Copy link
Neonatal Cardiovascular Physiology
Last updated: 04/04/2023
Key Points
- Neonatal cardiac output is heart rate-dependent due to a decreased ability to augment contractility and stroke volume.
- Anatomic or physiologic disturbances resulting in increased pulmonary vascular resistance can result in a return to fetal circulation.
- The presence of a shunt may impact the speed of induction in the pediatric patient.
Introduction
- Neonatal cardiovascular physiology is impacted by myocardial immaturity and the presence of a transitional circulation. At birth, the first breath initiates the transition away from fetal circulation. Lung inflation and an increase in PaO2 leads to decreased pulmonary vascular resistance (PVR) and increased pulmonary blood flow. Functional closure of the foramen ovale and ductus arteriosus typically occurs within the first 24-48 hours of life.1
- Persistent pulmonary hypertension as well as anatomic or physiologic disturbances that result in acidosis, hypoxemia, or hypercarbia lead to increased PVR and may result in persistent fetal circulation. Etiologies include sepsis, cyanotic congenital heart defect, or lung diseases such as congenital diaphragmatic hernia or meconium aspiration.1
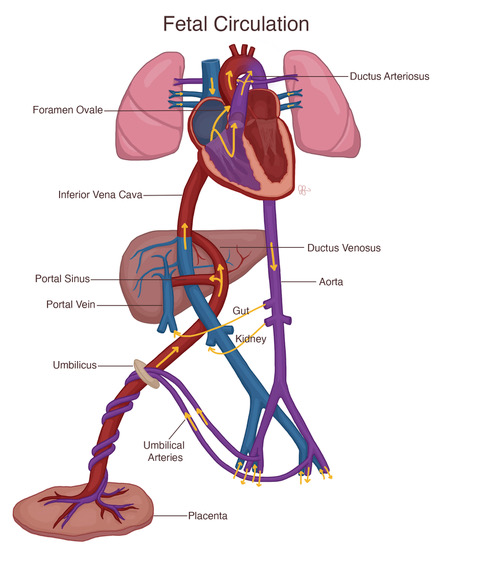
Figure 1. Fetal circulation. Source: Julie Fenske, MS, CCP (Reproduced with permission).
Neonatal Cardiovascular Physiology
- Up to six months of age, the neonate’s immature myocardium can result in a decreased ability to respond to hemodynamic changes.
Structural Characteristics1,2
- Neonatal myocardium is characterized by higher water-to-collagen and connective tissue-to-contractile tissue ratios. The immature myocyte has fewer myofibrils, and these myofibrils are less organized and evenly distributed throughout the cell.
- Neonatal myocardium has fewer, smaller, and morphologically immature mitochondria.
- Neonatal myocyte contractility is more dependent on plasma calcium due to an immature sarcoplasmic reticulum and poorly developed T-tubules.
- In the neonate, parasympathetic innervation is fully developed, whereas sympathetic innervation is incomplete. Responses to stimuli are often vagal in nature resulting in significant bradycardia.
Mechanics
- Compared to the adult heart, the neonatal heart is less compliant and approaches the flatter end of the Frank-Starling response curve. Clinically, this is relevant as the neonatal heart is at risk of overdistension by rapid volume increases, which could result in acute heart failure.1
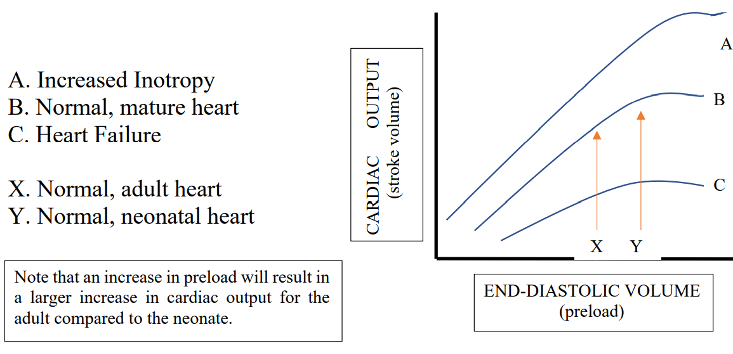
Figure 2. Cardiac output (CO) is determined by heart rate (HR) and stroke volume (SV) using the formula CO = HR x SV. As a result of the immature myocardium’s decreased ability to augment SV, the neonate’s CO is heart rate dependent.1
Electrophysiology
- At birth, the QRS axis is shifted downward and to the right, as the right ventricle is the dominant ventricle.3 As the left ventricle becomes more dominant, the QRS axis undergoes a leftward shift towards the adult axis.
Response to Vasoactive Medications
- Immediately following birth, there are high levels of circulating endogenous catecholamines that result in a decreased response to exogenous catecholamines.1
Normal Heart Rate (HR) and Blood Pressure (BP) for Age
- With age, the baseline HR is expected to decrease, and blood pressure is expected to increase. Baseline values may be different in patients with congenital heart disease and during awake versus sleeping states.1,4 Clinical decisions should be made with respect to the patient’s individual physiology.
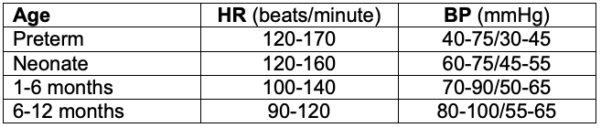
Table 1. Normal heart rate and blood pressure for age.
Anesthetic Considerations
Effect of Anesthetic Agents5
Volatile Agents
- Volatile anesthetics cause myocardial depression, and decreased sympathetic tone that lead to decreased cardiac output (CO) and BP.
- Immature myocardium is more sensitive to the myocardial depressant effects of volatile anesthetics, likely due to its age-related changes in intracellular calcium flux.2 This is most notable in neonates and infants younger than six months, in those with preexisting decreased ventricular function, and at high inspired volatile concentrations.
- Halothane has a greater depressant effect than other volatile anesthetics.
- The risk of myocardial depression with higher volatile concentrations is clinically significant in pediatric patients, given that minimum alveolar concentration (MAC) peaks at 6 months of age.6
Intravenous Agents
- Propofol inhibits the sympathetic nervous system and decreases vascular tone resulting in decreased BP. It can also cause myocardial depression at high doses.
- Etomidate is a hemodynamically stable induction medication with little to no effect on HR, contractility, or vascular tone.
- Benzodiazepines can lead to mild myocardial depression and decreased vascular tone, which is amplified when administered with opioids.
- Dexmedetomidine can result in bradycardia or heart block and should be used with caution in HR-dependent patients.
Speed of Induction
- In neonates, a greater proportion of the CO is delivered to vessel-rich organs, resulting in faster induction of anesthesia.
- Right-to-left shunting slows inhalational inductions, especially with less soluble agents such as sevoflurane, and may result in higher-than-expected arterial concentrations of IV medications.
- Theoretically, left-to-right shunting should speed inhalational inductions. However, this is not seen clinically.
Hemodynamic Support
- Neonates may have a decreased response to vasoactive medications due to high levels of circulating endogenous catecholamines. The choice of vasopressor should depend on the clinical situation and desired pharmacologic effect.1
- Painful stimuli (e.g. laryngoscopy, surgical stimulation, endotracheal suctioning) may cause bradycardia in the neonate and require anticholinergic administration.
- Increases in PVR should be avoided in order to prevent reversion to fetal circulation.
Volume Administration
- The less compliant neonatal heart is unable to accommodate rapid volume administration. Unlike in healthy adults, where volume administration can augment CO, neonates derive a lesser benefit and may be at risk for acute heart failure.1
- Volume overload is a risk factor for reopening of the ductus arteriosus and should be avoided.
References
- Andropoulos, DB. Physiology and cellular biology of the developing circulation. In: Andropoulos DB, Stayer SA, Mossad EB, Miller-Hance WC. Anesthesia for Congenital Heart Disease. 3rd ed. John Wiley & Sons, Incorporated; 2015: 84-105.
- Baum VC, Palmisano BW. The immature heart and anesthesia. Anesthesiology. 1997;87(6):1529-48. PubMed
- Pærregaard MM, Kock J, Pihl C, et al. The evolution of the neonatal QRS axis during the first four weeks of life. Neonatology. 2021;118(2):155-62. PubMed
- Sapra A, Malik A, Bhandari P. Vital sign assessment. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 PubMed
- Mazoit, JX. Pharmacology. In: Andropoulos DB, Gregory GA, eds. Gregory’s Pediatric Anesthesia. Sixth edition. Wiley Blackwell; 2020:191-225.
- Anderson BJ, Lerman J, Cote CJ. Pharmacokinetics and pharmacology of drugs used in children. In: Cote CJ, Lerman J, Anderson BJ (eds). A Practice of Anesthesia for Infants and Children. 6th edition. Philadelphia, PA. Elsevier. 2019: 100-176.
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.