Copy link
Brain Death or Death by Neurologic Criteria
Last updated: 12/21/2022
Key Points
- Brain death (BD)/death by neurologic criteria (DNC) occurs when there is an irreversible, permanent, and complete loss of brain function.
- BD/DNC is determined clinically in a patient when all the following are confirmed: catastrophic brain injury leading to irreversible loss of all brain function has occurred; confounding conditions have been eliminated; and clinical examination reveals coma, brain stem areflexia, and apnea.
- Neuroimaging and other ancillary testing may support or confirm the clinical diagnosis.
- The presence of drugs that depress the central nervous system, hypothermia, transient postanoxic cranial nerve areflexia, and fulminant Guillain-Barré Syndrome may mimic BD/DNC.
Introduction
- BD or DNC is defined as the irreversible, permanent, and complete loss of whole brain function, including consciousness, brainstem reflexes, and independent respiration.1,2
- BD/DNC is declared in about 2% of all hospital deaths.1
- Determination of BD/DNC is through specific, standardized procedures that should be well documented to ensure the avoidance of false positive determinations.1,2
- Care must be taken to eliminate the possibility of conditions mimicking BD/DNC.1,2
Pathophysiology
- Catastrophic traumatic brain injury or complete cessation of blood flow causes a permanent and complete loss of brain function, leading to neuronal cell death.
- Cessation of blood flow is usually in the setting of uncontrolled elevation in intracranial pressure (ICP) due to prior injury.
- The most common risk factors for BD/DNC include:
- Traumatic brain injury
- Anoxic brain injury
- Ischemic stroke
- Hemorrhagic stroke
- Loss of brain function has several systemic effects.3
- Intracranial hypertension (ICH) causes systemic hypertension, bradycardia, and irregular breathing pattern (Cushing’s response).
- Continued elevation in ICP causes increased sympathetic outflow (sympathetic storm), leading to intense vasoconstriction and tachycardia, which increases myocardial oxygen demand and decreased coronary oxygen delivery. This can lead to myocardial ischemia, dysfunction, and pulmonary edema. Myocardial dysfunction can be seen with ST segment changes, T-wave inversion, or arrhythmias such as atrial fibrillation on electrocardiogram.
- After the initial catecholamine surge, cardiovascular collapse can occur with vasodilation and myocardial dysfunction.
- ICH can also cause neuroendocrine dysfunction with disorders in hypothalamic-pituitary axis:3
- decreased levels of antidiuretic hormone (ADH) leads to central diabetes insipidus-associated hypernatremia and volume depletion;
- impaired cortisol production and release exacerbates hemodynamic instability;
- impaired TSH secretion and decreased conversion of T4 to T3;
- decreased release of insulin leads to hyperglycemia.
- Hypothalamic dysfunction can cause loss of temperature control and hypothermia.
Determination
- The American Academy of Neurology and World Brain Death Project have published the following recommendations for the determination of adult BD/DNC.1,2
- The patient has a clinical history consistent with permanent, catastrophic brain injury.
- There is neuroimaging evidence of increased ICP (severe cerebral edema and brain herniation).
- If an ICP monitor is in place, it should demonstrate elevated ICP that often equals or exceeds the mean
- arterial pressure (MAP).
- If clinical history or neuroimaging is not consistent with possible BD/DNC, conditions mimicking BD/DNC and reversible causes of coma must be ruled out.
- Confounding conditions that make the physical and apnea examinations unreliable must be eliminated prior to the BD/DNC examination.
- Neuromuscular blockade
- Central nervous system depressants
- Severe metabolic, acid/base or electrolyte abnormalities
- Severe hypotension
- Target a systolic blood pressure ≥100 mmHg or a MAP ≥60 mm Hg in adults with the use of volume, vasopressors, and/or inotropes as needed.
- Age-appropriate targets should be used for the pediatric population.
- Hypothermia. Many guidelines or regulations require that the patient should have a minimum core temperature of 36°C.
- Observation period: After progression to BD/DNC is suspected, an observation period should occur to rule out reversible coma. This period may be between 6 and 72 hours. Following hypothermia, longer observation periods may be needed as cranial nerves may have prolonged, temporary areflexia. A minimum of 24 hours is recommended for anoxic brain injury after resuscitated cardiac arrest.
- Clinical examination must reveal unresponsive coma, brain stem areflexia, and apnea despite hypercapnia.
- Unresponsive coma is determined with no response to noxious tactile, verbal, or visual stimuli. Noxious tactile stimuli is given by deep pressure on the condyles at the level of the temporomandibular joints, supraorbital notches, sternum and all 4 extremities. There should be no grimace or facial movement nor motor response to noxious stimuli that is not spinal cord mediated.
- Brain stem areflexia is determined when all of the following are present.
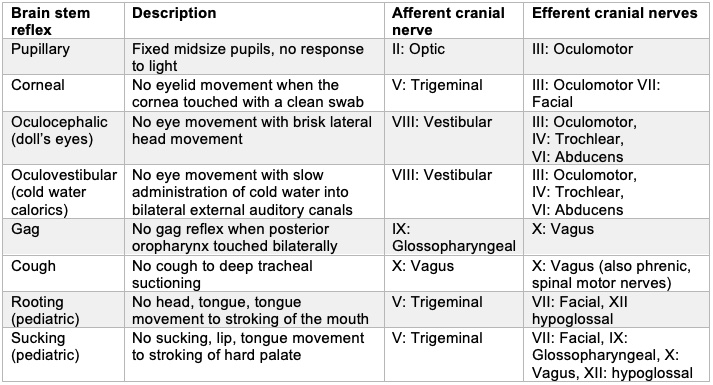
Table 1. Brain Stem Reflex
- Apnea testing is used to determine the inability for respiration despite hypercapnia, which should stimulate the medullary respiratory centers.
- The patient is preoxygenated with 100% O2 for 5 to 10 minutes. The ventilation frequency is then adjusted to achieve eucapnia.
- Mechanical ventilation is paused for the apnea test.
- The patient is oxygenated via cannula with free-flowing oxygen placed in the endotracheal tube (ETT) or with a T-piece and continuous positive airway pressure.
- Arterial blood gas (ABG) is taken at 10 minutes via a single percutaneous puncture or at 6 minutes and every 2-3 minutes from an arterial line. If point-of-care testing is used, the apnea test should continue until the PaCO2 is > 60 mmHg (or 20 mmHg above baseline in patients with chronic respiratory acidosis).
- The patient is monitored continuously for any signs of spontaneous respiratory effort and placed back on mechanical ventilation after the last ABG.
- The test is aborted if the following occur:
- observation of respiratory efforts;
- hemodynamically instability unresponsive to vasopressor titration;
- hypoxia (SpO2 < 85%) for > 30 seconds.
- The apnea test is consistent with BD/DNC if PaCO2 is > 60 mmHg (or 20 mmHg above baseline in chronic respiratory acidosis) and no respiratory efforts occur.
- A single clinical examination, including apnea testing, is the minimum standard for the determination of BD/DNC for adults. If two evaluations are performed, the clinical examinations are often performed by two separate clinicians. Only one positive apnea test should be performed in adults.
Ancillary Studies
- Ancillary tests are needed if a complete cranial nerve exam cannot occur (loss of globe, ruptured ear drum, cervical spine injury), the apnea test cannot be performed due to patient instability, or there is any question of the presence of confounding conditions.
- The World Brain Death Project recommends the following brain blood flow-based methods for ancillary testing to confirm the cessation of cerebral circulation:1
- conventional 4-vessel cranial angiography (digital subtraction angiography) is considered the gold standard for ancillary testing;
- radionuclide studies for brain blood flow;
- transcranial Doppler (TCD). TCD should not be used in pediatrics in absence of validation studies.
- Electroencephalogram (EEG) is no longer recommended as a routine ancillary study.1 Computed tomography angiography and magnetic resonance angiography are not recommended either.
Pediatric Patients1,2
- The definition is the same for adults and children.
- Minimum criteria are the same as adults:
- catastrophic brain injury leading to irreversible loss of all brain function has occurred;
- confounding conditions have been eliminated;
- clinical examination reveals unresponsive coma, brain stem areflexia, and apnea.
- Less evidence is available for the determination of BD/DNC in the very young and caution should be taken.
- If doubt is present, the clinician should err on the side of life.
- Age is at minimum 36-weeks gestation.
- Differences of the pediatric population versus adults:
- Observation period
- 24h in term newborns to 30 days of age
- 12h in infants and children (30 days to 18 years)
- 24h prior to initial testing following birth asphyxia, resuscitation from cardiac arrest and after rewarming from therapeutic hypothermia
- Minimum of 2 examination, including apnea testing
- Clinical criteria should include the absence of sucking and rooting reflexes
- Apnea testing targets are the same
- Ancillary tests
- Indications are the same as adults.
- Tests should be used in patients with chronic hypoxia and apnea should not.
- EEG is considered a valid ancillary study.
- TCD should not be used as it has not been validated in this population.
- Determination should be performed by pediatric clinicians with training and qualifications in pediatric critical care, neonatology, pediatric neurology, pediatric neurointensive care, pediatric neurosurgery or pediatric traumatology.
- Observation period
References
- Greer DM, Shemie SD, Lewis A, et al. Determination of Brain Death/Death by Neurologic Criteria: The World Brain Death Project. JAMA. 2020;324(11):1078-97. PubMed
- Wijdicks EF, Varelas PN, Gronseth GS, et al. Neurology AAo. Evidence-based guideline update: determining brain death in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2010;74(23):1911-8. PubMed
- Smith, M. Physiologic Changes During Brain Stem Death – Lessons for Management of the Organ Donor. J Heart Lung Transplant 2004;23:S217-22. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.