Copy link
Airway Foreign Bodies in Children
Last updated: 01/03/2023
Key Points
- Foreign body (FB) aspiration is a potentially life-threatening event in young children.
- A detailed history and physical examination and a high index of clinical suspicion is critical to diagnose FB aspiration.
- Both spontaneous and controlled ventilation techniques can be used during bronchoscopy for removal of airway FBs.
- Maintaining an adequate depth of general anesthesia during airway FB removal is essential to avoid coughing and possible dislodgment of the FB.
Introduction
- FB aspiration is a leading cause of death in children younger than three years old.1,2 Approximately 80% of pediatric FB aspirations occur in children younger than three years old, with a peak incidence between one and two years old.
- Several factors predispose children in this age group to FB aspiration.1 They tend to put objects in their mouth and their molars are not well developed to chew food properly. They also have immature swallowing coordination and are easily distracted when eating.
- Food products such as nuts (especially peanuts), seeds (commonly sunflower and watermelon seeds), and popcorn are the most aspirated FBs in infants and toddlers.1,2 Nonfood items such as small toys, coins, paper clips, pins and pen caps are more commonly aspirated by older children.1 Toy balloons and inflated gloves or condoms are the most common objects in fatal childhood FB aspiration.
- FBs that are round are more likely to cause complete airway obstruction. In addition, noncompressible objects that don’t break apart easily and have smooth slippery surfaces are more dangerous.
- Aspirated food products and vegetable substances expand with moisture and may fragment into small pieces.
- Similarly, aspirated oily substances such as nuts can cause chemical pneumonitis. Also, sharp objects may cause trauma to the airway.
- Most aspirated FBs lodge in the bronchial tree, and right-sided lodgment is more common.2
Clinical Presentation
- The clinical presentation depends upon several factors including the degree of airway obstruction, location of the FB, age of the child, characteristics of FB (i.e., size and composition), and elapsed time since the aspiration event.
- A history of a witnessed choking event is highly suggestive for FB aspiration.
- Common presenting symptoms include cough, dyspnea, wheezing, cyanosis, and stridor. While cough is very sensitive for FB aspiration, it is not very specific. Meanwhile, cyanosis or stridor are very specific, but not sensitive for FB aspiration.2
- Physical examination may be normal or reveal decreased breath sounds on one side, wheezing (either focal or generalized), and crackles.
- Signs and symptoms of a delayed presentation include fever, persistent cough or wheezing, recurrent pneumonia, etc.1,2
Diagnosis
- A detailed history and physical examination, and a high index of clinical suspicion is critical to diagnose FB aspiration in children.
- A chest x-ray is commonly used to confirm the diagnosis and identify the location of a radio-opaque FB. Since most aspirated FBs are organic in nature, they are unlikely to be visualized on a chest x-ray. Common radiographic abnormalities include localized emphysema and air trapping, atelectasis, infiltrates, and mediastinal shift (Figure 1). However, a “normal” chest x-ray does not rule out FB aspiration.

Figure 1. Chest x-ray of a two-year-old boy after a witnessed choking episode showing hyperinflation of the left lung and mediastinal shift to the right. Image courtesy of Jeremy Prager, MD, Children’s Hospital Colorado, Aurora, CO.
- Four types of bronchial obstruction related to FB aspiration have been described (Figure 2).3
-
- Bypass valve: The FB causes partial airway obstruction but allows aeration during inspiration and expiration. This is typically seen with small or flat FBs, and no radiographic abnormality is noted.
- Check valve: The FB allows air entry during inspiration, but not during expiration. This results in unilateral hyperinflation of the lungs and mediastinal shift to the opposite side.
- Ball valve: The FB is dislodged by the passage of air during exhalation and reimpacts during inhalation. This results in decreased air entry and mediastinal shift to the affected side.
- Stop valve: The FB causes complete bronchial obstruction with impeded air entry on both inhalation and exhalation. This results in consolidation of the distal bronchopulmonary segment with subsequent collapse.
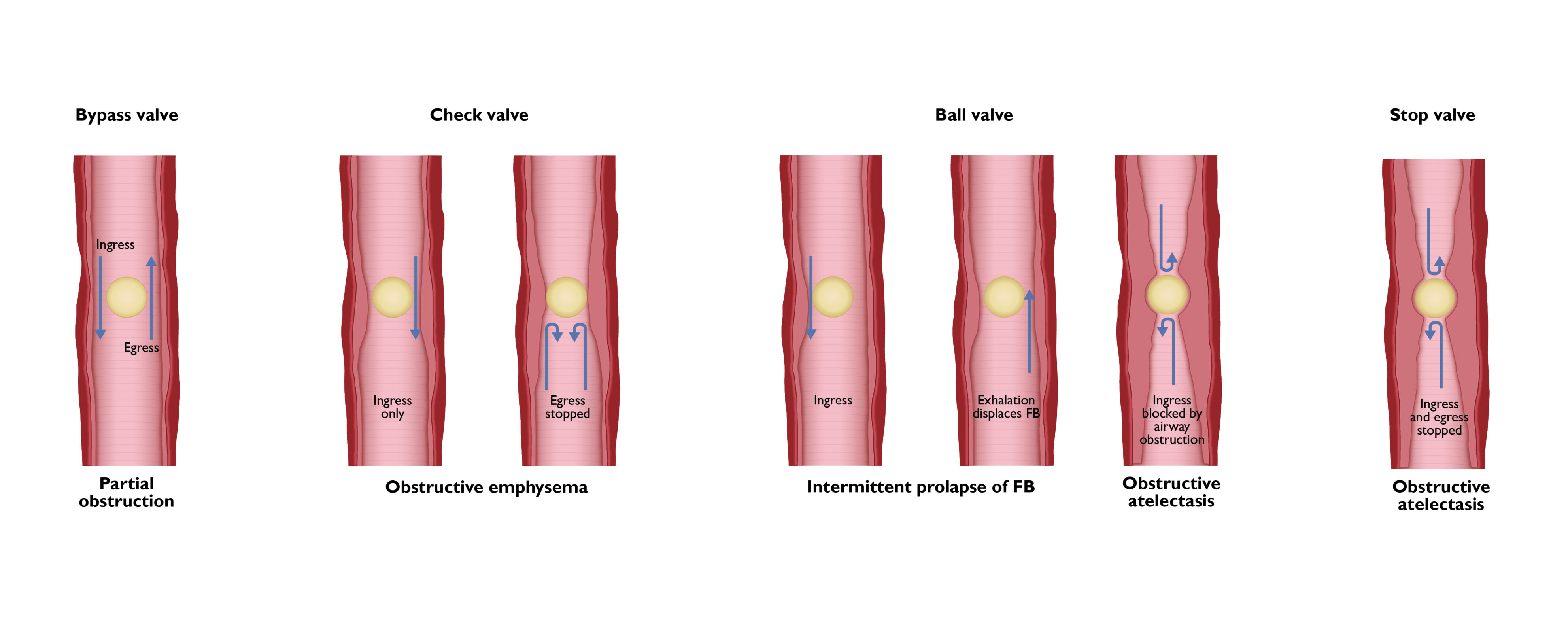
Figure 2. Types of bronchial obstruction with airway FBs.
- Neck x-rays are commonly used to look for upper aerodigestive FBs. The alignment of flat FBs may offer a clue. Tracheal FBs tend to align in the sagittal plane, whereas esophageal FBs tend to align in the coronal plane.2 Lateral x-rays may show soft tissue swelling and loss of cervical lordosis.
- Chest computed tomography (CT) and a virtual bronchoscopy can also be performed to evaluate airway FBs. During a virtual bronchoscopy, reformatted 3-dimensional CT images are used to generate intraluminal views of the lower airways (up to sixth and seventh generation bronchi).2 However, its routine use is limited by patient cooperation, increased costs, limited availability, and radiation exposure.2
Management
- The management goal for tracheobronchial FBs is removal of the FB and the urgency is dictated by the clinical presentation. The procedure of choice is rigid bronchoscopy because it allows control of the airway, visualization, and manipulation of the FB.
- The use of flexible bronchoscopy to diagnose and remove airway FBs has also been reported.2 Rarely, a thoracotomy may be necessary if the FB cannot be removed by rigid or flexible bronchoscopy.
Preanesthetic Evaluation/Preparation
- A detailed history of the onset and severity of symptoms, prior anesthetics, and other comorbidities must be reviewed.
- The patient’s nil per os (NPO) status must be solicited. Most cases are urgent, and the risks of delayed removal outweigh the risks of aspiration. If the patient has a full stomach, an orogastric tube may be inserted after the induction of general anesthesia prior to bronchoscopy.
- Physical examination includes evaluating the general appearance of the child (work of breathing, respiratory rate, etc.,), an airway assessment, and lung auscultation for symmetry of breath sounds and wheezing.
- Diagnostic imaging studies and other laboratory tests (if indicated) must be reviewed.
- The surgical plan and ventilation technique must be discussed with the otolaryngologist. A rigid bronchoscope should be set up and ready to use before the induction of anesthesia.
- Most patients have an intravenous (IV) catheter in situ prior to the induction of anesthesia. Clinical judgement must be used for placing a preoperative IV in an anxious child or administering sedative premedications.1
Intraoperative Management
- After adequate preoxygenation with 100% oxygen, either an inhalational or IV induction may be performed. Standard American Society of Anesthesiologists monitors must be used, and adequate IV access must be obtained.
- Following induction of general anesthesia, direct laryngoscopy is performed, and the airway is topicalized with a local anesthetic (lidocaine 1-2 mg/kg). The OR table is then rotated 90° away from the anesthesiologist. Close communication between the anesthesiologist and surgeon about the status of the airway is critical throughout the procedure. An adequate depth of anesthesia must be ensured before the surgeon begins the procedure. Dexamethasone (0.1- 0.5 mg/kg) IV is typically administered to reduce airway edema.
- The surgeon performs a direct laryngoscopy, and the trachea is intubated with a ventilating bronchoscope. The anesthesia circuit is attached to the side port of the bronchoscope to insufflate oxygen. The bronchoscope is then advanced into the distal airway under direct vision. If necessary, airway secretions are gently suctioned. Once the FB has been visualized, an optical grasping forceps is inserted, and the FB is grasped. Every attempt is made to remove the FB in one piece. After the FB has been successfully removed, a follow-up bronchoscopy is performed to rule out the presence of additional FBs. The patient is then allowed to emerge from anesthesia with a natural airway or after endotracheal intubation.
- One of the most critical moments during the FB removal is the passage through the laryngeal inlet. If the FB is accidentally dislodged in the subglottic region, it may cause complete airway obstruction. In that case, it must be pushed distally from the trachea to a main stem bronchus to allow ventilation of the opposite lung.
- There are two broad approaches to the mode of ventilation-spontaneous vs. controlled ventilation.1,2, 4 The choice between the two depends on the personal preference of the anesthesiologist and surgeon. A review of 94 cases of pediatric airway FB removal showed no difference in the side effects related to either spontaneous or controlled ventilation.4 A spontaneous ventilation technique is more commonly used.2 The advantages and disadvantages of both techniques are listed below (Table 1).
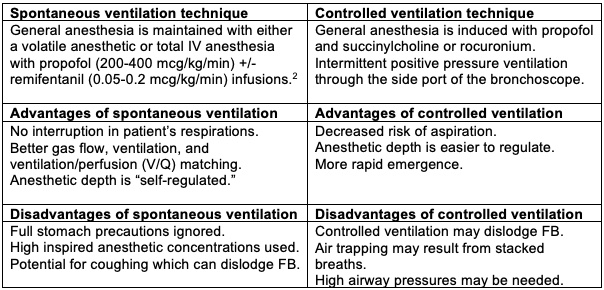
Table 1. Spontaneous vs. controlled ventilation during rigid bronchoscopy for removal of airway FBs in children.
Postoperative Care
- Early discharge (within 4 hours) following an uncomplicated bronchoscopy has been reported.2 Some patients are admitted overnight for observation.
- Predictors of prolonged recovery include the presence of airway inflammation on preoperative chest x-ray, a prolonged duration of bronchoscopy, and aggravation of pulmonary lesions on postoperative films.2
Complications
- Potential intraoperative complications include hypoxia, hypercarbia, bradycardia, hypotension, and the need for supplemental oxygen.4
- Major complications that have been reported include2
- severe laryngeal edema or bronchospasm requiring tracheostomy or reintubation;
- pneumothorax or pneumomediastinum;
- cardiac arrest;
- hypoxic brain damage; and
- tracheal or bronchial laceration requiring repair.
References
- Zur KB, Litman RS. Pediatric airway foreign body retrieval: surgical and anesthetic perspectives. Pediatr Anaesth. 2009:19(1): 109-17. PubMed
- Fidkowski CW, Zheng H, Firth PG. The anesthetic considerations of tracheobronchial foreign bodies in children: a literature review of 12,979 cases. Anesth Analg. 2010;111(4): 1016-25. PubMed
- Chatterji S, Chatterji P. The management of foreign bodies in air passages. Anaesthesia. 1972; 27(4): 390-5. PubMed
- Litman RS, Ponnuri J, Trogan I. Anesthesia for tracheal or bronchial foreign body removal in children: an analysis of ninety-four case. Anesth Analg. 2000;91: 1389-91. PubMed
Other References
- Chatterjee D. Airway foreign bodies in children. OpenAnesthesia. Published August 2017. Accessed February 6, 2023. Airway Foreign Bodies
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.