Copy link
Corneal Reflex: Anatomy
Last updated: 05/28/2019
Overview
The corneal reflex plays an important role in the evaluation of a comatose patient particularly in the neurocritical care setting. This brainstem reflex is used for determination of neurological prognosis in cardiac arrest survivors and for the determination of brain death in those with irreversible, catastrophic brain death. The test is ideally performed between the limbus and central cornea while avoiding the central field of vision (See Figure). The test can be performed with a puff of air or water but is most specific with a cotton-tipped swab. The test assesses the integrity of trigeminal nerve (afferent pathway) and the facial nerve (efferent pathway).
Anatomy
Afferent Limb
The afferent pathway of the reflex is via the nasociliary branch of the ophthalmic division (V1) of the trigeminal nerve (CN V). Multiple receptor types are present on the cornea and contribute to the afferent innervation. (1) The afferent pathway is conducted through both the pons and medulla. (1)
Efferent Limb
The efferent pathway of the reflex is via the cranial nerve VII (facial nerve) to the orbicularis oculi muscle. The efferent signal takes two pathways, a rapid conduction through an oligosynaptic arc reflex and a less direct route via descending spinal tract of the trigeminal nerve. While both the V and VII nuclei are within the pons, there is some degree of signal conduction through the medulla. (1,2) A normal response is blinking of both eyes in response to stimuli, blinking of one eye indicates an impaired reflex, and blinking of neither eye indicates an absent reflex. (2)
Triggering Stimuli
The test can be performed with a puff of air or a squirt of water but is most specific with a cotton-tipped swab. In the setting of life-or-death decision-making, escalating stimuli may be necessary, but has not been proven superior in head-to-head studies. The ideal location for application of a stimulus is between the limbus and central cornea. (1)
Anesthetic Considerations
General anesthesia and varying levels of sedation can ablate the corneal reflex in a dose-dependent manner. Some recommend waiting five half-lives from the last administration of anesthetics to determine brain death. (1) The common anesthetic use of the “eyelash reflex” is an approximation of the more precise corneal reflex.(2)
Key Points:
Corneal reflex: afferent = V1 branch of trigeminal nerve, efferent = facial nerve
Steps:
Pain receptors in cornea detect an irritating stimulus
C fibers are activated
Signal travels to cell bodies of C fibers in trigeminal ganglion, then via trigeminal sensory root —-> spinal trigeminal tract—-> spinal trigeminal nucleus of the pars caudalis
Pars caudalis neurons cross midline and branches into two routes
1. Branches to bilateral facial motor nuclei —-> facial nerve —-> through the stylomastoid foramen —-> zygomatic branch of facial nerve —-> orbicularis oculi muscle —-> close bilateral eyelids
2. Ascending anterior trigeminothalamic fibers —-> ventral posteromedial thalamic nucleus —-> recognition of painful stimulus
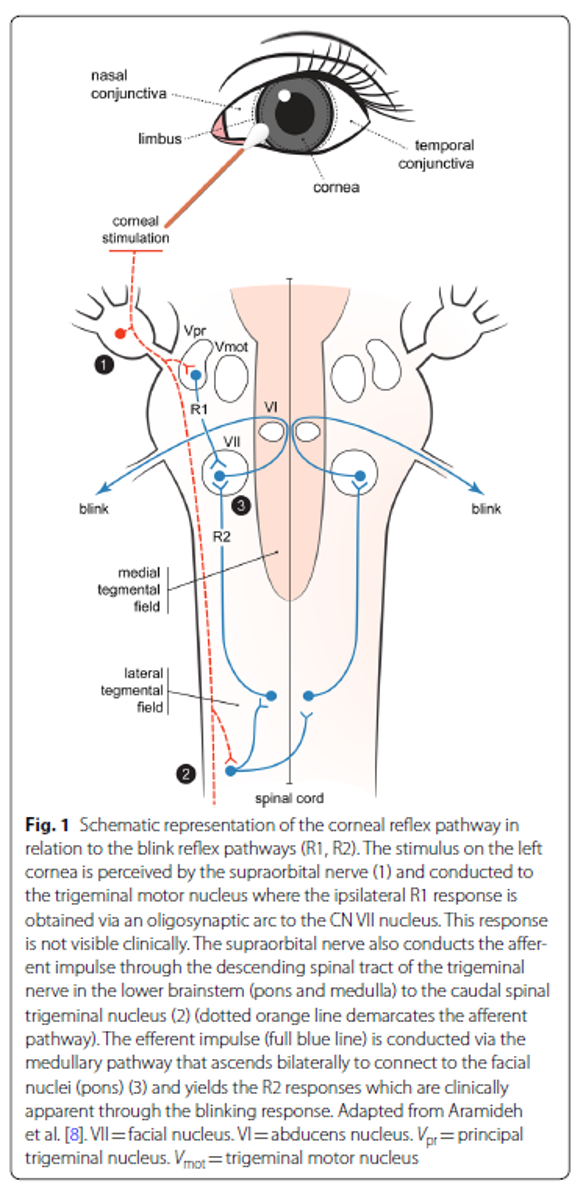
Schematic representation of the corneal reflex pathway: Reprinted by permission from Springer Nature: Neurocritical Care, Corneal Reflex Testing in the Evaluation of a Comatose Patient: An Ode to Precise Semiology and Examination Skills. Maciel CB, Youn TS, Barden MM, et al. Copyright © 2020.
References
- Maciel CB, Youn TS, Barden MM, et al. Corneal Reflex Testing in the Evaluation of a Comatose Patient: An Ode to Precise Semiology and Examination Skills. Neurocrit Care. 2020;33:399-404. doi: 10.1007/s12028-019-00896-0. PubMed Link
- Reshef ER, Schiff ND, Brown EN. A Neurologic Examination for Anesthesiologists: Assessing Arousal Level during Induction, Maintenance, and Emergence. Anesthesiology 2019;130:462–71. DOI: 10.1097/ALN.0000000000002559 PubMed Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.