Copy link
Anesthetic Management of Cesarean Delivery
Last updated: 09/27/2023
Key Points
- Cesarean deliveries may be emergent, urgent, scheduled, or elective depending on maternal and/or fetal indications.
- Anesthetic options include neuraxial and general anesthesia. Surgical local anesthesia or conscious sedation are not standard of care options.
Introduction
- In 2021, 32.1% of live births in the United States were via cesarean delivery (CD)1 which are done for a variety of maternal, placental, anatomic, and fetal indications.
- The anesthesia team must consider the comfort and the safety of the parturient and the fetus when providing anesthesia for CD.
- Anesthesia-related mortality during CD is very rare regardless of anesthetic technique.
- The overall effect on the neonate is likely small regardless of the anesthetic technique.
- Both neuraxial and general anesthesia are safe for parturients but neuraxial anesthesia is more commonly done for CD and is the preferred technique for some of the reasons listed in Table 1.
- CD was associated with 2.7 times the risk of morbidity when compared to vaginal deliveries and is estimated to contribute to 37% of severe maternal morbidity in this population.2
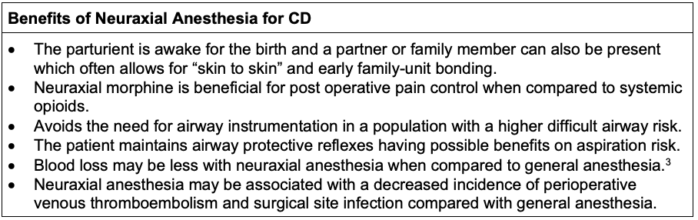
Table 1. Benefits of neuraxial anesthesia for CD;
Abbreviation: CD, cesarean delivery
Indications for CD
- The indications for CD are listed in Table 2.
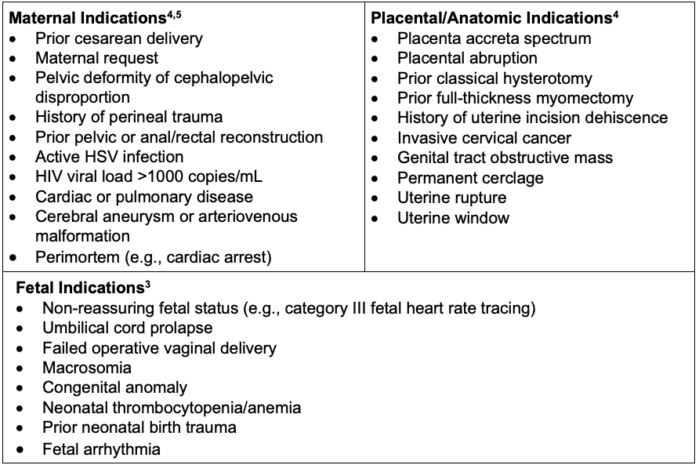
Table 2. Common indications for CD;
Abbreviations: HIV, human immunodeficiency virus, cesarean delivery; HSV, herpes simplex virus
ACOG Classification of CD
- The Royal College of Obstetricians and Gynaecologists (RCOG) classification of CD is listed in Table 3.
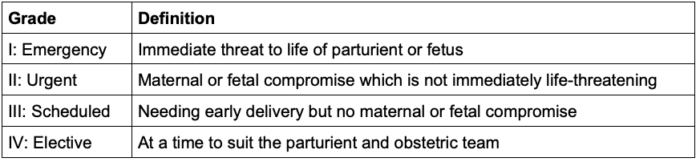
Table 3. RCOG classification of CD
Preoperative Assessment and Preparation
- The American Society of Anesthesiologists (ASA) Practice Guidelines for Obstetric Anesthesia recommends the following.6
- Anesthetic history, past medical history, obstetric history, and allergies should be reviewed, as well as a focused physical exam for nonemergent CD.
- The preoperative assessment for emergency CD should be as comprehensive as time permits.
- Lab testing: complete blood cell count, type and screen are typically drawn. Additional lab testing should be individualized to the patient.
- Standard NPO guidelines should be followed for scheduled and elective cases.7
- Aspiration prophylaxis is almost always innocuous in the absence of contraindications/allergies and recommended for all patients undergoing CD.7 Options for pharmacological prophylaxis include nonparticulate antacids (i.e., sodium citrate-citric acid 30 mL orally), H2 receptor blocker (i.e., famotidine 20 mg IV), proton pump inhibitors (i.e., pantoprazole 40 mg IV), and prokinetic agents (i.e., metoclopramide 10 mg IV).
- Large bore (18g or larger) peripheral intravenous (IV) access is recommended. A second IV should be considered for patients with difficult IV access or who are high risk for hemorrhage.
- Standard ASA monitors should be prepared and available. End-tidal carbon dioxide monitoring is not required during awake neuraxial without sedation but should be readily available and used as indicated.
- Fetal heart rate should be measured and documented prior to CD.
- A narrow spectrum antibiotic should be administered within 60 minutes prior to incision. Cefazolin (2g IV for patients less than 120 kg and 3g IV for patients more than 120 kg) is recommended for CD with intact membranes and absence of labor. In addition to cefazolin, azithromycin 500 mg IV is recommended for CD with ruptured membranes.
CD: Considerations for Neuraxial Anesthesia
- The goal is sensory level coverage from the sacral dermatomes to T4, and this is best tested via a pin prick.
- The most common drugs used for neuraxial anesthesia are a combination of local anesthetic and opioid.
- Hyperbaric bupivacaine 0.75% in 8.25% dextrose is the most common local anesthetic used for a spinal anesthetic. The typical dose of hyperbaric bupivacaine is 11-12 mg when combined with an opioid. The ED95 of intrathecal hyperbaric bupivacaine for CD is 11.2 mg.
- Fentanyl 10-25 mcg is commonly added to spinal anesthetics, as it is lipid soluble and has a synergistic effect with the local anesthetic resulting in improved intraoperative analgesia.
- Intrathecal or epidural morphine is typically given to provide analgesia postoperatively. The typical dose of intrathecal preserve-free morphine for CD is 75-200 mcg and the epidural dose is 1-3 mg.
- Local anesthetics commonly used to obtain surgical analgesia with an epidural catheter include 2% lidocaine and 3% 2-chlorprocaine. With 2% lidocaine and epinephrine (1:200,000), 15-25 mL is injected in 5 mL aliquots and the onset of anesthesia typically occurs in 5-10 minutes. The speed of onset can be increased by the addition of sodium bicarbonate. With 3% 2-chlrorprocaine, the onset of action is typically 8 minutes and can be reduced to 3 minutes with the addition of sodium bicarbonate. Addition of fentanyl (50-100 mcg) should be considered to improve block quality. The duration of action of 2% 3-chlorprocaine is only 40-60 minutes and additional local anesthetic is usually needed.
- A single shot spinal and the combined spinal epidural (CSE) are the most commonly performed neuraxial techniques for CD and can be safely utilized on most patients unless there are contraindications to a neuraxial anesthetic or if the procedure is emergent and therefore there isn’t enough time to safely perform the procedure.
- A few reasons a CSE may be done instead of a single shot spinal for CD are as follows:
- History of multiple CDs or other abdominal surgeries
- Severe patient obesity
- Patient with increased risk of having a complication from general anesthesia, such as a difficult airway, malignant hyperthermia, or aspiration event from a full stomach
- Patients who would benefit from extended neuraxial analgesia such as those with opioid use disorders, chronic pain syndromes, or expected complex or vertical laparotomy
- Alternatively, many patients undergoing a CD are already in labor with an in situ epidural catheter. If time permits, this can safely be utilized for surgical analgesia.
- Common side effects of neuraxial anesthesia are pruritus, nausea, vomiting, shivering, hypotension, and urinary retention.
- Complications of neuraxial anesthesia are the following but not limited to incomplete blockade, blockade failure, postdural puncture headache, high spinal, epidural hematoma, epidural abscess, and local anesthetic systemic toxicity.
CD: Considerations for General Anesthesia
- Common indications for CD under general anesthesia are listed in Table 4.
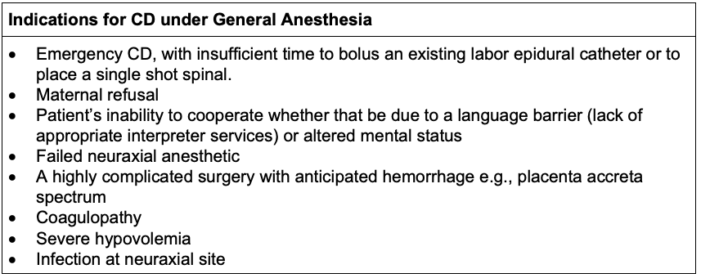
Table 4. Indications for CD under general anesthesia;
Abbreviation: CD, cesarean delivery
- The incidence of a cannot intubate/cannot ventilate scenario is higher among the pregnant patient population.
- Having additional airway equipment such as video laryngoscopy is critical.
- It is critical to be familiar with the difficult airway algorithm. The authors recommend reviewing the Obstetric Anesthetists Association and Difficult Airway Society’s master algorithm for obstetric general anesthesia and failed tracheal intubation. Link
- If a patient has a history of asthma, albuterol, low-dose epinephrine, and other histamine blocking agents should be available in case the patient were to experience bronchospasm.
- If a patient has a hypertensive disorder, the authors recommend having an antihypertensive agent available for induction. Labetalol is most commonly used unless there are allergies or contraindications to this medication.
- Awareness under general anesthesia for CD is not uncommon.8 There are multiple reasons why this may be the case including: underdosing of medications, potentially difficult airway, changes in drug distribution related to the physiologic changes of pregnancy, and a higher incidence of emergencies being the indication for the general anesthetic.
- General anesthesia is usually performed with a rapid sequence induction and intubation. Succinylcholine is most commonly used unless there is a contraindication. Both depolarizing and nondepolarizing muscle relaxants are large and highly ionized molecules, and therefore, do not cross the placenta.
- General anesthesia is typically maintained with a volatile anesthetic, such as sevoflurane until the fetus is delivered. This augments uterine relaxation and facilitates rapid delivery.
- Once the fetus is delivered, the patient is either transitioned over to a total intravenous anesthetic (TIVA) with propofol or a combined nitrous/volatile anesthetic. This is done because volatile anesthetics can markedly contribute to poor uterine tone and possible hemorrhage. The authors recommend converting to TIVA in the absence of contraindications.
- Multimodal analgesia should be utilized for post operative pain control, including acetaminophen and nonsteroidal anti-inflammatory drugs. If long-acting neuraxial opioid was not an option, truncal blocks should be strongly considered. In these cases, the patient should be followed especially closely in the postoperative period and provided oral and/or patient-controlled analgesia IV opioids, as indicated.
Intraoperative Management
- The patient should be positioned in left uterine displacement to minimize the chance of aortocaval compression, regardless of the anesthetic technique.
- Nausea and vomiting are common during a CD and there are a few different etiologies.
- Nausea and vomiting from hypotension is the most common etiology and should be treated with vasopressors, such as phenylephrine and ephedrine. Prophylactic ondansetron may also reduce the incidence of both hypotension and nausea caused by a spinal anesthetic.9
- Uterine exteriorization or replacement may cause nausea and is best treated with a potent IV opioid, such as fentanyl.
- Uterotonic medications can cause nausea. Reducing the rate at which these are administered can help reduce this side effect.
- Intraoperative blood pressures should be maintained within 20 percent of the patient’s baseline blood pressure, except in cases of severe hypertension (e.g., greater than 160 systolic/110 diastolic).
- Blood pressures are commonly maintained either with a phenylephrine infusion or bolus doses of phenylephrine and/or ephedrine. Norepinephrine, epinephrine, and/or vasopressin are rarely required and necessity is based on the individual patient’s underlying pathology (e.g., cardiomyopathy with reduced ejection fraction, pulmonary hypertension).
- Most healthy parturients do not require supplemental oxygen.
- Co-loading 500-1000 mL of crystalloid fluid is common prior to administering neuraxial anesthesia but the patient’s comorbidities must always be assessed prior to doing this.
- It is important to maintain normothermia just as it is in any surgical procedure. It is especially important in patients that have a general anesthetic for their CD or in patients that receive a blood transfusion.
- Uterotonic agents should be administered as indicated and will be covered in a separate summary.
CD: Anesthetic Considerations for Emergencies
- In rare cases, a CD is indicated when either the life of the parturient or the fetus or both are at risk. During these scenarios there may not be enough time to bolus a preexisting epidural catheter or place a neuraxial block.
- Examples of these scenarios are umbilical cord prolapse, uterine rupture, amniotic fluid embolism, cardiac arrest, and category III or terminal fetal heart rate tracing.
- In these scenarios, general endotracheal anesthesia should be performed with the following considerations.
- Administration of aspiration prophylaxis medications
- Obtaining a rapid pertinent history and physical exam focused on the anesthetic and uterotonic contraindications
- Performing a rapid sequence induction
- Utilizing video laryngoscopy to facilitate endotracheal intubation
- Having multiple experienced anesthesia providers at bedside and calling for additional help should always be considered
Enhanced Recovery After CD
- A consensus statement from the Society for Obstetric Anesthesia and Perinatology recommended the following elements for enhanced recovery after CD10 (Table 5).
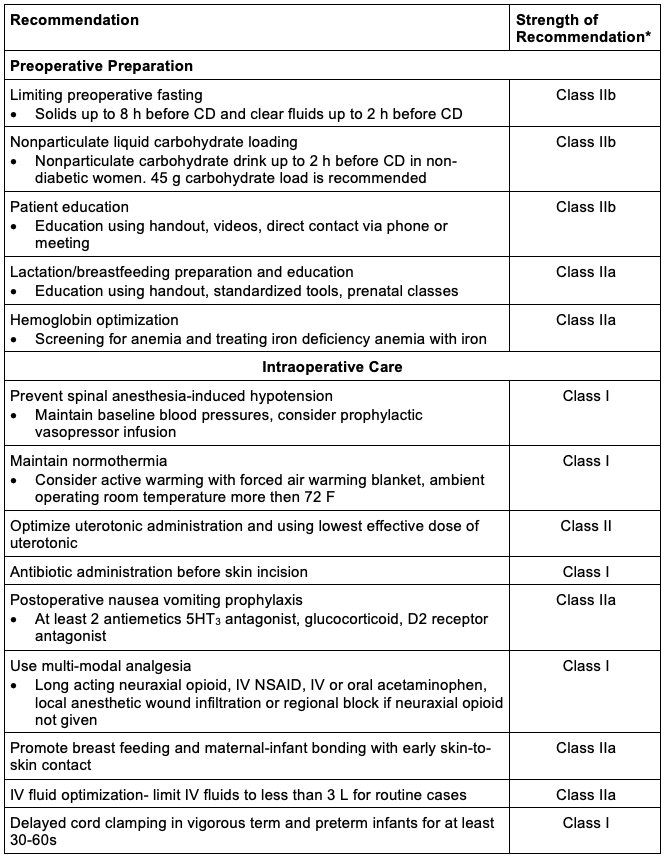
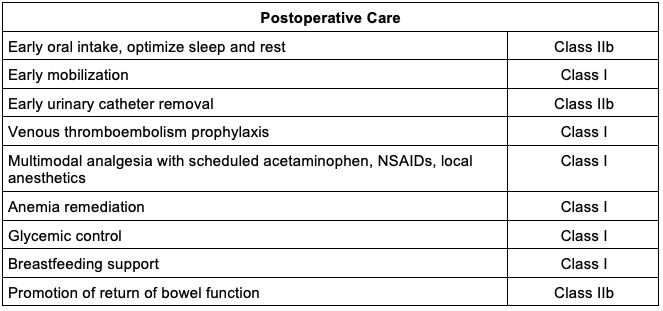
Table 5. Enhanced recovery after CD.
Abbreviations: CD, cesarean delivery; IV, intravenous; NSAID, nonsteroidal anti-inflammatory drug
Adapted from Bollag A, et al. Society for Obstetric Anesthesia and Perinatology: Consensus statement and recommendations for enhanced recovery after cesarean. Anesth Analg. 2021; 132(5): 1362-77.10
*Strength of recommendation: Class I (strong with benefit >>>risk), class IIa (moderate with benefit>>risk), class IIb (weak with benefit ≥ risk), class III (no benefit with benefit = risk).
References
- National Center for Health Statistics, final natality data. www.marchofdimes.org/peristats Updated September 15, 2023. Accessed September 15, 2023. Link
- Leonard SA, Main EK, Carmichael SL. The contribution of maternal characteristics and cesarean delivery to an increasing trend of severe maternal morbidity. BMC Pregnancy Childbirth. 2019; 19(1):16. PubMed
- Heesen M, Hofmann T, Klöhr S, et al. Is general anaesthesia for caesarean section associated with postpartum haemorrhage? Systematic review and meta-analysis. Acta Anaesthesiol Scand. 2013;57(9):1092-102. PubMed
- Barber EL, Lundsberg LS, Belanger K, et al. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118(1):29-38. PubMed
- Kennedy CE, Yeh PT, Pandey S, et al. Elective cesarean section for women living with HIV: a systematic review of risks and benefits. AIDS. 2017;31(11):1579-91. PubMed
- Practice guidelines for obstetric anesthesia: An updated report by the American Society of Anesthesiologists task force on obstetric anesthesia and the Society for Obstetric Anesthesia and Perinatology. Anesthesiology. 2016; 124(2): 270. PubMed
- Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: Application to healthy patients undergoing elective procedures: An updated report by the American Society of Anesthesiologists task force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017;126(3):376-93. PubMed
- Odor PM, Bampoe S, Lucas DN, et al. Pan-London Peri-operative Audit and Research Network (PLAN), for the DREAMY Investigators Group. Incidence of accidental awareness during general anaesthesia in obstetrics: a multicentre, prospective cohort study. Anaesthesia. 2021;76(6):759-76. PubMed
- Gao L, Zheng G, Han J, et al. Effects of prophylactic ondansetron on spinal anesthesia-induced hypotension: a meta-analysis. Int J Obstet Anesth. 2015;24(4):335-43. PubMed
- Bollag A, Lim G, Sultan P, et al. Society for Obstetric Anesthesia and Perinatology: Consensus statement and recommendations for enhanced recovery after cesarean. Anesth Analg. 2021; 132(5): 1362-77. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.