Vision loss is the most serious complication.
- Treatment includes acetazolamide, weight loss, and a low-salt diet.5,6 Acetazolamide is a carbonic anhydrase inhibitor that decreases CSF production. One can also consider topiramate and furosemide.5 When visual loss is severe or rapidly progressive, surgical interventions such as optic nerve sheath fenestration or CSF shunting may be needed.5,6
References
- Butterworth JF., et al. Neurophysiology & Anesthesia. In: Morgan and Mikhail’s Clinical Anesthesiology. Sixth edition. New York; McGraw Hill Education; 2018: 583-589.
- Koleva, M, De Jesus O. Hydrocephalus. 2021. In: StatPearls. Treasure Island (FL). StatPearls Publishing; 2022. Link
- Graff-Radford NR. Normal Pressure Hydrocephalus. In: DeKosky ST, ed. UpToDate. 2021. Link
- Lee AG, Wall M. Idiopathic Intracranial Hypertension (Pseudotumor Cerebri): Clinical Features and Diagnosis. In: Brazis PW, ed. UpToDate. 2021. Link
- Wall M, Lee AG. Idiopathic Intracranial Hypertension (Pseudotumor Cerebri): Prognosis and Treatment. In: Trobe J Swanson JW, ed. UpToDate. 2021. Link
- Thurtell MJ, Wall M. Idiopathic Intracranial Hypertension (Pseudotumor Cerebri): Recognition, Treatment, and Ongoing Management. Curr Treat Options Neurol. 2013;15(1):1-12. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.