Copy link
Pharmacological Changes with Aging: Opioids and Neuromuscular Blocking Agents
Last updated: 01/27/2023
Key Points
- Elderly patients exhibit increased pharmacokinetic and pharmacodynamic variability with opioid administration. This results in an increased incidence of adverse drug reactions. Thus, elderly patients require more careful titration of opioids and therapeutic drug monitoring.
- Although differences in pharmacokinetics influence the onset of effect and duration of action of neuromuscular blocking agents, the ED95 is not statistically different in elderly patients compared to young adults.
- Residual neuromuscular blockade appears to be more frequent in elderly patients when compared to young adults.
Pharmacological Changes With Aging: Opioids
Caution must be used when administering opioids to elderly patients secondary to the risk of respiratory depression, which has been noted to be 2.8 times greater in the elderly when compared to young adults.1,2 Although the risk of respiratory depression may be greater in older patients, this is not true for all opioid side effects. While opioids are among the major causes of postoperative nausea and vomiting, increasing age may actually decrease the risk of nausea and vomiting (Table 1).
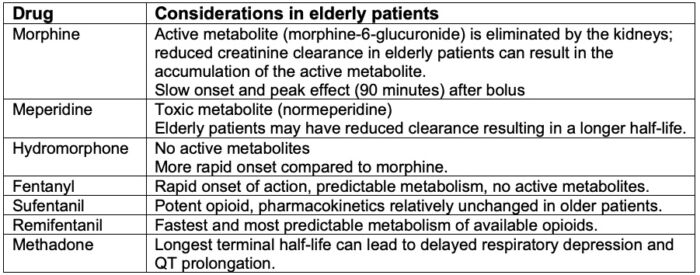
Table 1. Pharmacokinetic considerations for opioid use in elderly patients
Patient-Controlled Anesthesia (PCA)
PCA is an effective means to provide postoperative analgesia in elderly patients. Poor pain management places elderly patients at risk for confusion and postoperative delirium, which is associated with poor clinical outcomes. It should be emphasized that increased monitoring and individualization of dosage are essential in PCA management of elderly patients. Caution should be exercised when using a background infusion. It will take many hours to reach a steady state, which may expose elderly patients to toxicity 12-24 hours after initiation of the infusion.1
Conclusion
Opioids are used for balanced general anesthesia, as well as acute and chronic pain in elderly patients. Elderly patients need about half the dose of opioids compared to younger patients to achieve the same analgesic effect. Elderly patients have multiple factors that may place them at an increased risk for opioid toxicity, including increased pharmacologic variability, frequent polypharmacy, noncompliance with medication regimens, and impaired renal and hepatic function.1
Pharmacological Changes with Aging: Neuromuscular Blocking Agents
When initiating and maintaining paralysis in a geriatric patient, special consideration must be given to the potential for altered pharmacologic response to neuromuscular blocking agents (NMBAs).
Changes in Structure of the Neuromuscular Junction
In patients over 60, the neuromuscular junction undergoes continuous degeneration and regeneration. There is a reduction in the number of motor neurons in the spinal cord and ventral root fibers. This decrease in motor neurons is accompanied by a reduction in the number of motor units, consisting of a motor neuron and its innervated muscle fibers. An increase in the size of the motor unit partially compensates for the loss of motor units and results in an augmented twitch response when stimulating a single motor nerve in the geriatric population.1
Dose-Response Relationships in the Elderly
Several physiologic factors, with seemingly contradictory effects, play a role in the observed differences in onset of action and duration of NMBAs in geriatric patients. Loss of muscle mass should result in an upregulation of acetylcholine receptors and relative resistance to nondepolarizing NMBAs. However, decreases in lean body mass and volume of distribution would suggest that geriatric patients require decreased doses of NMBAs. Although differences in pharmacokinetics influence the onset of effect and duration of action, the dose of NMBAs that will generally produce 95% neuromuscular blockade (NMB) is the same in elderly and young adults.1
Onset of NMB
Onset of NMB is determined by the potency of the NMBA, and the time it takes the agent to reach the neuromuscular junction. The speed at which NMBAs are delivered to the neuromuscular junction is influenced by circulation to the muscles and cardiac output, which is frequently decreased in geriatric patients. Generally, a slower onset of NMB can be expected in the geriatric population.1
The slower onset of NMB in elderly patients may result in overdosing of NMBAs. To hasten the onset of effect, additional doses may be administered. The larger cumulative dose can result in an increased duration of action of the NMBA.
Pharmacokinetics and Duration of Action
Aging, even in healthy geriatric patients, is associated with decreased hepatic and renal blood flow and function. As most nondepolarizing NMBAs are eliminated through some combination of these means, alterations in the pharmacodynamics and duration of action should be expected (Table 2).
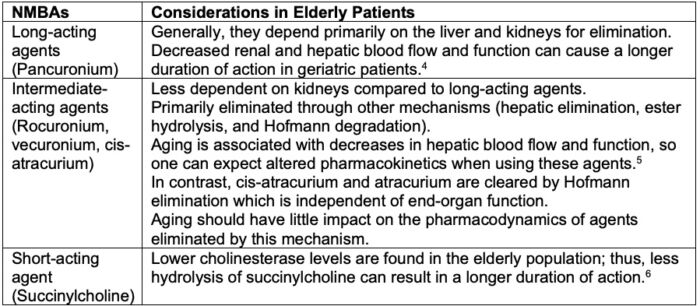
Table 2. Pharmacokinetic considerations with NMBAs in elderly patients
Postoperative Residual NMB
Residual NMB is a risk whenever a nondepolarizing NMBA is administered. While it occurs in both young and older patients, residual NMB appears to be more frequent in the elderly population. This occurs because of a combination of factors, including relative overdosing due to slower onset of effect, decreased clearance, decreased muscle mass, and increased variability in the duration of action of NMBAs.1
Neostigmine and Glycopyrrolate
The dose of neostigmine required for antagonism of residual NMB in the elderly is either similar to or greater than that of younger adults. The duration of action of neostigmine appears to be prolonged, which is potentially advantageous in the elderly, given that the duration of action of many nondepolarizing NMBAs is prolonged as well.
The cardiac muscarinic effects of neostigmine include dysrhythmias such as bradycardia and conduction defects. These can be exaggerated in elderly patients given their high prevalence of cardiovascular disease. Glycopyrrolate given to counteract these effects can frequently lead to tachycardia, which also may not be well tolerated in the elderly due to pre-existing cardiovascular disease. The increase in myocardial oxygen demand can lead to ischemia.1
Sugammadex
Sugammadex appears to reduce the incidence of incomplete recovery of muscle strength (residual paralysis) in the elderly population when compared to neostigmine and glycopyrrolate. Recovery to a train-of-four ratio more than 0.9 appears to take longer in the elderly following a dose of sugammadex. Also, clearance is expectedly decreased in the elderly due to decreased renal blood flow and function.1
Summary
Although age-related changes in hepatic, renal, and cardiac function slow the onset and clearance of many nondepolarizing NMBAs in geriatric patients, extensive changes at the neuromuscular junction do not increase the sensitivity to these compounds. Decreased clearance and alteration of pharmacodynamics in the elderly mandates that NMB be maintained and subsequent doses administered only after documentation of return of muscle strength with an NMB monitor.1
References
- Reves JG, Barnett SR, McSwain JR, Rooke GA, Geriatric Anesthesiology 3rd ed. Springer International Publishing, 2018.
- Cepeda MS, Farrar JT, Baumgarten M et al. Side effects of opioids during short-term administration: effect of age, gender, and race. Clin Pharmacol Ther. 2003; 74:102-12. PubMed
- Scott JC, Stanski DR. Decreased fentanyl/alfentanil dose requirement with increasing age: a pharmacodynamic basis. J Pharmacol Exp Ther 1987; 240:159-66. PubMed
- Duvaldestin P, Saada J, Berger JL, et al. Pharmacokinetics, Pharmacodynamics, and dose-response relationships of pancuronium in control and elderly subjects. Anesthesiology. 1982; 56:36-40. PubMed
- Matteo RS, Ornstein E, Schwartz AE et al. Pharmacokinetics and pharmacodynamics of rocuronium in elderly surgical patients. Anesth Analg. 1993; 77:1193-7. PubMed
- Lee LA, Athanassoglou V, Pandit JJ, Neuromuscular Blockade in the elderly patient. J Pain Res. 2016; 9: 437-444. PubMed
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.