Copy link
Tumescent Liposuction
Last updated: 05/24/2023
Key Points
- Liposuction techniques all involve the disruption of the fatty layer of tissue with the subsequent aspiration of fatty tissue. Tumescent liposuction and laser/ultrasound-assisted liposuction techniques are the most common methods of liposuction.2
- Potential complications of all types of liposuctions include local trauma, bleeding, violation of the abdominal or thoracic cavities, and hypothermia. Tumescent liposuction carries additional risks associated with infiltration of the fatty layer with lidocaine and epinephrine.2
- The maximum dose of tumescent lidocaine is up to 55 mg/kg.1,2 Higher total doses are tolerated due to the slowed uptake and, thus, lower peak concentrations of lidocaine.
- The risk of local anesthetic systemic toxicity (LAST) persists several hours after the procedure as serum lidocaine levels do not peak until 12-14 hours following the procedure.
Introduction
- Liposuction was first attempted in the 1920s but was not popularized until cannula liposuction was used in the 1960s. Initially, epinephrine was injected prior to the procedure to reduce blood loss, but general anesthesia was still required for analgesia.1
- In the 1980s tumescent liposuction was described as the use of an injectable solution of high-dose lidocaine with dilute epinephrine prior to the procedure. This technique obviated the need for general anesthesia.1
- True tumescent technique liposuction must occur with minimal sedation; if moderate sedation or deeper is administered, the technique is termed “semitumescent.”1
- Several factors must be considered when providing anesthesia during liposuction procedures: dosage of local anesthetics and the risk for systemic toxicity, patient temperature regulation, volume status, and potential trauma from the operation itself.2
Liposuction Basics and Patient Population
- Tumescent liposuction involves injecting a solution of epinephrine and lidocaine in isotonic crystalloid into the subcutaneous tissue prior to aspiration of fat1,2 (Figure 1).
- Vasoconstriction from dilute epinephrine (1:1,000,000 or 1mcg/cc) reduces procedural blood loss and slows the uptake of the local anesthetic, reducing peak plasma concentrations.1 Infiltration should occur at least 10 minutes prior to the procedure to allow for vasoconstriction to occur.2
- Low concentrations of lidocaine (0.1% or less) with dilute epinephrine has a prolonged duration of action and delayed serum peak concentration.1
- Tumescent solution is infiltrated subcutaneously 1:1 based on anticipated fat volume removal.2
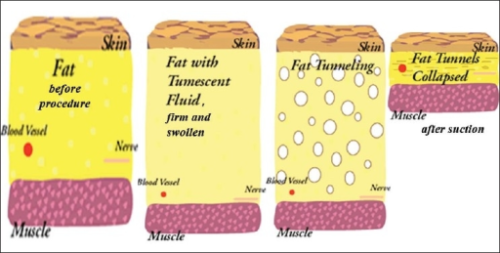
Figure 1. The principle of tumescent liposuction. Tumescent fluid is first injected into the subcutaneous tissue with resulting vasoconstriction of blood vessels. Fat tunneling is the process of removing fat with the suction catheter. Source: Venkataram J. Journal of Cutaneous and Aesthetic Surgery. 2008. Open i. CC BY 2.0. Link.

Figure 2. Example of liposuction cannula (top) and infiltration needle (bottom) Source: Loh CY, et al. Indian Journal of Plastic Surgery. 2013 Open i. CC BY-NC-SA 3.0. Link.
- Ultrasound and laser-assisted techniques both involve the application of energy to disrupt the fat tissue prior to aspiration.2
- Complications with ultrasound and laser techniques involve seroma formation, increased blood loss compared to tumescent liposuction due to a lack of epinephrine-mediated vasoconstriction, burns, and body-cavity perforation.
- Patient populations are 10:1 female:male, and the age ranges anywhere from teens to 70 years old.2
- Patient selection and preoperative evaluation should include consideration of cardiac, respiratory, hepatic, and renal function, along with an assessment of venous thromboembolism risk, coagulation disorders, and evaluation of medications that may impact the metabolism of lidocaine.
Potential Complications of Liposuction
- Tumescent liposuction (particularly with a ratio of infiltration to fat removal of 1:1 or more) has the potential for volume overload given the large amounts of solution injected into the subcutaneous tissue.4
- A foley catheter should be placed for fluid status monitoring and to prevent overdistention of the bladder in cases of large volume vascular uptake.2
- Caution should be used in patients with cardiac, renal, or hepatic dysfunction.
- Diuretics may be needed for patients who receive large volumes of tumescent solution.2
- The subcutaneously injected fluid is absorbed over 48 hours.
- Epinephrine levels peak 5-6 hours after the procedure.1
- Lidocaine levels peak 12-14 hours following the procedure.1
- Hypothermia may occur if tumescent solution is not warmed prior to injection. Active warming of the patient is usually necessary and body temperature monitoring should be performed.4
- Other risks include fat embolism and pulmonary embolism.
- Sequential compression devices should be utilized to prevent venous stasis.2
- Anticoagulants must be used with caution due to the risk of exacerbating blood loss from the large area of tissue disruption during the liposuction procedure.2
- The American Society of Plastic Surgeons recommends that liposuction not be combined with another procedure in the office-based setting. The society also recommends that large volume liposuction procedures (defined as >5L of total aspirate) should not be performed in an office-based setting.4
- Violation of the abdominal or thoracic cavities is possible with any of the methods of liposuction which can result in hemothorax, pneumothorax, hemoperitoneum, or pneumoperitoneum.2
- The serum threshold for local anesthetic toxicity is not explicitly defined but exists in the range of 6-10 mcg/mL. Total lidocaine doses ranging from 35 to 55 mg/kg have been shown to produce peak plasma levels less than 5 ug/mL in patients not taking medications impacting the CYP450 3A4 system responsible for metabolism of lidocaine.1
- The peak plasma concentration of local anesthetic following tumescent liposuction occurs 12-14 hours after the procedure. The late peak is due to the lipophilic nature of lidocaine, epinephrine-induced vasoconstriction, and the low vascularity of adipose tissue.1
- Sites where tumescent liposuction is performed must have medications (e.g., lipid emulsion) and equipment to treat LAST.
- Sedation and anesthetics can mask the signs and symptoms of LAST.
- Tumescent liposuction should not be combined with other uses of local anesthetics such as local infiltration, peripheral nerve blocks, or neuraxial analgesia.
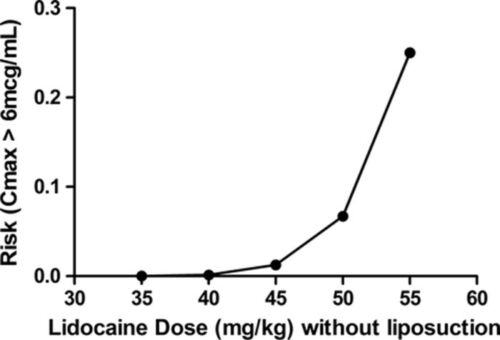
Figure 3. Graph of the risk of achieving toxic levels of lidocaine in the blood following subcutaneous injection of tumescent fluid containing lidocaine without subsequent liposuction. Used with permission from Weinberg G. Local anesthetic systemic toxicity and liposuction. Anesth Analg. 2016.5
- Lidocaine is metabolized in the liver via the cytochrome P450 3A4 enzymes. Other medications metabolized by these enzymes may inhibit the metabolism of lidocaine resulting in systemic toxicity.
- Notable CYP 450 3A4 inhibitors: Some antibiotics, fentanyl, antihypertensives (such as losartan, amlodipine, verapamil), antidepressants, benzodiazepines, statins1,4
References
- Lozinski A, Huq NS. Tumescent Liposuction. Clin Plast Surg. 2013; 40:593-613. PubMed
- Jaffe RA, Schmiesing CA, Golianu B. Liposuction. In: Anesthesiologist's Manual of Surgical Procedures. Philadelphia: Wolters Kluwer; 2020.
- Pardo M, Miller RD, Stoelting RK. Local anesthetics. In: Miller's Basics of Anesthesia. Eighth Edition ed. Philadelphia, PA: Elsevier; 2023:143-159.
- Shapiro FE, Punwani N, Rosenberg NM, et al. Office-based anesthesia: safety and outcomes. Anesth Analg. 2014;119(2):276-85. PubMed
- Weinberg G. Local anesthetic systemic toxicity and liposuction. Anesth Analg. 2016;122(5):1250-2. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.