Copy link
Bronchospasm
Last updated: 01/03/2023
Key Points
- Bronchospasm is an acute reversible reflex spasm of the smooth muscle in the bronchioles.
- Bronchospasm is more common among patients with asthma and recent upper respiratory infections within the past 2 weeks.
- Management of bronchospasm includes the administration of oxygen, inhaled bronchodilators, and epinephrine; in severe cases, consider using intravenous medications.
Pathophysiology
- Bronchospasm is the sudden reflexive spasm of the smooth muscle walls of the bronchioles caused by degranulation of mast cell or basophils. An airway with bronchospasm is characterized by contracted smooth muscles, excess mucus, inflammation and swelling of the airways, resulting in decreased airway diameter (Figure 1).
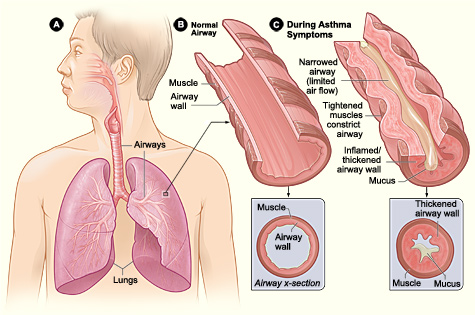
Figure 1. Cross-section of normal airway (left) and airway with bronchospasm (right) (Credit: National Heart, Lung and Blood Institute, National Institutes of Health. CC BY-NC 2.0)
- Acute bronchospasm can lead to progressively worsening increased work of breathing, difficulty with airflow, air-trapping, dynamic hyperinflation, and ventilation-perfusion (V/Q) mismatch.1 In extreme cases, bronchospasm can lead to cardiopulmonary failure requiring extracorporeal life support.
- Signs and symptoms of bronchospasm include wheezing, coughing, and/or increased work of breathing. Signs and symptoms of severe bronchospasm include loss of breath sounds, hypoxia and desaturation, increased airway pressure, and hemodynamic changes including bradycardia and hypotension.
- Bronchospasm produces a “shark fin”-appearing capnography waveform, representing bronchoconstriction (Figure 2).
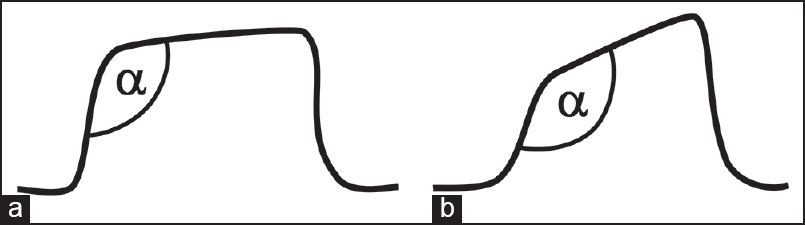
Figure 2. Capnogram of a normal breath (left) and bronchospasm (right) (Kodali BS, Urman RD. J Emerg Trauma Shock. 2014. CC BY-NC-SA 3.0)
Risk Factors
- Risk factors for perioperative bronchospasm can be divided into patient-related and anesthesia-related factors (Table 1).
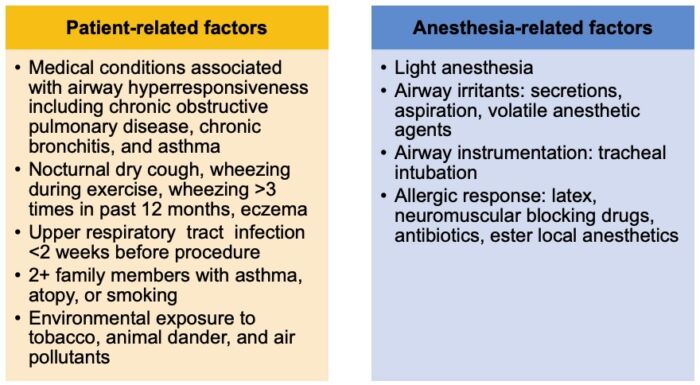
Table 1. Risk factors for bronchospasm. Adapted from Woods BD, Sladen RN. Br J Anaesth. 20091 and von Ungern-Sternberg BS, Boda K, Chambers NA, et al. Lancet. 2010.3
Prevention
Preoperative
- Evaluate for patient-related risk factors.
- Consider supplemental oxygen, inhaled beta-2 agonist (e.g., albuterol), and intravenous steroids if patient is at high risk prior to induction.4
- Consider the use of a supraglottic airway: Use of a supraglottic airway is associated with decreased incidence of bronchospasm compared to an endotracheal tube.1,3,4
Induction
- Consider intravenous induction over inhalational induction.3,4
- Place airway device after adequate depth of anesthesia.1
Emergence
- Suction oropharynx prior to extubation.
- Extubate either fully awake or fully deep.
Management
- The differential diagnosis of bronchospasm includes inadequate depth of anesthesia, endobronchial intubation, mechanical obstruction of endotracheal tube, anaphylaxis, asthma attack, among other etiologies.5
- Management of bronchospasm differs for intubated and nonintubated patients (Table 2).5
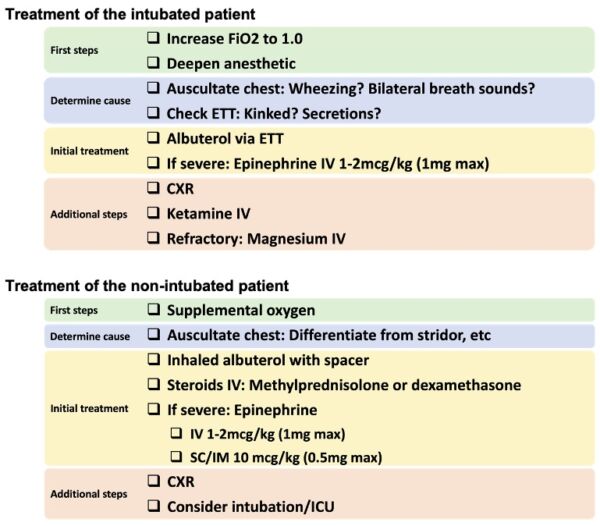
Table 2. Management of bronchospasm. Adapted from Regli A, Becke K, von Ungern-Sternberg BS. Curr Opin Anaesthesiol. 20173 and Society for Pediatric Anesthesia Critical Events Checklists.5
References
- Woods BD, Sladen RN. Perioperative considerations for the patient with asthma and bronchospasm. Br J Anaesth. 2009;103. Suppl 1:i57-i65. PubMed
- Kodali BS, Urman RD. Capnography during cardiopulmonary resuscitation: Current evidence and future directions. J Emerg Trauma Shock. 2014;7(4):332-40. PubMed
- von Ungern-Sternberg BS, Boda K, Chambers NA, et al. Risk assessment for respiratory complications in paediatric anaesthesia: a prospective cohort study. Lancet. 2010; 376(9743) :773-83. PubMed
- Regli A, Becke K, von Ungern-Sternberg BS. An update on the perioperative management of children with upper respiratory tract infections. Curr Opin Anaesthesiol. 2017;30(3):362-67. PubMed
Other References
- Society for Pediatric Anesthesia Critical Events Checklists. Link
- Sinskey JL. Bronchospasm in the Pediatric Patient. OpenAnesthesia. Published November 1, 2021. Accessed February 6, 2023. Bronchospasm in the Pediatric Patient
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.