Copy link
Apgar Score
Last updated: 12/13/2022
Key Points
- The components of the Apgar score are appearance, pulse, grimace, activity, and respiration.
- The Apgar scores are performed at 1 and 5 minutes of life. If a newborn infant’s Apgar score at 5 minutes is less than 7, it is repeated every 5 minutes until 20 minutes of life.
- At 5 minutes, an Apgar score of 7-10 is considered reassuring, while scores of 4-5 are moderately abnormal, and scores of 0-3 are low.
- An Apgar score only reflects a newborn infant’s clinical status at one point in time and should not be used to guide neonatal resuscitation or to diagnose asphyxia.
Introduction
- In 1952, Dr. Virginia Apgar, an obstetric anesthesiologist at Columbia University, NY, created the Apgar scoring system to standardize the rapid assessment of newborns in the first minute of life.1,2 Although the Apgar score is commonly thought of as an acronym, it was originally named after Dr. Apgar.
- The Apgar scoring system quantifies the clinical signs of neonatal distress, including bradycardia, pallor, hypotonia, apnea, respiratory depression, and cyanosis.1,2
- The Apgar scoring system is widely used as an assessment tool and is endorsed by the American Academy of Pediatrics and the American College of Obstetrics and Gynecology (ACOG).1,2
Components and Timing
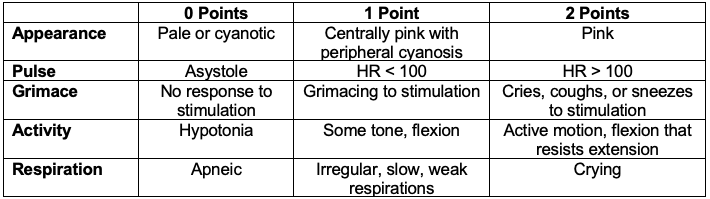
Table 1. Components of the Apgar score. Adapted from Simon LV, Hashmi MF, Bragg BN. Apgar score. In: StatPearls. NIH National Library of Medicine. (Internet). Treasure Island, FL: StatPearls Publishing. 2022.2
Timing
The Apgar scores are performed at 1 and 5 minutes of life. If a newborn infant’s Apgar score at 5 minutes is less than 7, it should be repeated every 5 minutes until 20 minutes of life.1,2
Interpretation of Apgar Scores
- The Apgar score only reflects a newborn infant’s clinical status at one point in time and includes subjective components. It should not be used to guide resuscitative efforts.1
- A low Apgar score at 1 minute does not predict adverse clinical outcomes as it will likely improve by 5 minutes.
- Apgar scores alone should not be used to establish a diagnosis of asphyxia.1
- The ACOG Task Force on Neonatal Encephalopathy defines the 5-minute Apgar score of 0-3 as low and concerning, 4-6 as moderately abnormal, and 7-10 as reassuring.3
- The Apgar score does not predict individual neonatal mortality or neurologic outcomes. Most newborn infants with low Apgar scores do not go on to develop cerebral palsy.1-3 However, based on population studies, Apgar scores less than 5 at 5 and 10 minutes confer an increased relative risk of cerebral palsy in large populations. This increased risk is as high as 20- to 100-fold higher than infants with 5-minute Apgar scores of 7-10.1
- A recent population-based cohort study in Sweden found an increased risk of cerebral palsy and seizures with lower Apgar scores at 5 and 10 minutes.4
- When a newborn infant has an Apgar score of 5 or more at 5 minutes, an umbilical arterial blood sample from a clamped section of the umbilical cord should be obtained, if possible.1
- An Apgar score that remains 0 beyond 10 minutes may be useful in determining if the termination of resuscitation efforts is appropriate, as very few newborn infants with an Apgar score of 0 at 10 minutes survive with normal neurologic outcomes.1,2
Clinical Use and Limitations
- The Apgar score is a rapid method for evaluating a newborn infant after birth at 1 and 5 minutes of life. It evaluates the effectiveness of resuscitation efforts started before the first minute of life.2
- The Apgar score should not be used to determine the initial need for intervention, as the Neonatal Resuscitation Program states that resuscitation efforts must be initiated before the 1-minute Apgar score is assigned.2
- There are several limitations of the Apgar score:1,2
- The Apgar score is a snapshot of the newborn infant’s physiologic condition at one point in time.
- Apgar scores may vary with gestational age, birth weight, congenital anomalies, maternal sedation or general anesthesia, trauma, etc.
- Several components of the Apgar score are subjective and are prone to inter-rater variability.
References
- American Academy of Pediatrics Committee on Fetus and Newborn, et al. The Apgar score. Pediatrics. 2015;136(4): 819-22. PubMed
- Simon LV, Hashmi MF, Bragg BN. Apgar score. In: StatPearls. NIH National Library of Medicine. (Internet). Treasure Island, FL: StatPearls Publishing. 2022. Link
- ACOG. Executive summary: Neonatal Encephalopathy and Neurologic Outcome. 2nd Edition. Obstet Gynecol. 2014; 123(4): 896-901. PubMed
- Persson M, Razaz N, Tedroff K, et al. Five- and 10-minute Apgar scores and risks of cerebral palsy and epilepsy: Population-based cohort study in Sweden. BMJ. 2018: 360: k207. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.